This report is based on research conducted by Abt Associates in partnership with the MacColl Center for Health Care Innovation and Bailit Health Purchasing, Cambridge, MA, under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract Nos. 290-2010-00004-I/ 290-32009-T). The findings and conclusions in this document are those of the authors, who are responsible for its contents; the findings and conclusions do not necessarily represent the views of AHRQ. Therefore, no statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services.
Suggested citation: New Models of Primary Care Workforce and Financing Case Example #5: WellMed. (Prepared by Abt Associates, in partnership with the MacColl Center for Health Care Innovation and Bailit Health Purchasing, Cambridge, MA, under Contract No.290-2010-00004-I/ 290-32009-T.) AHRQ Publication No. 16(17)-0046-5-EF. Rockville, MD: Agency for Healthcare Research and Quality; October 2016.
Table of Contents
Introduction
Why WellMed?
Overview of the Practice
Patient Population Description and Practice Panel Size
Model of Care
Workforce Configuration
Care Coordination
Care Management
Pharmacy Integration
Behavioral Health Integration
Palliative Care
Workflow
Team Building and Training
Access, Comprehensiveness, and Quality
Access
Comprehensiveness
Quality
Implications for Primary Care Staffing Models
Acknowledgements
Introduction
The Agency for Healthcare Research and Quality (AHRQ) contracted with Abt Associates and its partners, the MacColl Center for Health Care Innovation and Bailit Health Purchasing, to conduct research on innovative ways to configure primary care workforce teams that can deliver fully comprehensive, high-quality care to the U.S. population. The purpose of the research is to offer models of primary care teams and the associated costs for consideration and discussion by policymakers and providers in the field of health services delivery. To explore existing innovative workforce configurations, AHRQ and the Abt project team conducted a literature review, explored extant data sources, convened a Technical Expert Workgroup of national experts in primary care workforce, and conducted site visits to primary care practices with innovative workforce configurations.
The case example report that follows provides an in-depth look at the workforce configuration of WellMed, a health care delivery network serving primarily Medicare-eligible seniors. This site visit included visits to a WellMed clinic: WellMed at Medical Center (located 7622 Louis Pasteur Dr., Suite 100, San Antonio, TX 78229); Specialists for Health-Cardiology at Medical Center (located at 4330 Medical Dr., Suite 500, San Antonio, TX 78229); WellMed Headquarters (located at 8637 Fredericksburg, Ste. 100, San Antonio, TX 78240); a new senior clinic, WellMed at Crockett Park (located at 1715 McCullough Ave., San Antonio, TX 78212); and the Trevino Lopez Senior Center (located at 8353 Culebra Rd., San Antonio, TX 78251). Team members visited the practice on September 16–17, 2015. The data discussed below were collected on or prior to the visit and reflect calendar year 2014.
Why WellMed?
WellMed is a large and growing integrated ambulatory care system with a well-established model of care that has been implemented across Central Texas and in Florida. WellMed assumes risk for all of its Medicare Advantage patients and, using the flexibility of capitated payment, has crafted a suite of primary care and specialty services designed to meet the needs of their population with minimal referral outside the system. Although the system does not specifically seek patient-centered medical home recognition, its primary care practices are team based, with enhanced roles for all staff. It aspires to “one-stop shopping” for patients, bringing in-house specialists to the primary care clinics and providing onsite lab and imaging services and behavioral health. WellMed is embedded in the community and partners with local and State agencies to provide health and social services at all senior centers in the San Antonio area and to spread this model to other locations.
Overview of the Practice
WellMed was founded in San Antonio in 1990 by George M. Rapier, MD, with the goal of changing health care delivery for seniors. His vision was to provide quality, proactive, preventive care and build strong patient relationships. The stated mission of WellMed is to “help the sick become well and to help patients understand and control their health in a lifelong effort at wellness.” WellMed has more than 800 primary care locations in Texas and Florida, more than 85 of which have integrated specialist services. Over 6,000 providers in the WellMed system provide services in dermatology, geriatrics, cardiology, family practice, hospital medicine, internal medicine, neurology, osteopathy, palliative care, pain management, podiatry, rheumatology, and wound care. The system runs ambulatory care practices and senior care centers.
