CLABSI Investigation: Walk the Process (Slide Presentation)
On the CUSP: Stop BSI
Contents
Slide 1. CLABSI Investigation
Slide 2. Learning Objectives
Slide 3. Infection Rate Above Zero?
Slide 4. Spike in Infections?
Slide 5. Process Auditing
Slide 6. Process Audit: Lessons Learned
Slide 7. Process Audit: Lessons Learned
Slide 8. Standardize
Slide 9. Line Cart Contents - 4 drawers
Slide 10. Process Auditing
Slide 11. Process Audit: Lessons Learned
Slide 12. Process Audit: Lessons Learned
Slide 13. Process Auditing
Slide 14. Infrequent Infections?
Slide 15. Infrequent Infections
Slide 16. Conclusion
Slide 17. References
Slide 18. Thank You
Slide 1. CLABSI Investigation
Melinda Sawyer, RN, MSN, PCCN
David A. Thompson DNSc, MS, RN
Slide 2. Learning Objectives
- Describe the steps to take if your unit’s infection rate is higher than zero
- Describe the “lessons learned” from others who have walked this process
Slide 3. Infection Rate Above Zero?
Or
Were you at zero and then had a spike in your infections?
Slide 4. Spike in Infections?
We suggest walking the process from line placement to maintenance before adding new technologies.
Slide 5. Process Auditing
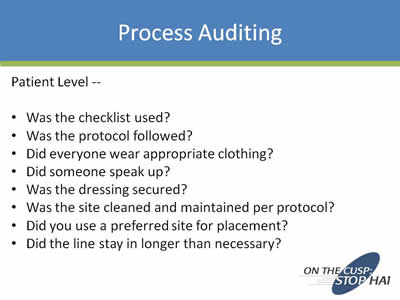
Patient Level --
- Was the checklist used?
- Was the protocol followed?
- Did everyone wear appropriate clothing?
- Did someone speak up?
- Was the dressing secured?
- Was the site cleaned and maintained per protocol?
- Did you use a preferred site for placement?
- Did the line stay in longer than necessary?
Slide 6. Process Audit: Lessons Learned
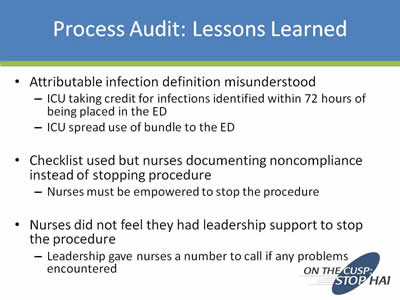
- Attributable infection definition misunderstood:
- ICU taking credit for infections identified within 72 hours of being placed in the ED
- ICU spread use of bundle to the ED
- Checklist used but nurses documenting noncompliance instead of stopping procedure:
- Nurses must be empowered to stop the procedure
- Nurses did not feel they had leadership support to stop the procedure:
- Leadership gave nurses a number to call if any problems encountered
Slide 7. Process Audit: Lessons Learned
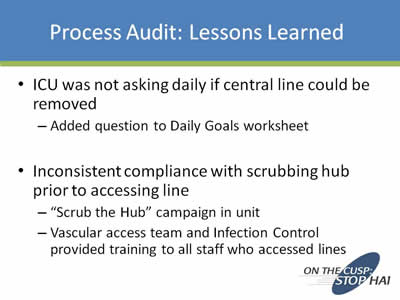
- ICU was not asking daily if central line could be removed
- Added question to Daily Goals worksheet
- Inconsistent compliance with scrubbing hub prior to accessing line
- "Scrub the Hub" campaign in unit
- Vascular access team and Infection Control provided training to all who accessed lines
Slide 8. Standardize

Image of a health professional in a surgical gown and surgical mask.
Slide 9. Line Cart Contents - 4 Drawers
Four images of open drawers in a line cart showing the contents.
Slide 10. Process Auditing
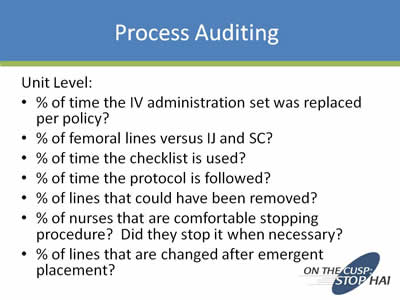
Unit Level:
- % of time the IV administration set was replaced per policy?
- % of femoral lines versus IJ and SC?
- % of time the checklist is used?
- % of time the protocol is followed?
- % of lines that could have been removed?
- % of nurses that are comfortable stopping procedure? Did they stop it when necessary?
- % of lines that are changed after emergent placement?
