Patient and Family Engagement
CUSP Toolkit
Slide 1. Cover Slide.
Slide 2. Learning Objectives
Slide 3. The Patient's Hospital Experience1
Slide 4. Patient- and Family-Centered Care3
Slide 5. What is Patient Family Engagement1
Slide 6. Who are Advisors and What do they do?
Slide 7. Characteristics of an Engaged Advisor1
Slide 8. Characteristics of an Engaged Advisor
Slide 9. How To Work With Patient and Family Advisors1
Slide 10. How To Engage Patients and Families1
Slide 11. How To Engage Patients and Families (continued)1
Slide 12. Effective Patient and Family Communication
Slide 13. The Importance of Effective Communication
Slide 14. The Link Between Communication and Patient Safety1
Slide 15. Communication Tips1
Slide 16. IDEAL Discharge Planning
Slide 17. What Is IDEAL Discharge Planning?1
Slide 18. Benefits of IDEAL Discharge Planning for Clinicians1
Slide 19. IDEAL Discharge
Slide 20. What if an Adverse Event Occurs on the Unit?
Slide 21. Engagement Strategies
Slide 22. Introduction to Adverse Events
Slide 23. Immediate Response to an Adverse Event4
Slide 24. Next Steps in Responding to an Adverse Event5
Slide 25. How to Communicate About an Adverse Event6
Slide 26. The Second Victim: Health Care Workers7
Slide 27. Summary
Slide 28. Tools
Slide 29. References
Slide 30. References
Note: Slide content is presented below each of the images.
Slide 1. Cover Slide
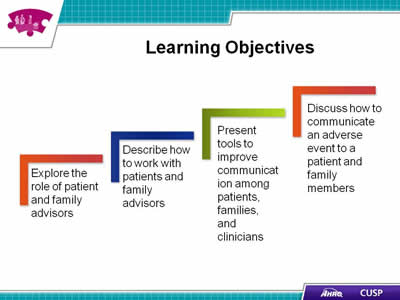
Slide 2. Learning Objectives
- Explore the role of patient advisors.
- Describe how to work with patient and family advisors.
- Present tools to improve communication among patients, families, and clinicians.
- Discuss how to communicate an adverse event to a patient and family members.
Slide 3. The Patient's Hospital Experience1
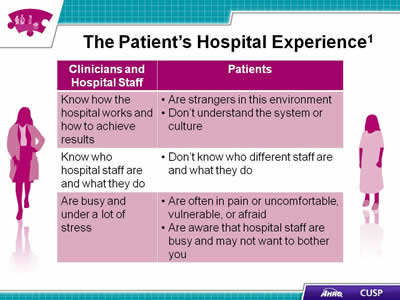
| Clinician and Hospital Staff | Patients |
|---|---|
| Know how the hospital works and how to achieve results |
|
| Know who hospital staff are and what they do |
|
| Are busy and under a lot of stress |
|
Slide 4. Patient and Family-Centered Care3
- Involves “…collaborating with patients and families of all ages, at all levels of care, and in all health care settings … acknowledges that families, however they are defined, are essential to patients’ health and well-being..."
- Core concepts of patient- and family-centered care are:
- Dignity and respect
- Information sharing
- Participation
- Collaboration
Slide 5. What is Patient Family Engagement?1
- Patient and family engagement:
- Is an important component of patient- and family-centered care.
- Creates an environment where patients, families, clinicians, and hospital staff all work together as partners to improve the quality and safety of hospital care.
- Involves patients and family members as:
- Members of the health care team.
- Advisors working with clinicians and leaders to improve policies and procedures.
Slide 6. Who are Advisors and What do they do?
- Advisors are collaborative partners in developing and revising hospital policies, procedures, and practices
- Patients and family members who have received care at our hospital and who want to help improve experiences for others.
- They help our hospital improve quality and safety of care by:
- Giving input and feedback.
- Identifying potential changes and feedback.
- Planning and implementing changes that matter to patients and families.
Slide 7. Characteristics of an Engaged Advisor1
- Listen well.
- Share your views.
- Draw on your communication skills.
- Ask questions.
- Be ready for disagreements.
Slide 8. Characteristics of an Engaged Advisor
(Vignette still). Select to play.
Slide 9. How to Work With Patient and Family Advisors1
- Invite two or three patients and family members to a team meeting to discuss their hospital stay.
- Ask patients and families to give feedback on educational or informational materials.
- Invite patients and families to present at staff orientations and in-service programs.
- Explore the hospital and unit through the eyes of patients and their families by doing a “walk-about” with patients and families.
Slide 10. How To Engage Patients and Families1
- When you enter the room:
- Read chart before stepping in.
- Make eye contact with the patient.
- Introduce yourself by name and role.
- Introduce new people in room by name, role, and what they will do.
- When you first assess the patient:
- Ask how the patient prefers to be addressed.
- Identify family who should be partners in the patient’s care.
- Highlight main points of communication tools.
- Invite the patient and family to use the white board to "talk" with clinicians.
Slide 11. How To Engage Patients and Families1 (continued)
- Ask about and listen to the patient and family’s needs:
- Use open-ended questions.
- Listen to, respect, and act on what the patient and family say.
- Help patients articulate their concerns when needed.
- Get a translator’s assistance if the patient or family member cannot understand you.
- Help the patient and family understand the diagnosis, condition, and next steps:
- Give timely and complete information—take every opportunity to educate the patient and family.
- Use plain language.
- Invite the patient or family to take notes.
Slide 12. Effective Patient and Family Communication
(Vignette still) Select to play.
Slide 13. The Importance of Effective Communication
Slide 14. The Link Between Communication and Patient Safety1

- Patient outcomes.
