CUSP: A Framework for Success (Slide Presentation)
On the CUSP: Stop BSI
Contents
Slide 1. CUSP: A Framework for Success
Slide 2. Today's Speakers
Slide 3. Working Together – The Players
Slide 4. Learning Objectives
Slide 5. The Michigan CUSP Experience
Slide 6. It Is Not Just a Simple Checklist
Slide 7. CUSP – The Michigan Experience
Slide 8. ICU Safety Climate
Slide 9. Culture / Climate and Outcomes
Slide 10. ICU Safety Climate
Slide 11. Teamwork Climate & Annual Nurse Turnover
Slide 12. Quote from Man and Superman
Slide 13. The Comprehensive Unit-based Safety Program
Slide 14. Ideas for Ensuring Patients Receive the Interventions: the 4Es
Slide 15. Ensure Patients Reliably Receive Evidence
Slide 16. Measure
Slide 17. What is CUSP?
Slide 18. On the CUSP: Stop BSI Intervention
Slide 19. Translating Evidence into Practice
Slide 20. Safety Score Card Keystone ICU Safety Dashboard
Slide 21. Pre CUSP Work
Slide 22. Steps of CUSP
Slide 23. Step 1: Science of Safety
Slide 24. Step 2: Identify Defects
Slide 25. Prioritize Defects
Slide 26. Step 3: Executive Partnership
Slide 27. Step 4: Learning from Mistakes
Slide 28. Step 4 cont’d: Identify Most Important Contributing Factors
Slide 29. Step 4 cont’d: Identify Most Effective Interventions
Slide 30. Step 4 cont’d: Evaluate Whether Risks Were Reduced
Slide 31. Step 5: Teamwork Tools
Slide 32. Step 5 cont’d: Call List
Slide 33. Step 5 cont’d: Morning Briefing
Slide 34. Step 5 cont’d: Shadowing
Slide 35. CUSP is a Continuous Effort
Slide 36. Action Items -- CUSP
Slide 37. Action Items
Slide 38. References
Slide 39. Photo
Slide 40. CUSP + CAUTI Process and Prevention
Slide 41. Objectives
Slide 42. Science of Safety Education
Slide 43. Project Planning
Slide 44. Project Planning
Slide 45. Project Awareness
Slide 46. Data Collection
Slide 47. Planning Education
Slide 48. Educate on the Evidence
Slide 49. Developing CAUTI Education
Slide 50. CAUTI Education
Slide 51. Urinary Catheter Insertion Competency
Slide 52. Evaluate - Learn from Defects
Slide 53. Execute New Plan
Slide 54. Other Strategies
Slide 55. Outcome = Culture Change
Slide 56. Identify Why Defects - CAUTIs
Slide 57. Execute New Plans
Slide 58. Execute New Plans
Slide 59. CUSP - Not a Linear Process
Slide 60. Polling Questions
Slide 1. National Content Webinar
CUSP: A Framework for Success
March 7, 2012
Slide 2. Today’s Speakers

- Marge Cannon, Medical Officer, CMS.
- Minet Javellana, Health Insurance Specialist, CMS.
- Barb Edson, Vice President of Clinical Quality, HRET.
- Chris George, Director of National Projects, MHA Keystone Center.
- Chris Goeschel, Director of Strategic Development and Research Initiatives at Armstrong Institute for Patient Safety and Quality, John Hopkins University.
- Mary Jo Skiba, Project Manager QI/Research, Alpena Regional Medical Center.
Slide 3. Working Together – The Players

- Centers for Medicare & Medicaid Services Quality Improvement Organization (CMS QIO).
- Agency for Health Care Research and Quality (AHRQ).
- On the CUSP: Stop HAI www.onthecuspstophai.org.
- CLABSI National Project Team Michigan Health & Hospital Association:
- Michigan Keystone Center for Patient Safety & Quality (MHA Keystone).
- Armstrong Institute for Patient Safety and Quality Johns Hopkins University (JHU).
- Health Research & Educational Trust (HRET), research affiliate of the American Hospital Association.
Image: Pieced puzzle in the shape of a square held by a person on each of the four corners.
Slide 4. Learning Objectives
- Understand CUSP impact on safety.
- List CUSP components.
- Describe how a hospital implemented CUSP.
Slide 5. The Michigan CUSP Experience
Chris George, RN MS
Director of National Projects
Michigan Health & Hospital Association
Keystone Center for Patient Safety & Quality
Image: Logo for "Pure Michigan".