WellMed highlights its leadership in medical risk management, effective disease management and chronic care programs, and specializes in the complete coordination of care for patients. The system is growth oriented, with a strong acquisitions team. WellMed promotes its services to prospective patients as providers who can spend time with patients, offer affordable care, and connect qualified patients with State and Federal social and financial assistance programs.
Patient Population Description and Practice Panel Size
WellMed serves more than 200,000 people in the San Antonio area who receive coverage from Medicare Advantage. WellMed flourishes in the San Antonio market in part because San Antonio does not have many secondary insurance coverage options. Most people have only traditional Medicare, and WellMed can provide much more comprehensive care than standard fee-for-service Medicare, which allows very fragmented access to specialty care.
The WellMed standard for a panel is 600 capitated patients, although some physicians have many more. Historically, physicians were paid without consideration of panel size; now the bonus policy is tied to the number of patients in the panel. New patients typically choose their provider, so panels are not assigned, but grow. Patient panels in WellMed primary care practices are primarily Secure Horizons Medicare Advantage beneficiaries for whom WellMed assumes full risk. WellMed has two categories of fee-for-service patients on panels: a small number of patients retained in provider panels when their practice was acquired, and WellMed employees who receive primary care at WellMed clinics. Approximately 90 percent of the panel of Dr. Nahim Pearose, the physician whose practice was the focus for the site visit, is capitated and 10 percent are commercial patients. Dr. Pearose's current panel is approximately 400 Secure Horizons patients. He estimated 60 commercial patients. Dr. Pearose sees an average of 10–13 patients per day, spending an average of 15 minutes of a total 30-minute visit with each patient. The combined total number of patients for the 2.8 FTE providers at the Medical Center clinic is 2,200, comprising 1,970 Medicare Advantage patients and 250 with commercial insurance.
Model of Care
The WellMed new patient brochure describes the care model as including:
- Access to care & information
- Health care for all
- After-hours access coverage
- Accessible patient & lab information
- Practice-based services
- Comprehensive care for both acute & chronic conditions
- Prevention screening & services
- Ancillary diagnostic services
- Care management
- Wellness promotion
- Disease prevention
- Patient engagement and education
- Care coordination
- Collaborative relationships—ER, hospital care & specialist care
- Care transition
- Practice management
- Disciplined financial management
- Cost-benefit decisionmaking
- Facilities management
- Health information technology
- Electronic medical record
- Electronic orders & reporting
- Evidence-based decision support
- Quality & DataRAPS
- Evidence-based best practices
- Medication management
- Quality improvement
- Practice-based care team
- Provider leadership
- Effective communication
- Patient participation
- Health coaches
Workforce Configuration
Exhibit 1: WellMed at Medical Center Clinic team FTEs and roles
| FTE | Workforce Category/Role | Comments |
|---|---|---|
| 2.8 | MDs | Five physicians: 2 full-time, 1 part-time (0.5), 1 who works one morning session per week (0.1), and 1 who works one day per week (0.2). |
| 1.0 | PA | One full-time PA. |
| 1.0 | Scribe | Two part-time medical students for 1.0 FTE who scribe for Dr. McCarroll. |
| 2.0 | LVN health coach | Two full-time health coaches support one pod (three providers) each. |
| 2.0 | LVN | Two full time LVNs (aside from the two health coaches) perform triage for incoming calls and walk-ins. |
| 8.0 | MA | Seven full-time MAs are dedicated to specific pods. Two full-time float MAs act as triage nurses, filling in as needed. One full-time ancillary MA performs additional MA tasks for all pods as needed. A full-time team lead is the back-up clinic manager as needed. The team lead has MA training and helps with MA tasks such as maintaining daily flow logs, and ensuring the procedure room is clean. |
| 1.0 | X-ray technician | One full time x-ray technician performs onsite scans. |
| 1.0 | Phlebotomist | One full-time phlebotomist works onsite performing blood draws, sending them for analysis, and conducting other phlebotomy tasks as needed. |
| FTE | Business Operations Support Workforce Category/Role | Comments |
| 1.0 | Clinic manager | One full-time clinic manager. |
| 1.0 | Administrative staff person exclusively dedicated to insurance verification | |
| X | IT | Role contributed/managed centrally. |
| X | Housekeeping, security, maintenance | Role contributed/managed centrally. |
| FTE | Front Office Support Workforce Category/Role | Comments |
| 3.0 | Front desk staff | Three full-time staff schedule appointments and register/check-in/check-out patients. |
| 1.0 | Call Center/Operator | |
| 2.0 | Medical records clerks | Two full-time clerks pull medical records and enter data as needed and scan all paper charts into the eClinicalWorks EHR. |
MD=medical doctor; PA=physician assistant; LVN=licensed vocational nurse; MA=medical assistant; IT=information technology; LVN=licensed vocational nurse; MA=medical assistant; EHR=electronic health record; X=No specific FTE provided/role may be paid for and managed centrally
The WellMed at Medical Center clinic is one of 84 WellMed clinics in the San Antonio area and serves a primarily geriatric, Medicare-eligible population. The clinic has had almost no staff turnover in over 4 years. The clinic manager said that staff longevity means the clinic teams work well together, trust each other's judgment, and communicate openly and consistently. Along with exam rooms and a reception area, the clinic has onsite x-ray and lab services, and a room for minor procedures.
