Guiding Principles Help Healthcare Community Address Potential Bias Resulting From Algorithms
Issue Number
894
December 19, 2023
AHRQ Stats
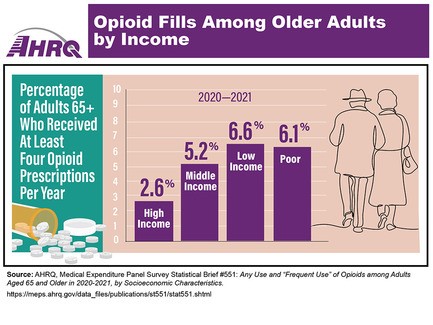
Access more data on this topic in the associated statistical brief, plus additional AHRQ data infographics.
Today's Headlines:
- Guiding Principles Help Healthcare Community Address Potential Bias Resulting From Algorithms.
- Impact of COVID-19 Highlighted in AHRQ Annual Report on Healthcare Quality and Disparities.
- Grantee Applies Human Factors Approach to Healthcare Systems To Improve Safety.
- AHRQ Authors Call for Equity Focus in Learning Health Systems.
- Highlights From AHRQ's Patient Safety Network.
- AHRQ Updates Resource To Reflect Trends in Behavioral Health Integration.
- Explore Careers at AHRQ.
- New Research and Evidence From AHRQ.
- AHRQ in the Professional Literature.
Guiding Principles Help Healthcare Community Address Potential Bias Resulting From Algorithms
A new AHRQ-funded publication in JAMA Network Open addresses the use of algorithms in healthcare, their impact on racial/ethnic disparities in care and approaches to identify and mitigate biases. This work, conducted by a technical expert panel that included AHRQ researchers, provides the healthcare community with guiding principles to avoid repeating errors that have tainted the use of algorithms in other sectors. The use of algorithms is expanding in many realms of healthcare, from diagnostics and treatments to payer systems and business processes. The technical expert panel developed a conceptual framework to apply the guiding principles across an algorithm's life cycle to address the problems of structural racism and discrimination, centering on healthcare equity for patients and communities as the overarching goal. Access the article, AHRQ's press release and more information on AHRQ's work to explore the current use of algorithms in healthcare.
Impact of COVID-19 Highlighted in AHRQ Annual Report on Healthcare Quality and Disparities
AHRQ's 2023 National Healthcare Quality and Disparities Report provides important new insights into the COVID-19 pandemic's impacts on healthcare delivery. Delivered annually to Congress, the report notes that COVID-19 death rates increased between the pandemic's first and second years despite the nation having more knowledge about the disease and greater availability of testing, treatments and vaccines. Uninsured people and people with annual incomes lower than $75,000 were less likely to be recommended for COVID-19 vaccination by healthcare professionals. Additional findings:
- Hospital care: Among middle-age and older adults hospitalized for COVID-19 between March 2020 and March 2022, the median weekly percentage who required ventilator support was more than 10 percent.
- Ambulatory care: About 1 in 6 adults delayed getting medical care due to COVID-19 in 2020. Adults ages 65 and over were most likely to defer medical visits.
- Nursing home care: Between May 2020 and January 2023, the percentage of nursing homes reporting “critical” shortages of nursing staff ranged between 14 percent and 27 percent.
- Telehealthcare: Among Medicare beneficiaries, the number of telehealthcare visits increased 154 percent between March 2019 and March 2020. Telehealthcare visits have decreased since then but remain higher than prepandemic levels.
Access the report, which includes a "Portrait of American Healthcare" that summarizes the nation's capacity to deliver services to the population, as well as Quality and Disparities Tables that provide statistical assessments of healthcare delivery performance in eight areas.
Grantee Applies Human Factors Approach to Healthcare Systems To Improve Safety
AHRQ grantee Rollin J. “Terry” Fairbanks, M.D., M.S., senior vice president and chief quality and safety officer and an emergency physician at MedStar Health in the Baltimore and Washington, D.C., region, is applying a human factors engineering approach to healthcare delivery to reduce patient safety events, particularly in high-risk settings of care. Used in safety-critical industries like aviation, a human factors approach seeks to understand the factors, such as the work environment and technology, that influence peoples' actions, so that systems can be redesigned for optimal safety and overall performance and reliability. Dr. Fairbanks, who is also a professor of emergency medicine at Georgetown University School of Medicine, has used human factors engineering to develop patient safety resources for acute care settings, including a toolkit to help introduce emergency medicine clinical pharmacist programs to hospitals to avoid adverse drug events in emergency department patients. Access Dr. Fairbanks' profile and the profiles of other AHRQ grantees.