Slide 6. It Is Not Just a Simple Checklist
Image of the top of two Annals of Medicine articles: one titled The Checklist; the other titled "The art of medicine: Reality check for checklists".
Slide 7. CUSP – The Michigan Experience
Use of CUSP tied with a technical intervention, such as central line-associated blood stream infection prevention “checklist.”
“Knowing the difference between adaptive and technical challenges is one of the key tasks of leadership.”
Ronald A. Heifetz
Slide 8. ICU Safety Climate
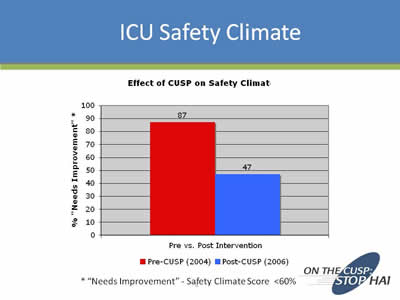
Image: Bar chart showing the "Effect of CUSP on Safety Climate". Results: Pre vs. Post Intervention. Pre-CUSP (2004) shows that 87% of Safety Climate Score needs improvement, while Post-CUSP (2006) drops to 47%.
Slide 9. Culture / Climate and Outcomes
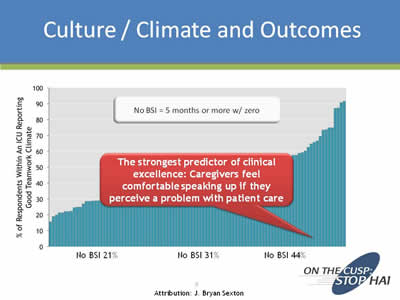
Image: Graph titled "No BSI = 5 months or more w/ zero". Underneath the title is a text box which states "The strongest predictor of clinical excellence: Caregivers feel comfortable speaking up if they perceive a problem with patient care".
Slide 10. ICU Safety Climate
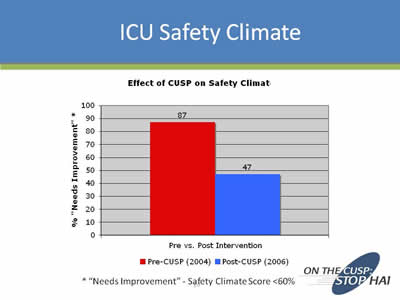
Image: Bar chart showing the "Effect of CUSP on Safety Climate". Results: Pre vs. Post Intervention. Pre-CUSP (2004) shows that 87% of Safety Climate Score needs improvement, while Post-CUSP (2006) drops to 47%.
Slide 11. Teamwork Climate & Annual Nurse Turnover

Chart showing the percentage of teams reporting positive teamwork climate and annual nurse turnover. The first group is labeled High turnover: 16.6%. The second group is labeled Md turnover: 10.8%; and the third group is labeled Low turnover: 7.9%.
Slide 12. Quote from Man and Superman
“The reasonable man adapts himself to the world; the unreasonable one persists in trying to adapt the world to himself. Therefore all progress depends on the unreasonable man.”
Man and Superman
George Bernard Shaw
Slide 13. The Comprehensive Unit-based Safety Program
The Comprehensive Unit-based Safety Program (CUSP): An Intervention to Learn from Mistakes and Improve Safety Culture
Chris Goeschel, ScD MPA MPS RN FAAN
Director, Strategic Development and Research Initiatives at Armstrong Institute for Patient Safety and Quality
Johns Hopkins University
Slide 14. Ideas for Ensuring Patients Receive the Interventions: the 4Es
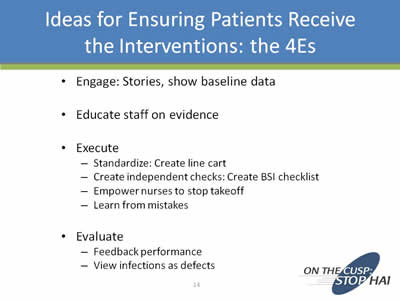
- Engage: Stories, show baseline data.
- Educate staff on evidence.
- Execute:
- Standardize: Create line cart.
- Create independent checks: Create BSI checklist.
- Empower nurses to stop takeoff.
- Learn from mistakes.
- Evaluate:
- Feedback performance.
- View infections as defects.
