Learn About CUSP
CUSP Toolkit
Contents
Slide 1. Cover Slide
Slide 2. Learning Objectives
Slide 3. CUSP Supports Kotter's Eight Steps of Change
Slide 4. CUSP Supports Kotter's Eight Steps of Change
Slide 5. CUSP Aligns With and Supports Other Quality and Safety Tools
Slide 6. CUSP is Compatible with TeamSTEPPS
Slide 7. CUSP is Compatible with TeamSTEPPS
Slide 8. Is Your Hospital Safe?
Slide 9. Video
Slide 10. The CUSP Model
Slide 11. A Collaborative Effort
Slide 12. Toolkit Modules
Slide 13. Toolkit Users
Slide 14. Toolkit Users
Slide 15. Implementation
Slide 16. Challenges
Slide 17. Assemble the Team
Slide 18. Barriers to Team Performance
Slide 19. Engage the Senior Executive
Slide 20. The Challenges of Partnering with a Senior Executive
Slide 21. Understand the Science of Safety
Slide 22. System-Level Factors Impact Safety
Slide 23. Identify Defects Through Sensemaking
Slide 24. Examples of Defects or Errors That Affect Patient Safety
Slide 25. Implement Teamwork and Communication
Slide 26. Elements That Affect Communication and Information Exchange
Slide 27. Apply CUSP
Slide 28. The CUSP Model Generates Measurable Results
Slide 29. CUSP Results
Slide 30. Summary
Slide 31. References
Slide 32. References
Note: Slide content is presented below each of the images.
Slide 1. Cover Slide
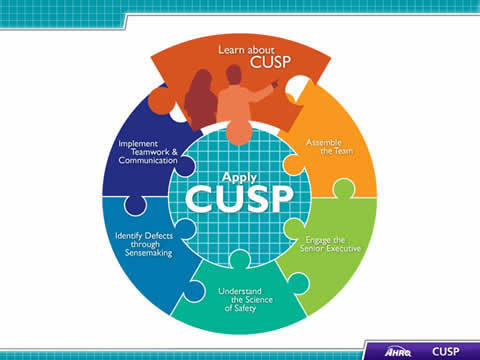
Image: CUSP Toolkit logo.
Slide 2. Learning Objectives
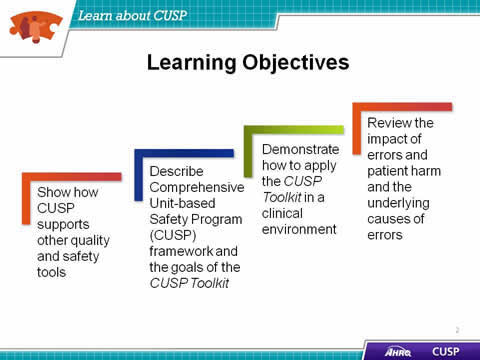
- Show how CUSP supports other quality and safety tools.
- Describe Comprehensive Unit-based Safety Program (CUSP) framework and the goals of the CUSP Toolkit.
- Demonstrate how to apply the CUSP Toolkit in a clinical environment.
- Review the impact of errors and patient harm and the underlying causes of errors.
Slide 3. CUSP Supports Kotter's Eight Steps of Change2
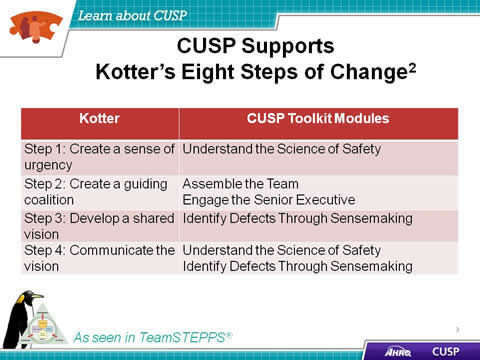
| otter | CUSP Toolkit Modules |
|---|---|
| Step 1: Create a sense of urgency | Understand the Science of Safety |
| Step 2: Create a guiding coalition | Assemble the Team Engage the Senior Executive |
| Step 3: Develop a shared vision | Identify Defects Through Sensemaking |
| Step 4: Communicate the vision | Understand the Science of Safety Identify Defects Through Sensemaking |
Slide 4. CUSP Supports Kotter's Eight Steps of Change2
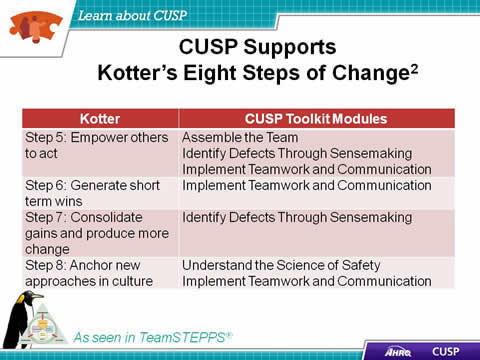
| Kotter | CUSP Toolkit Modules |
|---|---|
| Step 5: Empower others to act | Assemble the Team Identify Defects Through Sensemaking Implement Teamwork and Communication |
| Step 6: Generate short term wins | Implement Teamwork and Communication |
| Step 7: Consolidate gains and produce more change | Identify Defects Through Sensemaking |
| Step 8: Anchor new approaches in culture | Understand the Science of Safety Implement Teamwork and Communication |
Slide 5. CUSP Aligns With and Supports Other Quality and Safety Tools1
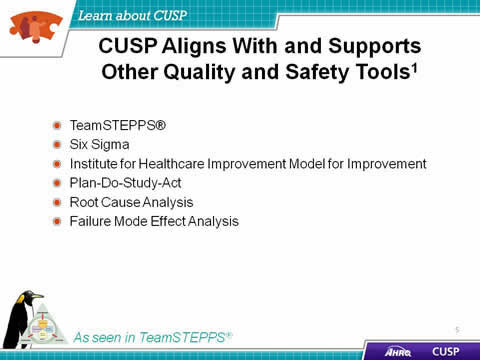
- TeamSTEPPS®.
