Appropriate Assertion (Slide Presentation)
On the CUSP: Stop BSI
Contents
Slide 1. On the CUSP: Stop BSI Assertion
Slide 2. Communication Styles
Slide 3. Aggressive- The Goal is to Dominate and Win!
Slide 4. Passivity- The Goal is to Appease and Avoid Conflict at All Costs!
Slide 5. Assertiveness
Slide 6. Assertion IS
Slide 7. Assertion Includes:
Slide 8. Assertion is Not
Slide 9. Communication to Improve Patient Safety: A Continuous Process
Slide 10. Helpful Hints in Applying The Assertion Model
Slide 11. Improving Assertion
Slide 12. #37: "It is easy for personnel in this ICU to ask questions when there is something that they do not understand."
Slide 13. #26: "In this ICU, it is difficult to speak up if I perceive a problem with patient care."
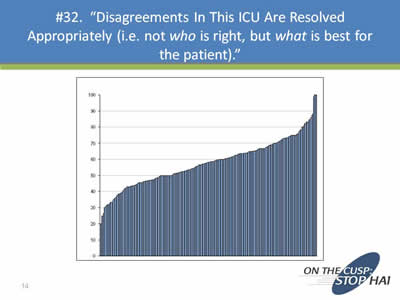
Slide 14. #32: "Disagreements in this ICU are resolved appropriately (i.e. not who is right, but what is best for the patient)."
Slide 15. Discussion
Slide 16. What Next?
Slide 1. On the CUSP: Stop BSI Assertion
David Thompson, DNSc, MS, RN
Jill Marsteller, PhD, MPP
Department of Anesthesiology and Critical Care Medicine
The Johns Hopkins Quality and Safety Research Group
Note: All slides have the logo: On the CUSP: Stop HAI on the bottom right-hand corner.
Slide 2. Communication Styles

- Assertive
- Aggressive
- Passive or Passive Aggressive?
©2004 JHU Quality and Safety Research Group
Slide 3. Aggressive- The Goal is to Dominate and Win!
- This is what I think. What you think does not matter. You are uninformed”
- Often expression of feelings, thoughts in a way that is not wholly truthful
- Usually done in an inappropriate and unprofessional manner
- Body language: Clenched fists, crossed arms, glaring eyes, intrusive on personal space
Slide 4. Passivity- The Goal is to Appease and Avoid Conflict at All Costs!
- Fail to express your thoughts or opinions
- Sarcastic
- Give in with resentment
- Remain silent
- Body language: “The Victim Stance”
Slide 5. Assertiveness
Assertiveness is an attitude and a way of positively relating to those around you; skills set for effective communication.
- See yourself as having worth
- You value others equally, respecting their right to an opinion
- Engage in communication respectfully, while also respecting your own opinions
Slide 6. Assertion IS
Being appropriately assertive means:
- Organized in thought and communication
- Speak clearly and audibly
- Disavowing perfection while looking for clarification and common understanding
- Owned by the entire team (not just a “subordinate” skill-set, and it must be valued by the receiver to work)
Slide 7. Assertion Includes:
- Saying “yes” when indicated, but “no” when you mean “no”
- Using “I” when not speaking for the team
- Respectively defending your position, even if it provokes conflict
- Body language: Secure, upright position in a relaxed manner, making eye contact, standing with open hands
Slide 8. Assertion is Not

- Aggressive
- Hostile
- Confrontational
- Ambiguous
- Demeaning
- Condescending
- Selfish
Slide 9. Communication to Improve Patient Safety: A Continuous Process
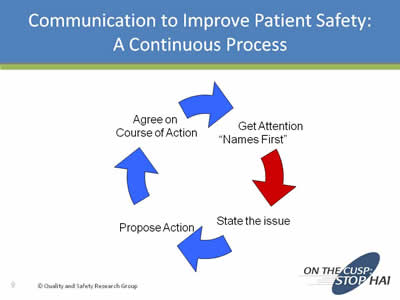
Image of arrows going around in a circle with the following four steps: Get attention "Names first", State the issue, Propose action, and Agree on course of action.
Slide 10. Helpful Hints in Applying The Assertion Model
- Focus on the common goal: Quality care, the welfare of the patient, safety; it’s hard to disagree with safe, high-quality care
- Avoid the issue of who’s right and who’s wrong
- “Patient-centered care”– It is not who is right or who is wrong, it is what is best for the patient
- Depersonalize the conversation
- Actively avoid being perceived as judgmental
- Be hard on the problem, not the people
Slide 11. Improving Assertion
- Names First - get their attention
- Make eye contact
- Express you concern and feelings
- State the issue (clear, concise)
- Propose action(s)
- Re-assert as necessary
- Agree on course of action
- Escalate if no resolution
Note: Image from Slide 10 is shown on the right side of the slide.
Slide 12. #37: "It is easy for personnel in this ICU to ask questions when there is something that they do not understand."
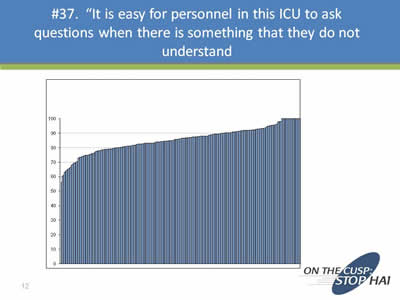
Image of a graph showing a line moving sloping slowly upwards.
Slide 13. #26: "In this ICU, it is difficult to speak up if I perceive a problem with patient care."
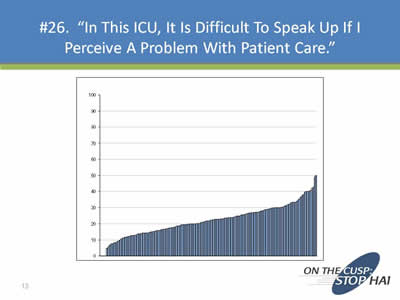
Image of a graph showing a line moving sloping slowly upwards.
Slide 14. #32: "Disagreements in this ICU are resolved appropriately (i.e. not who is right, but what is best for the patient)."
Image of a graph showing a line moving sloping slowly upwards.
Slide 15. Discussion
- Why is it difficult to always be assertive?
- What can you do to assure that your concerns are heard?
- What can we do at the organizational level that will help you succeed at providing safe patient-centered care?
Slide 16. What Next?
- We will build on our assertive training to effectively master conflict resolution strategies
- What are some skill sets we should work on before we begin to address personal and work-related conflict?