Slide 15. Ensure Patients Reliably Receive Evidence
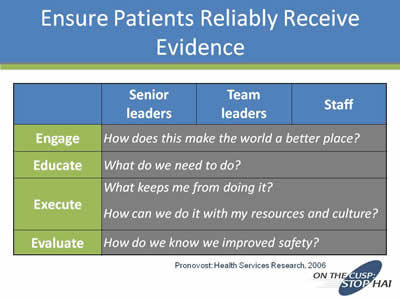
| Senior Leaders | Team Leaders | Staff | |
|---|---|---|---|
| Engage | How does this make the world a better place? | ||
| Educate | What do we need to do? | ||
| Execute | What keeps me from doing it? How can we do it with my resources and culture? | ||
| Evaluate | How do we know we imrpoved safety? | ||
Pronovost: Health Services Research, 2006
Slide 16. Measure
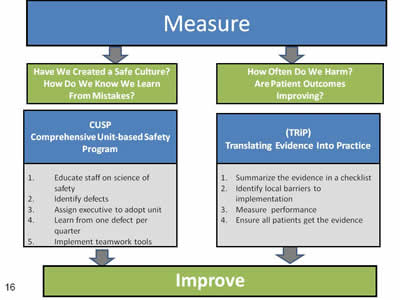
Measure
|
Have We Created a Safe Culture? How Do We Know We Learn From Mistakes?
|
CUSP Comprehensive Unit-based Safety Program
|
1. Educate staff on science of safety
2. Identify defects
3. Assign executive to adopt unit
4. Learn from one defect per quarter
5. Implement teamwork tools
|
Improve
Measure
|
How Often Do We Harm? Are Patient Outcomes Improving?
|
(TRiP) Translating Evidence Into Practice
|
1. Summarize the evidence in a checklist
2. Identify local barriers to implementation
3. Assign executive to adopt unit
4. Measure performance
5. Ensure all patients get the evidence
|
Improve
Slide 17. What is CUSP?
- Comprehensive Unit-based Safety Program.
- An intervention to learn from mistakes and improve safety culture.
Slide 18. On the CUSP: Stop BSI Intervention
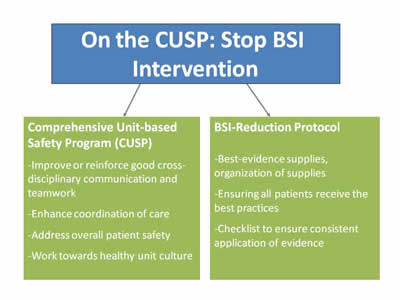
- On the CUSP: Stop BSI Intervention:
- Comprehensive Unit-based Safety Program (CUSP)
- Improve or reinforce good cross-disciplinary communication and teamwork.
- Enhance coordination of care.
- Address overall patient safety.
- Work towards healthy unit culture.
- BSI-Reduction Protocol
- Best-evidence supplies, organization of supplies.
- Ensuring all patients receive the best practices.
- Checklist to ensure consistent application of evidence.
- Comprehensive Unit-based Safety Program (CUSP)
Slide 19. Translating Evidence into Practice

Image of a chart that shows how to translate evidence into practice: Summarize the evidence, identify local barriers implementation, measure performance, and ensure all patients receive the intervention. The source is from the BMJ 2008 article by Pronovost, Berenholtz and Needham.
Slide 20. Safety Score Card Keystone ICU Safety Dashboard
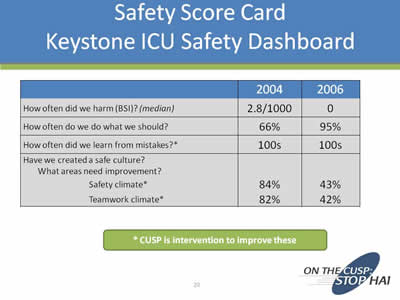
| 2004 | 2006 | |
|---|---|---|
| Engage | 2.8/1000 | 0 |
| Educate | 66% | 95% |
| Execute | 100s | 100s |
|
Have we created a safe culture? Which areas need improvement? Safety Climate*: Teamwork Climate*: |
84% 82% |
43% 42% |
*CUSP intervention to improve these
Slide 21. Pre CUSP Work
- Create a CUSP team:
- Nurses, physician, support staff, infection preventionist.
- Assign a team leader
- Measure culture in the unit.
- Work with hospital quality leader or hospital management to have a senior executive assigned to CUSP team.
Slide 22. Steps of CUSP
- Educate staff on science of safety.
- Identify defects.
- Assign executive to adopt unit.
- Learn from one defect per quarter.
- Implement teamwork tools.
Slide 23. Step 1: Science of Safety
- Understand system determines performance.