Slide 11. Process Audit: Lessons Learned
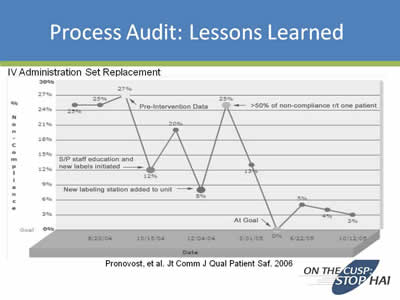
Line chart titled: IV Administration Set Replacement. The chart shows the percent of noncompliance from the time period 8/20/04 to 10/12/05 and the interventions that were taken. Source of the chart is: Pronovost, et al. Jt Comm J Qual Patient Saf. 2006.
Slide 12. Process Audit: Lessons Learned
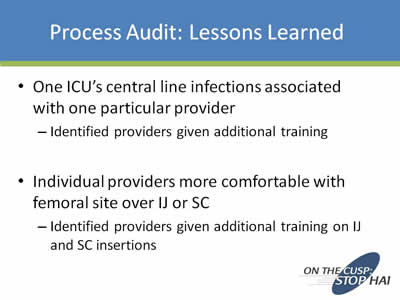
- One ICU's central line infections associated with one particular provider
- Identified providers given additional training
- Individual providers more comfortable with femoral site over IJ or SC
- Identified providers given additional training on IJ and SC insertions
Slide 13. Process Audit: Lessons Learned
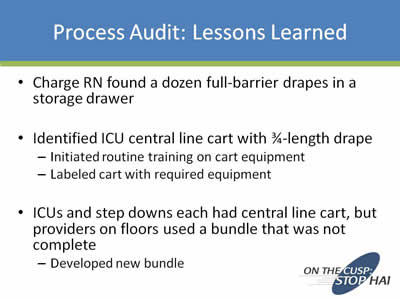
- Charge RN found a dozen full-barrier drapes in a storage drawer
- Identified ICU central line cart with 3/4-length drape
- Initiated routine training on cart equipment
- Labeled cart with required equipment
- ICUs and step downs each had central line cart, but providers on floor used a bundle that was not complete
- Developed new bundle
Slide 14. Infrequent Infections?

Slide 15. Infrequent Infections
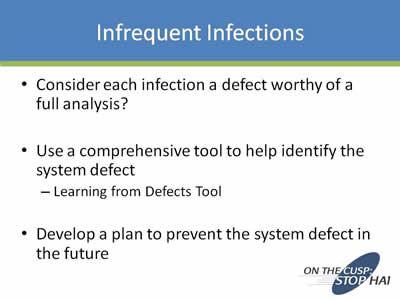
- Consider each infection a defect worthy of analysis?
- Use a comprehensive tool to help identify the system defect
- Learning from Defects Tool
- Develop a plan to prevent the system defect in the future
Slide 16. Conclusion
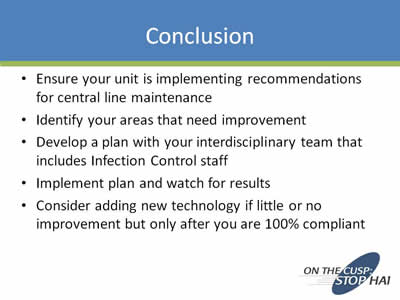
- Ensure your unit is implementing recommendations for central line maintenance
- Identify your areas that need improvement
- Develop a plan with your interdisciplinary team that includes Infection Control staff
- Implement plan and watch for results
- Consider adding new technology if little or no improvement but only after you are 100% compliant
Slide 17. References
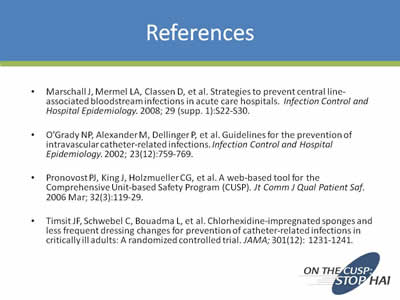
- Marschall J, Mermel LA, Classen D, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals. Infection Control and Hospital Epidemiology. 2008; 29 (supp. 1):S22-S30.
- O’Grady NP, Alexander M, Dellinger P, et al. Guidelines for the prevention of intravascular catheter-related infections. Infection Control and Hospital Epidemiology. 2002; 23(12):759-769.
- Pronovost PJ, King J, Holzmueller CG, et al. A web-based tool for the Comprehensive Unit-based Safety Program (CUSP). Jt Comm J Qual Patient Saf. 2006 Mar; 32(3):119-29.
- Timsit JF, Schwebel C, Bouadma L, et al. Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically ill adults: A randomized controlled trial. JAMA; 301(12): 1231-1241.
Slide 18. Thank You