Primary care providers (PCPs) and physician assistants (PAs) are primarily employed staff, with selected in-house specialty services as well. The clinic is divided into two “pods,” which are PCP–medical assistant (MA) teamlets with a floating MA available as needed. The two pods are physically located on opposite sides of the clinic with MA and triage nurse desks in the center. All providers, MAs, and triage nurses can talk to each other across the center desk via an opening in the wall for quick verbal communication when needed. Teams meet daily and as needed in huddles to plan the day's patient schedule and review outstanding items. Each pod has a dedicated health coach. The health coach is an integral part of the pod and works closely with patients to establish care plans around issues such as diabetes care or weight loss. Health coaches use motivational interviewing (MI) techniques to ensure goals set with the patient are patient driven. The health coaches say that, because patient relationships are at the core of their work, patient-driven goals result in higher follow-through and goal achievement. The coaches follow up weekly with patients to monitor progress and ensure they are making progress toward their goals. The health coach we interviewed normally tracks ~30 followup calls per day. In addition, this coach is also a licensed vocational nurse (LVN) who acts as a backup nurse, starting intravenous medications, inserting catheters, helping with medical records, and performing other clinical tasks as needed. Although medical issues are the core of the health coaches' training, they regularly field requests about psychosocial needs and liaise with WellMed behavioral health services and social work. The health coach we interviewed mentioned that older patients may turn to a health coach they feel comfortable with for mental health needs related to depression caused by loss (for example of a spouse or personal health), mental decline, or other issues. She said many Latino or Asian patients are culturally inclined to simply agree with the provider as a person of authority, but may feel more comfortable being open about personal health information when meeting with the health coach. In this role, the health coach is alerted early to potential physical or mental health issues and has a broad understanding of the patient's current health issues. The coach can share this information with the larger care team (PCP, MA, behavioral health provider, etc.), who can tailor care appropriately.
WellMed employs one or two health coaches at each clinic. Clinic coaches have monthly meetings with the larger health coach group and monthly meetings to enhance skills, such as MI techniques. Due to the success of the onsite health coaches, the Medical Center clinic accomplishes most diabetes coaching in-house. The health coaches are also part of the practice manager's core group that works on process improvement and takes the lead on clinic-specific issues.
Mary Hopkins, the practice manager of the WellMed at Medical Center clinic, oversees all workforce issues, clinic-specific strategy planning, staffing, and physical space needs. She is assisted by a team lead who was trained as an MA and is the backup clinic manager. Mary is committed to the idea of “backups for her backups” and encourages crosstraining as appropriate for licensure. She believes that when staff support each other and feel supported, they do their jobs more effectively, efficiently, and compassionately. Mary says she works hard to address issues in real time and doesn't hesitate to call a quick meeting or follow up with staff on the spot to address issues or concerns. Mary said that patient care comes first, and staff members are encouraged by Dr. McCarroll, a clinical lead, and by the supervisory staff to respect each other.
“It doesn't say Dr. McCarroll on the outside of the building, it says WellMed. It's about the patient.”