- Use strategies to improve system performance:
- Standardize.
- Create independent checks for key process.
- Learn from mistakes.
- Apply strategies to both technical work and teamwork.
- Recognize teams make wise decisions with diverse and independent input.
Slide 24. Step 2: Identify Defects
- Administer the staff safety assessment and ask staff, “How will the next patient be harmed?”
- Review error reports, liability claims, sentinel events, or M and M conference.
Slide 25. Prioritize Defects

- List all defects.
- Discuss with staff what are the three greatest risks and what you should work on first.
Slide 26. Step 3: Executive Partnership
- Executive should become a member of unit team.
- Executive should meet monthly with unit team.
- Executive should:
- Review defects.
- Ensure unit team has resources to reduce risks.
- Hold team accountable for improving risks and central line-associated blood steam infection rate.
Slide 27. Step 4: Learning from Mistakes
- What happened?
- Why did it happen (system lenses)?
- What could you do to reduce risk?
- How do you know risk was reduced?
- Create policy, process, or procedure.
- Ensure staff know policy.
- Evaluate if policy is used correctly.
Slide 28. Step 4 cont’d: Identify Most Important Contributing Factors
- Rate each contributing factor:
- Importance of the problem and contributing factors:
- In causing the accident.
- In future accidents.
- Importance of the problem and contributing factors:
Slide 29. Step 4 cont’d: Identify Most Effective Interventions
- Rate each intervention:
- How well the intervention solves the problem or mitigates the contributing factors for the accident.
- Rate the team belief that the intervention will be implemented and executed as intended.
Slide 30. Step 4 cont’d: Evaluate Whether Risks Were Reduced
- Did you create a policy or procedure?
- Do staff know about the policy?
- Are staff using it as intended?
- Do staff believe risks have been reduced?
Slide 31. Step 5: Teamwork Tools
- Call list.
- Daily goals.
- Morning briefing.
- Shadowing.
- Culture check up.
Slide 32. Step 5 cont’d: Call List
- Ensure your unit has a process to identify which physician to page or call for each patient.
- Make sure call list is easily accessible and updated.
Slide 33. Step 5 cont’d: Call List
- Have a morning meeting with charge nurse and unit attending(s) about the unit-level plan for the day.
- Discuss work for the day:
- What happened during the evening?
- Who is being admitted and discharged today?
- What are potential risks during the day; how can we reduce these risks?
Slide 34. Step 5 cont’d: Shadowing
- Follow another type of clinician doing his or her job for between 2 and 4 hours.
- Have the shadower discuss with staff what he or she will do differently now that he or she has walked in another person’s shoes.
Slide 35. CUSP is a Continuous Effort
- Add science of safety education to orientation.
- Learn from one defect per quarter; share or post lessons.
- Implement teamwork tools that best meet the unit’s needs
- Review details in the CUSP manual.
Slide 36. Action Items -- CUSP
- Look over the CUSP manual with team members.
- Brainstorm potential hazards with team
- Assess team composition with respect to CUSP elements.
- Review pre-implementation checklist — where are you?
Slide 37. Action Items
- Review content of Web site at www.onthecuspstophai.org:
- Toolkits.
- Slidesets.
- Manuals.
- Project Management Checklists:
- Pre-Implementation Checklist.
- CEO/Senior Leader Checklist.
- Infection Preventionist Checklist.
Slide 38. References
- Pronovost P, Weast B, Rosenstein B, et al. Implementing and validating a comprehensive unit-based safety program. J Pat Safety. 2005; 1(1):33-40.
- Pronovost P, Berenholtz S, Dorman T, et al. Improving communication in the ICU using daily goals. J Crit Care. 2003; 18(2):71-75.
- Pronovost PJ, Weast B, Bishop K, et al. Senior executive adopt-a-work unit: A model for safety improvement. Jt Comm J Qual Saf. 2004; 30(2):59-68.
- Thompson DA, Holzmueller CG, Cafeo CL, et al. A morning briefing: Setting the stage for a clinically and operationally good day. Jt Comm J Qual and Saf. 2005; 31(8):476-479.
Slide 39. Photo

Image: Black and white photo of a young child playing in the sand.
Slide 40. CUSP + CAUTI Process and Prevention
Mary Jo Skiba, RN BSN
Project Manager QI/Research
Image of various medical equipment, including an IV bag..
Slide 41. Objectives
- Apply CUSP interventions to CAUTI project.
- Remove barriers/identify steps to successful.