- Six Sigma.
- Institute for Healthcare Improvement Model for Improvement.
- Plan-Do-Study-Act.
- Root Cause Analysis.
- Failure Mode Effect Analysis.
Slide 6. CUSP is Compatible with TeamSTEPPS3
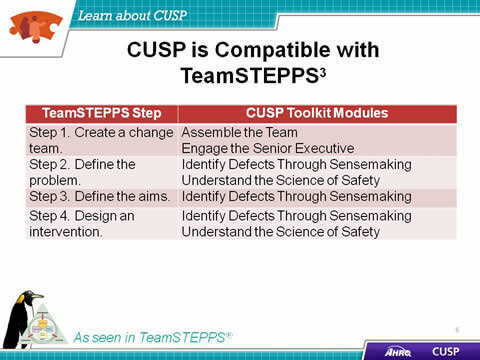
| TeamSTEPPS Step | CUSP Toolkit Modules |
|---|---|
| Step 1. Create a change team. | Assemble the Team Engage the Senior Executive |
| Step 2. Define the problem. | Identify Defects Through Sensemaking Understand the Science of Safety |
| Step 3. Define the aims. | Identify Defects Through Sensemaking |
| Step 4. Design an intervention. | Identify Defects Through Sensemaking Understand the Science of Safety |
Slide 7. CUSP is Compatible with TeamSTEPPS3
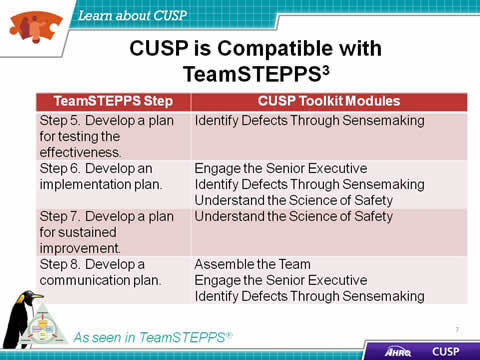
| TeamSTEPPS Step | CUSP Toolkit Modules |
|---|---|
| Step 5. Develop a plan for testing the effectiveness. | Identify Defects Through Sensemaking |
| Step 6. Develop an implementation plan. | Engage the Senior Executive Identify Defects Through Sensemaking Understand the Science of Safety |
| Step 7. Develop a plan for sustained improvement. | Understand the Science of Safety |
| Step 8. Develop a communication plan. | Assemble the Team Engage the Senior Executive Identify Defects Through Sensemaking |
Slide 8. Is Your Hospital Safe?
- Would you want a loved one to be a patient at your hospital? Your unit?
- Would you want to be a patient in the unit where you work?
- Can you say with 100 percent certainty that you believe that your hospital does everything it can to protect its patients?
Slide 9. Video
Slide 10. The CUSP Model
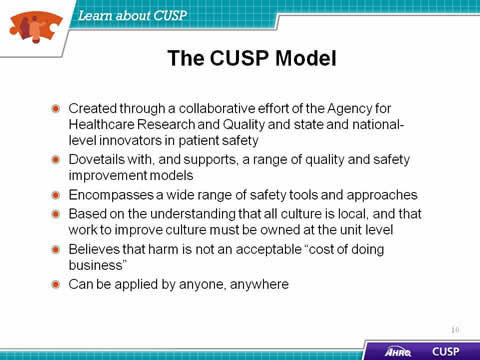
- Created through a collaborative effort of the Agency for Healthcare Research and Quality and state and national-level innovators in patient safety.