- Patient safety.
- Perceptions of quality.
Slide 15. Communication Tips1
- Speak slowly.
- Use plain language.
- Reassure the patient and family by giving information.
- Thank patient or family for calling attention to any issue raised.
- Invite them to continue asking questions.
Slide 16. IDEAL Discharge Planning

Slide 17. What Is IDEAL Discharge Planning?1
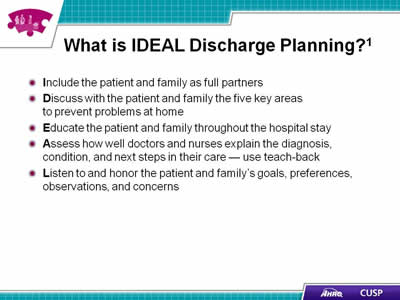
- Include the patient and family as full partners.
- Discuss with the patient and family the five key areas to prevent problems at home.
- Educate the patient and family throughout the hospital stay.
- Assess how well doctors and nurses explain the diagnosis, condition, and next steps in their care—use teach-back.
- Listen to and honor the patient and family's goals, preferences, observations, and concerns.
Slide 18. Benefits of IDEAL Discharge Planning for Clinicians1
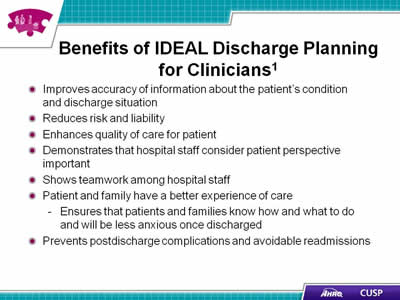
- Improves accuracy of information about the patient's condition and discharge situation.
- Reduces risk and liability.
- Enhances quality of care for patient.
- Demonstrates that hospital staff members consider patient perspective important.
- Shows teamwork among hospital staff.
- Patient and family have a better experience of care:
- Ensures that patients and families know how and what to do and will be less anxious once discharged.
- Prevents postdischarge complications and avoidable readmissions.
Slide 19. IDEAL Discharge
(Vignette still) Select to play.
Slide 20. What if an Adverse Event Occurs on the Unit?
Slide 21. Engagement Strategies
- Engaging in planning and design — Infrastructure advisory
- Engaging in everyday care—How-to strategies
- Engaging after an adverse event.
Slide 22. Introduction to Adverse Events
- Adverse event: An injury to a patient caused by medical intervention rather than by the underlying disease or condition of the patient.
- The mission of health care providers is to help and care for patients without harming them, but adverse events happen.
- When an adverse even occurs, it can be difficult for a health care worker to take ownership and communicate with the patient and family.
- Prompt, compassionate, and honest communication with the patient and family after an adverse event is essential.
Slide 23. Immediate Response to an Adverse Event4
- Care for the patient.
- Report to the appropriate parties.
- Communicate with the patient (who, what, when, where, and why).
- Document the event in the medical record.
Slide 24. Next Steps in Responding to an Adverse Event5
- Investigation.
- Continued communication with the patient and family.
- Apology and remediation.
- System and process improvement.
- Measurement and evaluation.
- Education and training.
Slide 25. How to Communicate About an Adverse Event6
- Speak slowly and use clear language.
- Give an advance alert ("I'm afraid I have some bad news to share with you.")
- Give the news in a few, brief sentences.
- Quietly wait for the reaction.
- Watch and listen for response signals.
Slide 26. The Second Victim: Health Care Workers7
- Health care workers involved in an adverse event experience their own trauma.
- Health care workers should request ongoing support from peers.
- Hospitals have developed Employee Assistance Programs and Medically Induced Trauma Support Services.
Slide 27. Summary
- Advisors provide valuable insight about patient and family experiences and care delivery.
- Effective engagement and communication among patients, family members, and other members of the health care team impacts health outcomes and patient and family satisfaction.
- IDEAL Discharge Planning is an effective tool for ensuring patient and family member engagement and education.
- Organizations should be prepared to respond and communicate proactively when adverse events occur.
Slide 28. Tools
- Am I Ready To Become an Advisor?1
- Working with Advisors1
- Be a Partner in Your Care1
- Get to Know Your Health Care Team1
- Care Transitions from Hospital to Home: IDEAL Discharge Planning1
- SBAR (Situation – Background – Assessment - Recommendation)2
Slide 29. References
- Guide to Patient and Family Engagement in Hospital Quality and Safety. Rockville, MD: Agency for Healthcare Research and Quality; May 2013. AHRQ Publication No. 13-0033
- TeamSTEPPS Instructor Guide. Rockville, MD: Agency for Healthcare Research and Quality; June 2006. AHRQ Publication No. 06-0020.
- Conway J, Johnson B, Edgman-Levitan S, et al. Partnering With Patients and Families To Design a Patient- and Family-Centered Health Care System: A Roadmap for the Future. A work in progress. Bethesda, MD: Institute for Family-Centered Care and Institute for Healthcare Improvement, unpublished manuscript, June 2006.
Slide 30. References
- Bonacum D, Houk C, Moidel BI, et al. Communicating about episodes of harm to patients. In: Leonard M, ed. Achieving Safe and Reliable Healthcare. Chicago: Health Administration Press; 2004. p. 93–112.
- McDonald T, Helmche L, Smith K, et al. Responding to patient safety incidents: the ‘seven pillars.’ Qual SafHealth Care 2010;19:e11.
- Hallenback JL. Palliative Care Perspectives. 1st ed. New York: Oxford University Press 2003.
- Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ. 2000 Mar 18;320(7237):726-727.