- CAUTI project initiation Use CUSP to maintain success.
Slide 42. Science of Safety Education
- Education done prior to CAUTI.
- Safety survey to identify at-risk departments.
- Mandatory science of safety training.
Slide 43. Project Planning
- CAUTI Team.
- Policies.
- Awareness campaign.
- Data collection plan.
- Project start date.
- Education
- Plan for follow-up.
Images to the right of the text include a photo of stick figures circled around a light bulb and a photo of a construction site with many large cranes.
Slide 44. Project Planning
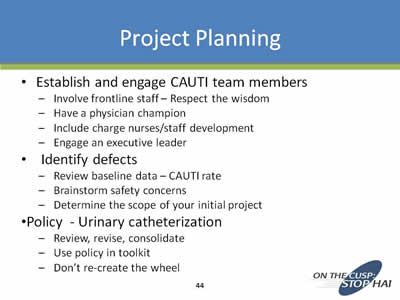
- Establish and engage CAUTI team members:
- Involve frontline staff – Respect the wisdom.
- Have a physician champion Include charge nurses/staff development.
- Engage an executive leader.
- Identify defects:
- Review baseline data – CAUTI rate
- Brainstorm safety concerns.
- Determine the scope of your initial project.
- Policy - Urinary catheterization:
- Review, revise, consolidate.
- Use policy in toolkit.
- Don’t re-create the wheel.
Slide 45. Project Awareness
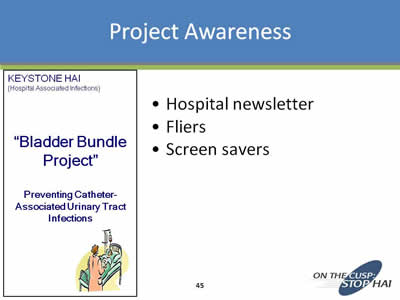
- Hospital newsletter.
- Fliers.
- Screen savers.
Image: Flyer example by KEYSTONE HAI titled "Bladder Bundle Project": Preventing Catheter-Associated Urinary Tract Infections.
Slide 46. Data Collection
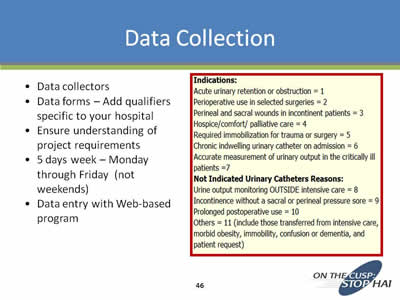
- Data collectors.
- Data forms – Add qualifiers specific to your hospital.
- Ensure understanding of project requirements.
- 5 days week – Monday through Friday (not weekends).
- Data entry with Web-based program.
- Indications:
- Acute urinary retention or obstruction = 1.
- Perioperative use in selected surgeries = 2.
- Perineal and sacral wounds in incontinent patients = 3.
- Hospice/comfort/palliative care = 4.
- Required immobilization for trauma or surgery = 5.
- Chronic indwelling urinary catheter on admittion = 6.
- Accurate measurement of urinary output in the critically ill patients = 7.
- Not Indicated Urinary Catheters Reasons:
- Urine output monitoring OUTSIDE intensive care = 8.
- Incontinence without a sacral or perineal pressure sore = 9.
- Prolonged postoperative use = 10.
- Others = 11 (include those transferred from intensive care, morbid obesity, immobility, confusion of dementia, and patient request).
Slide 47. Planning Education

Identify Defects -- Plan Ahead to Prevent Roadblocks
- Nursing:
- Who will be trained?
- Who will train?
- How will we train?
- When will we train?
- How will we do makeups?
- How much ongoing training or re-training needed?
- Physicians
- Who will train?
- How will we train?
- When will we train?
Slide 48. Educate on the Evidence
- Didactic:
- CAUTI face-to-face inservice.
- All nursing/aide.
- Guideline for prevention of CAUTI.
- Physician CME.
- Department meetings.
- Demonstration of insertion competency.
Slide 49. Developing CAUTI Education
- Don’t re-create the wheel.
- Use other hospitals’ PowerPoint slides.
- Multiple CAUTI toolkits.
- Update/revise to fit.
Slide 50. CAUTI Education
- Trained the trainers.
- Engaged frontline staff.
Image: Flyer that explains how catheter-related infections can occur.
Slide 51. Urinary Catheter Insertion Competency
- Traveling mannequin.
- 100 percent of aides and all nurse frequent inserters (ED, OR, WHU, IP rehab, ICU).