– Mary Hopkins, Clinic Manager
Care Coordination and Transitions
Centralized elements of the WellMed system, such as its care management program, palliative care, and employed hospitalists in local inpatient facilities, are connected to primary care by structural ties. These ties include dedicated care managers and hospitalists for each clinic who develop relationships with staff and patients. Primary care and specialist physicians attend common grand rounds so information and strategies can be shared. Hospitalists and other specialists are culturally and financially incentivized to communicate with PCPs. Messages among primary care teams, centralized care management staff, and specialist providers are tracked in the electronic health record (EHR) and at Patient Care Committee (PCC) meetings. Physicians are incentivized to track and intervene with high-risk patients to keep readmission rates low, and at a minimum to communicate well through the PCC meetings.
The WellMed PCC meeting, held weekly at each clinic, reviews care for all patients who: 1) are currently hospitalized, 2) were recently discharged from the hospital, or 3) made an emergency room (ER) visit. The clinic manager, physicians, PA, and health coaches all attend this meeting. Care managers, referral coordinators, and palliative care physicians assigned to the clinic from WellMed central services also attend in person. Hospitalists for hospitalized patients call in.
Physicians or hospitalists for hospitalized patients present cases, establish care plans, anticipate problems, and plan follow-up services. Meetings use a transition or ER tracking sheet, prepared by utilization management for the organization that lists all patients from the clinic in the review categories. The PCC team assigns or adjusts the risk level of each patient, based on clinical parameters. The team may assess caregiver support and home environment, suggesting home visits or considering referral to palliative care or other services, depending on the circumstances. The meetings are designed to keep all providers current so they can work as a team and can assist other PCPs' patients.
In the Medical Center clinic, care is coordinated through the nurse triage hub that is physically located in the center of the clinic and through the collaborating health coaches. Triage LVNs receive emails and telephone calls from patients requesting care. The triage nurse sends the request to a PCP, usually the PA, who reviews items entered by the triage nurse and decides whether the patient requires an in-person visit, a referral to a specialist, laboratory tests, or updated medications. The PA can also perform other provider-level actions. Decisions are usually ~20 minutes from item entry. Health coaches also directly coordinate patient care through greater WellMed and a non-WellMed network of specialists and community resources. Health coaches regularly address behavioral health issues with patients and refer directly to WellMed social workers and behavioral health specialists. Community resources include the Texas Department of Aging and Disability, and Project MEND, which provides medical equipment at no charge or reduced cost.
Care Management
WellMed patients have access to multiple specialty care options within WellMed and to consultative specialty providers outside the system when indicated. Registered nurse (RN) outpatient case managers oversee the management of high-risk patients with multiple chronic conditions based on their risk stratification scores. The case managers also oversee patients in the hospital in collaboration with hospitalists and health coaches. These RNs set up followup appointments with specialists, determine barriers to discharge, and work with social service agencies to provide services. Transition care followup is typically 30 days.
Complex patients receive services from an RN outpatient case manager assigned to the patient's primary care team. This RN conducts home visits to ensure the patient is taking the appropriate medications, assess symptoms, and perform other tasks. Complex patients may be referred to care management by their PCP, who can request a home visit to determine complexity and the adequacy and safety of their home environment. An assessment determines followup frequency. All patients in a particularly high-risk stratification category receive in-home visits, with the care manager sending regular reports to and communicating with the PCP. In-hospital care managers refer complex patients to outpatient care management. Both in-hospital and outpatient case managers attend Medical Center PCC meetings, either in person or on the phone. Complex care followup is traditionally for 90 days before the patient is returned to the primary care team. The patient's willingness to accept services also determines followup and interactions.
WellMed is currently conducting a telemedicine pilot with RN case managers who install scales, blood pressure measurement devices, and pulse oximetry equipment in patient homes. To report their health remotely, patients answer five computer-generated “yes/no” questions (in English or Spanish). Alerts generated by “no” answers or out-of-range clinical measurements are relayed to centralized telemedicine RNs, who alert care management.
WellMed has no specific protocols for specialty referrals to avoid creating barriers to referral and educates PCPs on algorithms for care. Commonly used specialty physicians such as cardiologists have specific office hours in primary care clinics and frequently see patients together with the PCP. WellMed has far fewer specialists than other systems: for instance, they have no endocrinologists. WellMed is starting to focus on the culture of care between primary and specialty care with the goal of helping both groups understand they are on the same team and realize the importance of collaborating with the right people.
Pharmacy Integration
WellMed addresses medication management for geriatric populations by conducting medication reconciliation at every primary care and specialty visit. Patients are asked to bring all their medications with them to every visit. WellMed is developing a partnership with the University of the Incarnate Word to collaborate on integrated pharmacy care delivery.