- Dovetails with, and supports, a range of quality and safety improvement models.
- Encompasses a wide range of safety tools and approaches.
- Based on the understanding that all culture is local, and that work to improve culture must be owned at the unit level.
- Believes that harm is not an acceptable 'cost of doing business'.
- Can be applied by anyone, anywhere.
Slide 11. A Collaborative Effort4
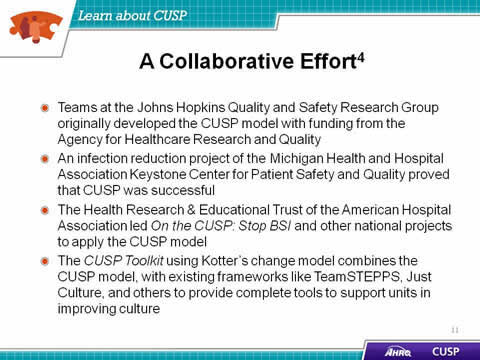
- Teams at the Johns Hopkins Quality and Safety Research Group originally developed the CUSP model with funding from the Agency for Healthcare Research and Quality.
- An infection reduction project of the Michigan Health and Hospital Association Keystone Center for Patient Safety and Quality proved that CUSP was successful.
- The Health Research & Educational Trust of the American Hospital Association led On the CUSP: Stop BSI and other national projects to apply the CUSP model.
- The CUSP Toolkit using Kotter's change model combines the CUSP model, with existing frameworks like TeamSTEPPS, Just Culture, and others to provide complete tools to support units in improving culture.
Slide 12. Toolkit Modules
- Learn About CUSP.
- Assemble the Team.
- Engage the Senior Executive.
- Understand the Science of Safety.
- Identify Defects through Sensemaking.
- Implement Teamwork and Communication.
- Apply CUSP.
Note: After a unit's first implementation of CUSP, modules can be used in any order, depending on the needs of the unit or organization.
Slide 13. Toolkit Users
- Senior executives:
- Help leaders prioritize improvement efforts.
- Provide resources for interventions to alleviate defects.
- Patient safety officers:
- Work with senior executives and managers to maintain an ongoing infrastructure for improvement activities.
- Nurse managers:
- Educate staff on the science of safety.
- Provide opportunities for staff to learn and practice using teamwork and communication tools.
- Work with senior executives and managers to maintain an ongoing infrastructure for improvement activities.
Slide 14. Toolkit Users
- Frontline staff:
- Engage with Stakeholders in safety improvement.
- Physician champions:
- Share knowledge on the immediate and long-term benefits of teamwork and communication tools.
Slide 15. Implementation
- Share videos with teams to spark engagement in staff safety assessments.
- Provide templates and discussion guides to project leads.
- Educate teams on the science of safety.
- Use videos and training modules to orient new clinical staff.
- Train teams in using teamwork and communication tools.
- Engage senior executives and physician champions.
Slide 16. Challenges
- Applicability and usability of CUSP within specialty units (i.e. NICU, oncology).
- Senior executive engagement and participation.
- High staff turnover.
- Nurse empowerment.
Slide 17. Assemble the Team
- Understand the importance of your CUSP team.
- Develop a strategy to build a successful team.
- Identify characteristics of effective teams and barriers to team performance.
- Define roles and responsibilities of team members.
Slide 18. Barriers to Team Performance3
- Inconsistency in team membership.
- Lack of time.
- Lack of information sharing.
- Hierarchy.
- Varying communication styles.
- Presence of conflict.
- Lack of coordination and follow-up.
- Misinterpretation of cues.
- Lack of role clarity.
Slide 19. Engage the Senior Executive
- Identify characteristics to search for when recruiting the senior executive.
- Describe the responsibilities of the senior executive.
- Explain the role of the senior executive in addressing technical and adaptive work.
- Explain how to engage the senior executive and develop shared accountability for the work.
Slide 20. The Challenges of Partnering with a Senior Executive
- May lack clinical background.
- May not recognize the value of CUSP.
- May not be able to meet with the CUSP team regularly.
Slide 21. Understand the Science of Safety
- Describe the historical and contemporary context of the Science of Safety.
- Explain how system design affects system results.
- List the principles of safe design and identify how they apply to technical work and teamwork.
- Indicate how teams make wise decisions when there is diverse and independent input.