- Read policy.
- Take quiz.
- Perform procedure.
- Instant remediation and repeat demonstration.
Slide 52. Evaluate - Learn from Defects
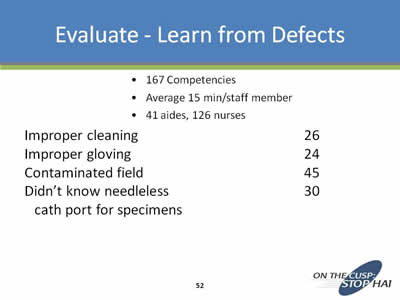
- 167 Competencies.
- Average 15 min/staff member.
- 41 aides, 126 nurses.
Improper cleaning: 26
Improper gloving: 24
Contaminated field: 45
Didn’t know needleless cath port for specimens 30
Slide 53. Execute New Plan
- Improvement plan for competency.
- Require field competency all aides within 2 months, supervised by RNs.
- Newly hired aides trained by RNs.
- Yearly aide hands-on demo of competency.
Slide 54. Other Strategies
- Caths flagged with date of insertion.
- Secured to legs.
- Specimen collection for culture:
- Don’t use first urine drained from catheter ED patients.
- Prior to collection, change catheter unless known change within 7 days Inpatients.
- If catheter in for 7 days must change prior to specimen collection.
- Perineal hygiene prior to cath.
- “John Door” educational posters.
Slide 55. Outcome = Culture Change
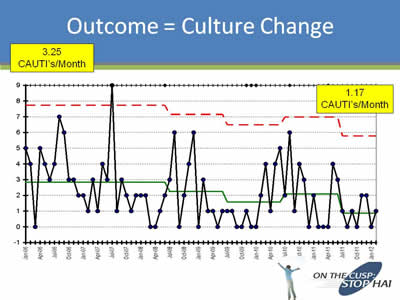
Image: Graph showing that at the start of the initiative there were 3.25 CAUTI's/month and by the end there were 1.7 CAUTI's/month.
Slide 56. Identify Why Defects - (Increased)CAUTIs
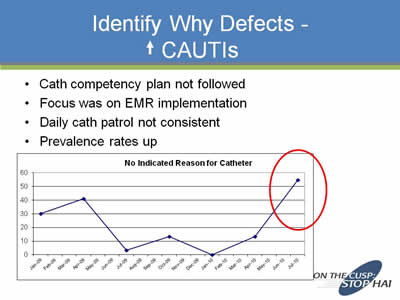
- Cath competency plan not followed.
- Focus was on EMR implementation.
- Daily cath patrol not consistent.
- Prevalence rates up.
Image: Bar graph showing "No Indicated Reason for Catheter" nearly doubling from 30 to 60 from January 2009 to July 2010.
Slide 57. Execute New Plans
- Annual competency aide and ED/OR nurses.
- Imbedded competency orientation/annual skill evaluations.
- Agenda item every leadership/staff meeting.
- Charge nurse daily cath patrol.
- Feedback monthly staff and physicians.
Slide 58. Execute New Plans

- Build cath necessity into EMR.
- Consider decrease size standard cath - #16 to 14.
- ED data capture of cath necessity.
Slide 59. CUSP - Not a Linear Process
“You might have to fight the battle more than once in order to win it.” (Margaret Thatcher)
Don’t worry alone. CUSP is a team sport.
“Shoot for the moon. Even if you miss, you'll land among the stars.” (Les Brown)
Questions?
mjskiba@agh.org
Slide 60. Polling Questions
- Have you ever heard of the Comprehensive Unit-based Safety Program (CUSP) before?
- I have never heard of CUSP
- I have heard of CUSP, but have not implemented it
- I have heard of CUSP, but have not successfully implemented it.
- Have implemented CUSP successfully and actively using it in my unit.
- My senior executive regularly attends safety meetings on my unit, and can identify the top three safety issues that our safety team is currently working on:
- Very rarely attends and is out of touch with our unit safety issues.
- Intermittently attends, and is somewhat aware of our unit safety issues.
- Attends whenever possible, and is aware of our unit’s top three safety issues.
- By ensuring that your senior executive is a part of your safety team, meeting monthly with your unit team, and holding your unit team accountable for improving risks surrounding a hospital inquired condition, my unit will be successfully utilizing the executive partnership component of CUSP?
- No, not at all.
- Not sure.
- Yes, those are the main elements of the executive partnership component of CUSP.



