How CUSP Enables Nurse Empowerment (Slide Presentation)
On the CUSP: Stop BSI
Contents
Slide 1. How CUSP Enables Nurse Empowerment
Slide 2. Presenters (continued)
Slide 3. CUSP Components
Slide 4. How is CUSP Different? It Empowers Nurses
Slide 5. St. Joseph Mercy Hospital's Journey
Slide 6. Best Practices: Learning from Defects Tool
Slide 7. Best Practices: Engaging & Sustaining Nurse Involvement in CUSP Huddles
Slide 8. Components
Slide 9. SICU Huddle Board
Slide 10. Surgical Unit Huddle Board
Slide 11. Lessons for Your Hospital: Strategies That Promote Nurses & Leverage CUSP
Slide 12. A Healthcare Imperative
Slide 13. Joanne Timmel, MSN, RN, NE-BC
Slide 14. Implementing CUSP: Assumptions & Prerequisites
Slide 15. Implementing CUSP: Engaging the TEAM
Slide 16. CUSP: How it Empowers Nurses in the Hospital
Slide 17. CUSP: Example of Empowerment
Slide 18. CUSP: Example of Empowerment
Slide 19. CUSP: Example of Empowerment
Slide 20. Best Practices: Engaging & Sustaining Nurse Involvement in CUSP
Slide 21. Lessons for Your Hospital: Strategies That Promote Nurses with the Leverage of CUSP
Slide 22. Questions?
Slide 1. How CUSP Enables Nurse Empowerment
November 15, 2011
Presenters:
Pat Posa, RN, BSN, MSA
Joanne Timmel, MSN, RN, NE-BC
On top of slide it states: "CLABSI Supplemental Call Series"
Slide 2. Presenters (continued)
Pat Posa, RN, BSN, MSA
System Performance Improvement Leader
St. Joseph Mercy Heath System
On top of slide it states: "CLABSI Supplemental Call Series"
Slide 3. CUSP Components
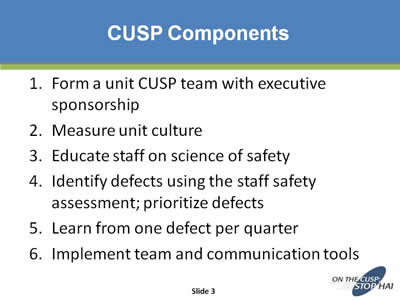
- Form a unit CUSP team with executive sponsorship
- Measure unit culture
- Educate staff on science of safety
- Identify defects using the staff safety assessment; prioritize defects
- Learn from one defect per quarter
- Implement team and communication tools
Slide 4. How is CUSP Different? It Empowers Nurses
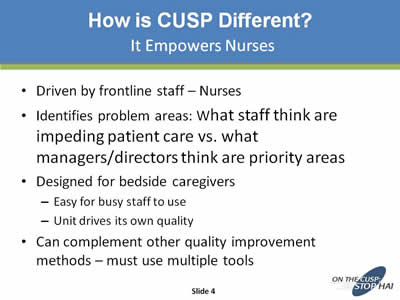
- Driven by frontline staff – Nurses
- Identifies problem areas: What staff think are impeding patient care vs. what managers/directors think are priority areas
- Designed for bedside caregivers
- Easy for busy staff to use
- Unit drives its own quality
- Can complement other quality improvement methods – must use multiple tools
Slide 5. St. Joseph Mercy Hospital's Journey
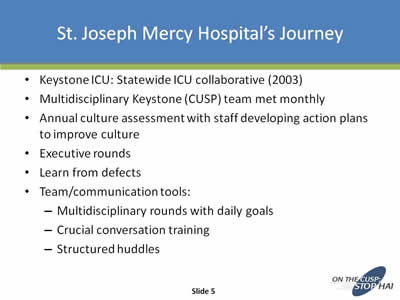
- Keystone ICU: Statewide ICU collaborative (2003)
- Multidisciplinary Keystone (CUSP) team met monthly
- Annual culture assessment with staff developing action plans to improve culture
- Executive rounds
- Learn from defects
- Team/communication tools:
- Multidisciplinary rounds with daily goals
- Crucial conversation training
- Structured huddles
Slide 6. Best Practices: Learning from Defects Tool

Image of several pages from a document called "Mindfully Learning from Defects".
Slide 7. Best Practices: Engaging & Sustaining Nurse Involvement in CUSP Huddles
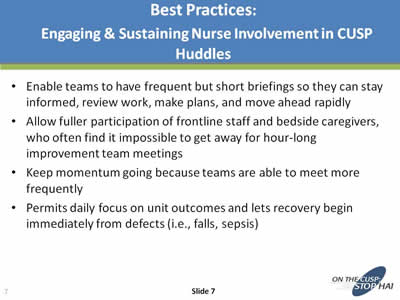
- Enable teams to have frequent but short briefings so they can stay informed, review work, make plans, and move ahead rapidly
- Allow fuller participation of frontline staff and bedside caregivers, who often find it impossible to get away for hour-long improvement team meetings
- Keep momentum going because teams are able to meet more frequently
- Permits daily focus on unit outcomes and lets recovery begin immediately from defects (i.e., falls, sepsis)
Slide 8. Components
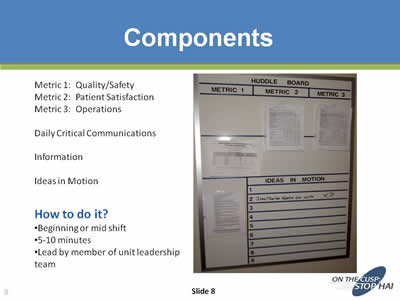
Metric 1: Quality/Safety
Metric 2: Patient Satisfaction
Metric 3: Operations
Daily Critical Communications
Information
Ideas in Motion =
How to do it?