Slide 22. System-Level Factors Impact Safety5
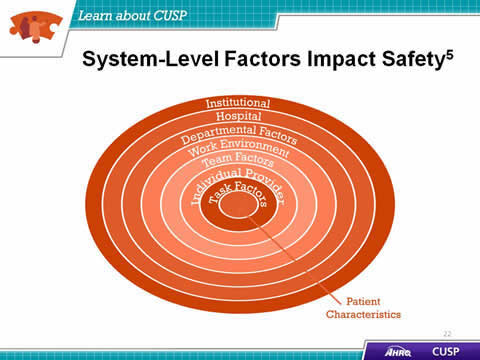
- Institutional.
- Hospital.
- Departmental Factors.
- Work Environment.
- Team Factors.
- Individual Provider.
- Task Factors.
- Patient Characteristics.
Slide 23. Identify Defects Through Sensemaking
- Introduce CUSP and Sensemaking tools to identify defects and errors.
- Discuss the relationship between CUSP and Sensemaking.
- Show how to apply CUSP and Sensemaking tools.
- Discuss how to share findings.
Note: This module combines the CUSP steps Identify Defects and Learn from Defects.
Slide 24. Examples of Defects or Errors That Affect Patient Safety
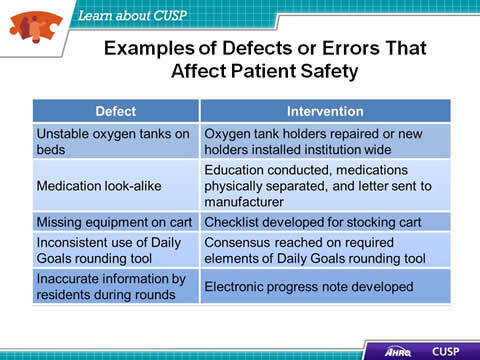
| Defect | Intervention |
|---|---|
| Unstable oxygen tanks on beds | Oxygen tank holders repaired or new holders installed institution wide |
| Medication look-alike | Education conducted, medications physically separated, and letter sent to manufacturer |
| Missing equipment on cart | Checklist developed for stocking cart |
| Inconsistent use of Daily Goals rounding tool | Consensus reached on required elements of Daily Goals rounding tool |
| Inaccurate information by residents during rounds | Electronic progress note developed |
Slide 25. Implement Teamwork and Communication
- Recognize the importance of effective communication.
- Identify barriers to communication.
- Describe the connection between communication and medical error.
- Identify and apply effective communication strategies from CUSP and TeamSTEPPS.
Slide 26. Elements That Affect Communication and Information Exchange
- Interruptions.
- Task absorption.
- Verbal abuse.
- Fatigue.
- Not following plan of care.
- Ambiguous orders or directions.
- Change in team members.
- Work load.
Slide 27. Apply CUSP
- Introduce Just Culture principles.
- Learn how Just Culture principles can augment CUSP.
- Review key steps of the CUSP Toolkit.
A Just Culture system6
- Holds itself accountable.
- Holds staff members accountable.
- Has staff members that hold themselves accountable.
Slide 28. The CUSP Model Generates Measurable Results7
- CUSP in Michigan ICUs:
- Correlated with significant improvements in safety climate in 71 units.
- Overall mean safety climate scores significantly improved from 42.5 percent (2004) to 52.2 percent (2006).
- In 2009, more than 350 hospitals in 22 States reduced CLABSI rates by an average of 35 percent after implementing CUSP.
Slide 29. CUSP Results
- Heightened engagement of staff and senior leaders.
- Improved communication among care team members.
- Shared mental models.
- Expanded knowledge of potential hazards and barriers to safety.
- Collaborative focus on systems of care.
Slide 30. Summary
- CUSP integrates with and supports a broad range of quality and safety models.
- Communication is cited as a root cause of most errors.
- Individuals across an organization can use the CUSP Toolkit and expect measurable results.
Slide 31. References
- Agency for Healthcare Research and Quality, Department of Defense. TeamSTEPPS. Available at http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/index.html.
- Kotter J, Rathgeber H. Our iceberg is melting: Changing and succeeding under any conditions: 1st ed. New York, St. Martin's Press; 2006.
- Agency for Healthcare Research and Quality, Department of Defense. TeamSTEPPS. Available at http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/index.html.
- Health Research and Educational Trust, Johns Hopkins University Quality and Safety Research Group, Michigan Health & Hospital Association Keystone Center for Patient Safety and Quality. Eliminating CLABSI: A national patient safety imperative a progress report on the National On the CUSP: Stop BSI project. Rockville, MD; Agency for Healthcare Research and Quality, April 2011. AHRQ Publication No: 11-0037-EF.
Slide 32. References
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998;316:1154-7.
- Griffith, S. Just Culture. Plano, TX: Outcome Engineering; 2011.
- Pronovost P, Goeschel C, Colantuoni E, et al. Sustaining reductions in catheter related bloodstream infections in Michigan intensive care units: observational study. BMJ 2010;340:c309.