Behavioral Health Integration
Behavioral health services at the Medical Center clinic are provided 4 hours per week by a psychiatrist supplied by Zeitgeist, a local mental health organization. Services are medication management for mental illness (including major depression), and behavioral modification therapy. The Medical Center clinic also partners with a local behavioral health training program. For a $5 flat fee, clinicians in training will see any WellMed patient for individual and family counseling, behavioral health, and cognitive behavior therapy.
Palliative Care
Palliative care is an integral part of primary care for geriatric populations at WellMed. Unlike hospice, palliative care still provides primary care, while focusing on comfort. Dr. Elizabeth Glazier started the palliative care program at WellMed as a subspecialty consultation service, offering expertise on palliative care issues to PCPs and care managers. The program now has a multidisciplinary care team that provides home visits and on-call services 24/7.
Any WellMed member is eligible for palliative care services at no out-of-pocket expense. Patients are referred to the program either directly by their PCP or via a palliative care team representative who regularly attends the PCC at their PCP clinic. Patients can be seen in clinic or in the home. Patients seen at home, who are the most ill, are often admitted into the Bridges home visiting program within palliative care. Patients retain their PCP, who is included in all decisions to maintain continuity of care. The Bridges team also uses the eClinicalWorks EHR and advises the PCP about all decisions and updates.
Psychosocial issues are primarily addressed by social workers on the palliative care team, who also train WellMed RNs, MAs, LVNs, and nurse practitioners in relevant skills. The entire palliative care team performs home visits. Some homebound patients need advanced clinical care, so the team says it creates “a clinic without walls.” The team also notes food and household needs, facilitates as-needed behavior change and home modifications, and supports the caregiver.
The palliative care team interfaces with WellMed PCPs about care issues, end-of-life plans, and changes in care goals to balance guideline-driven care and what is preferred by the patient. The palliative care program refers to hospice and works with many hospices in San Antonio; none are part of WellMed. Hospice provides services such as 24/7 nurses who respond in home, a chaplain, and in-home bathing. The palliative care team says it is proud that 90 percent of patients in the program die at home with family near. This far exceeds the national average for dying at home, which is a general patient preference, and also avoids the high cost of a terminal hospital stay. The team is figuring out how best to prevent patients from final, unnecessary hospitalizations and are encouraging earlier referral to palliative care. The WellMed palliative care service initiated a “Call us first” campaign with a refrigerator magnet encouraging patients to call them first and not 911. They educate about the services they provide, such as intravenous fluids, x-rays, advice, and reassurance about disturbing symptoms. The program is resulting in fewer catastrophic high cost cases that end with patients dying in intensive care units. The program is a financial benefit for the system, but Dr. Glazier also believes it creates a much better quality end-of-life experience for patients.
Dr. Glazier is a proponent of the palliative care model as a way for geriatric patients to age in place. She gives regular grand rounds presentations and is developing an algorithm or protocol to help PCPs understand when to refer to palliative care. She would like to take this protocol nationwide to share with other Medicare advantage programs and is developing a “palliative care in a box” starter kit for this purpose.
WellMed Palliative Care Staffing Model (provided by WellMed)
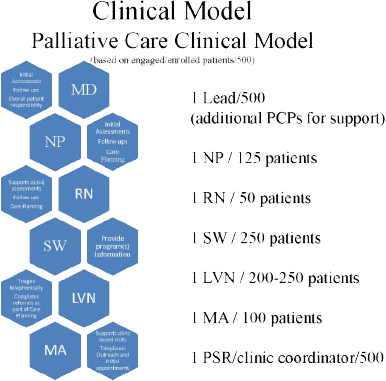
Source: American Academy of Home Care Medicine
Workflow
At the WellMed at Medical Center clinic, the front desk staff use a color-coding system for patient charts. For example, patients who received reminder calls about upcoming appointments have lavender flags in their chart. Front desk and medical records staff and the x-ray technician divide the task of calling patients to remind them of appointments. Outstanding issues are identified during the reminder call or when the patient arrives. To prepare for a patient visit, an MA reviews the patient's record before the visit and discusses issues or concerns with the PCP in the daily huddle. The front desk staff greets the patient on arrival and marks the patient's chart to tell the MA that the patient has arrived and has been checked in.