- Beginning or mid shift
- 5-10 minute
- Lead by member of unit leadership team
To the right of the text is an image of a Huddle Board.
Slide 9. SICU Huddle Board
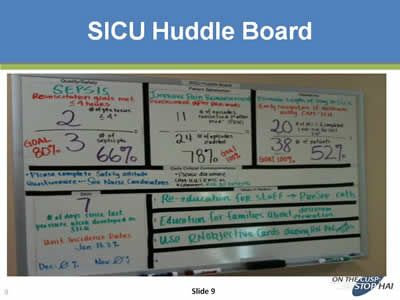
Image of a Surgical Intensive Care Unit (SICU) Huddle Board.
Slide 10. Surgical Unit Huddle Board
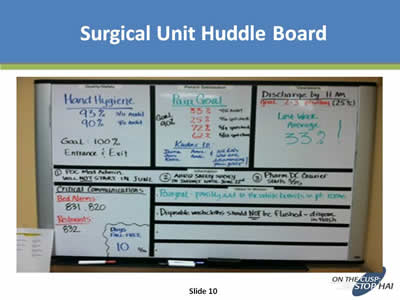
Image of a Surgical Intensive Care Unit (SICU) Huddle Board.
Slide 11. Lessons for Your Hospital: Strategies That Promote Nurses & Leverage CUSP
- Frontline staff are an integral part of the CUSP team
- Teams should meet monthly
- Nurses who work in the unit every day are the best people to identify where there are opportunities to improve and how to improve
- Nurses need to be allowed to take responsibility for identifying problems and be given a forum and strategy to solve them:
- CUSP team
- Learn from defects tool
- Structured huddles
Slide 12. A Healthcare Imperative
“In medicine, as in any profession, we must grapple with systems, resources, circumstances, people, and our own shortcomings, as well. We face obstacles of seemingly endless variety. Yet somehow we must advance, we must refine, we must improve.”
Atul Gawande, Better: A Surgeon’s Notes on Performance
Slide 13. Joanne Timmel, MSN, RN, NE-BC
Nurse Manager
The John Hopkins Hospital
On top of slide it states: "CLABSI Supplemental Call Series"
Slide 14. Implementing CUSP: Assumptions & Prerequisites
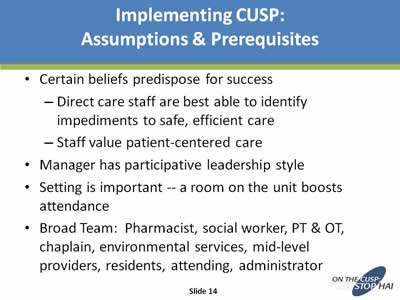
- Certain beliefs predispose for success:
- Direct care staff are best able to identify impediments to safe, efficient care
- Staff value patient-centered care
- Manager has participative leadership style
- Setting is important -- a room on the unit boosts attendance
- Broad Team: Pharmacist, social worker, PT & OT, chaplain, environmental services, mid-level providers, residents, attending, administrator
Slide 15. Implementing CUSP: Engaging the Team
- Define CUSP for your setting
- Kick off with science of safety presentation
- Ask the question: “How will the next patient be harmed on our unit?”
- Return to Contents
Slide 16. CUSP: How it Empowers Nurses in the Hospital
Nurses are empowered when —
- They see change happen
- Their concerns are affirmed
- They develop a voice and can tell their story
- They are supported by a unit culture that values speaking up regarding patient safety
Nurses are empowered when they actually have power
Slide 17. CUSP: Example of Empowerment
A surgical unit before CUSP —
- Chaos
- Unclear plan of care
- Very poor communication with the surgeons
- Patients frustrated and angry at nurses
- Nurses felt powerless, so they left — high turnover
Slide 18. CUSP: Example of Empowerment
Our first CUSP project:
- Proposed cohorting
- Implemented nurse-physician joint rounds
- Developed a written daily goal sheet generated from rounds
- Established other mechanisms for non-urgent communication besides rounds
- Continued to articulate collaborative culture by hosting First Monday breakfasts
Slide 19. CUSP: Example of Empowerment
Nurses now have a place to address day-to-day intransigent system problems
- Medications not available when due
- Pain control issues in admitted outpatients
- Inpatient nurse/PACU nurse communication
- Contributing factors to recent medication errors
- New residents’ lack of familiarity with POE system
- Strategies for coverage with decreased resident hours
- Pain control issues/narcotics issues with patients with chronic pancreatitis, Interventional Radiology patients
Slide 20. Best Practices: Engaging & Sustaining Nurse Involvement in CUSP
- Absolutely requires three strong champions: Nurse, physician, administration
- Monthly meetings require email reminders, individual invites, reminders throughout day, support to allow staff to step away from patients
- Energy maintained when you focus on what matters to the bedside nurse
- Really resolve some problems
Slide 21. Lessons for Your Hospital: Strategies That Promote Nurses with the Leverage of CUSP
- If nurses are not engaged in the CUSP process, ask why
- Are you trying to lower CLABSI rates by ultimately requiring nurses to do more when they know they aren’t able to do half of what they expect of themselves?
- Find low-hanging fruit (e.g., need red labels on high-concentration PCA)
Slide 22. Questions?