AHRQ Authors Call for Equity Focus in Learning Health Systems
A new commentary by AHRQ authors in Healthcare Policy asserts that learning health systems—those in which knowledge generation processes are embedded in daily practice—are uniquely positioned to generate critical real-world evidence needed to advance health equity. Learning health systems, the authors conclude, can help eliminate pervasive inequities by prioritizing health equity; developing partnerships with patients and communities; conducting research to generate evidence on the effectiveness of interventions to improve outcomes across diverse populations; implementing strategies to integrate clinical care, public health and social care; and participating in multisector collaborations to address the social determinants of health. Access the commentary.
Highlights From AHRQ's Patient Safety Network
AHRQ's Patient Safety Network (PSNet) highlights journal articles, books and tools related to patient safety. Articles featured this week include:
- Assessing the clinical, economic, and health resource utilization impacts of prefilled syringes versus conventional medication administration methods: results from a systematic literature review.
- Blackbox error management: how do practices deal with critical incidents in everyday practice? A qualitative interview study.
- Risk-adjusted cumulative sum for early detection of hospitals with excess perioperative mortality.
Review additional new publications in PSNet's current issue or access recent cases and commentaries in AHRQ's WebM&M (Morbidity and Mortality Rounds on the Web).
AHRQ Updates Resource To Reflect Trends in Behavioral Health Integration
Updates to AHRQ's Academy for Integrating Behavior Health and Primary Care lexicon incorporate the latest science and reflect emerging needs on topics such as community engagement, health equity and social determinants of health. The Academy's mission is to promote and support the integration of behavioral health into primary and ambulatory care settings with focuses on providing care for patients using substances, particularly opioids, and for those with mental health conditions. The revised lexicon defines the functions of integrated behavioral health in primary care practices, clarifying what to implement and what to expect on the path to integration.
Explore Careers at AHRQ
Join the team that strives to improve healthcare for all Americans by investing in health systems research, creating strategies to support practice improvement and providing data and analytics to identify opportunities for improvement. Current vacancies include:
- Supervisory Health Scientist Administrator/Division Director, Center for Evidence and Practice Improvement. Application deadline: Dec. 29.
- Program Specialist. Office of Extramural Research, Education, and Priority Populations/Division of Policy Coordination and Analysis. Application deadline: Dec. 29.
- Health Scientist Administrator, Center for Evidence and Practice Improvement/Division of Practice Improvement. Application deadline: Jan. 5.
- Physician, Center for Evidence and Practice Improvement/U.S. Preventive Services Task Force Division. Application deadline: Jan. 5.
- Health Scientist Administrator, Center for Quality Improvement and Patient Safety/Division of General Patient Safety. Application deadline: Jan. 17.
New Research and Evidence From AHRQ
- Systematic review (draft open for comment): Genitourinary Syndrome of Menopause: A Systematic Review.
AHRQ in the Professional Literature
Development of an app for tracking family engagement with early intervention services: focus groups and pilot evaluation study. Wagner L, Corona L, Khan N, et al. JMIR Hum Factors 2023 Sep 12;10:e45957. Access the abstract on PubMed®.
Insurance-based disparities in stroke center access in California: a network science approach. Zachrison KS, Hsia RY, Schwamm LH, et al. Circ Cardiovasc Qual Outcomes 2023 Oct;16(10):e009868. Epub 2023 Sep 25. Access the abstract on PubMed®.
Patient perspectives on seeking emergency care for acute low back pain and access to physical therapy in the emergency department. Kim HS, Strickland KJ, Seitz AL, et al. Ann Emerg Med 2023 Aug;82(2):154-63. Epub 2023 Feb 8. Access the abstract on PubMed®.
Cardiac rehabilitation reduces two-year mortality after coronary artery bypass grafting. Bauer TM, Yaser JM, Daramola T, et al. Ann Thorac Surg 2023 Nov;116(5):1099-1105. Epub 2023 Jun 29. Access the abstract on PubMed®.
Assisted living or nursing home: who is moving in? Wang J, Mao Y, McGarry B, et al. J Am Geriatr Soc 2023 Nov;71(11):3480-8. Epub 2023 Jul 14. Access the abstract on PubMed®.
The Affordable Care Act Medicaid expansion, social disadvantage, and the practice location choices of new general internists. Escarce JJ, Wozniak GD, Tsipas S, et al. Med Care 2022 May;60(5):342-50. Access the abstract on PubMed®.
Reduced compared with traditional schedules for routine antenatal visits: a systematic review. Balk EM, Danilack VA, Bhuma MR, et al. Obstet Gynecol 2023 Jul 1;142(1):8-18. Epub 2023 Jun 7. Access the abstract on PubMed®.
Mechanisms to enhance racial equity in health care: developing a model to facilitate translation of the ACCURE intervention. Griesemer I, Birken SA, Rini C, et al. SSM Qual Res Health 2023 Jun;3:100204. Epub 2022 Dec 2. Access the abstract on PubMed®.