Workflow at the Medical Center clinic follows many common clinic workflow procedures with a few notable exceptions. To directly engage and emphasize the patient-first mission, patients are approached in-person by the MA in the waiting room. To assist with recognition, patients are photographed when they come for their first visit.
Once patients have checked in, MAs record weight and vitals and talk with patients to put them at ease. MAs also review reasons for patient visits and medications, and check for standard well-care such as last colonoscopy or mammogram and other preventive care if applicable. If laboratory tests are needed or vaccines are due, this is noted in the electronic record as part of patient followup. MAs then check with the PCP to confirm ordering of necessary tests. MAs leave while the PCP performs the visit and addresses the reason for the visit. The PCP enters medical information into the EHR in real time. Visits often take ~30 minutes because of the needs of the geriatric population. Once the PCP part of the visit is complete, the MA returns to deliver vaccines or escort the patient to the laboratory or x-ray if needed. Followup visits, if necessary, are scheduled at the front desk before the patient leaves. Referral or followup information is relayed to the patient again by the front desk staff. Some patients receive followup calls directly from the health care coach or the PCP, depending on their care plan.
Physician Scribes
One physician at the Medical Center clinic uses a scribe for documenting visits; this is a growing trend among WellMed providers. Scribes are often pre-med students who work closely with a single provider on a daily basis. The main role of the scribe is to record all visit interactions and procedures in the EHR, ensure complete capture of the visit, and record followup recommendations. The physician at the Medical Center clinic who uses a scribe felt that this allowed him to be much more efficient during the patient visit because he was able to focus on patient assessment and interaction instead of EHR input. Having the scribe record patient history in real time improves charting accuracy. The physician has learned to dictate during most of the visit so the scribe can capture details. The scribe had a Bachelor of Science degree and was studying to be a PA and said the role was useful for learning how to interact with and assess patients during a visit. The scribe gave a recent example of learning how two seemingly unrelated conditions (glaucoma and high blood pressure) can be related, through observing the physician and asking questions after the visit.
Protocols
The Medical Center clinic has been working on implementing standard protocols. At the time of the site visit, the PCPs had reviewed new protocols for urine analysis, chest pain, and electrocardiograms. Before deciding to standardize, the staff followed similar protocols, but they were not formalized.
Exhibit 2: WellMed at Medical Center Team Tasks and Roles
| Tasks | Roles Included |
|---|---|
| Pre-visit planning, chart scrubbing | MA reviews care gaps and checks for preventive services that are due and shares information with the physician ahead of the scheduled visit. An MD or PA may be involved in monitoring preventive services. The care team (PCP, health coach, and MAs) holds a daily huddle to review the day's cases; the health coach checks on patients' action plans including if milestones have been achieved. |
| Greeting the patient | Three staff dedicated solely to greeting patients greet the patient on arrival and confirm registration in the WellMed system with necessary information on file such as an up-to-date HIPAA form and current insurance card. The front desk staff marks the patient's chart so the MA knows the patient is ready for an exam room. The front desk staff help the MA identify the patient if the MA cannot quickly match the photo to the patient. |
| Ordering lab tests and collecting vital signs | MA greets the patient in the lobby by name, takes them to the exam room, collects weight and vitals, and confirms the reason for the visit. Necessary lab tests are confirmed by the PCP and ordered by the MA. |
| Delivery of routine preventive services | MA is responsible for the delivery of routine preventive screenings and some services. The clinic is currently developing and standardizing protocols for routine tasks. Providers deliver clinical preventive services. |
| Medication reconciliation or management | Reconciliation is by MAs and confirmed by clinicians. The clinic does not have a pharmacist on staff. |
| Reviewing and reconciling problem list | This is a PCP role. |
| Patient navigation | This is primarily an MA or health coach role, but can be shared by front desk staff, the phlebotomist, or x-ray tech as needed. |
| Self-management goal setting and action planning | Health coaches lead self-management goal setting and action planning. Plans are reviewed and approved by the PCP. The health coach may meet with the patient one-on-one or when the PCP is in the room. If a problem or question arises in one-on-one visits, the PCP might come back into the room. Health coaches follow up with the patient's action plan and goal achievement between clinic visits or on visits arranged specifically with the patient. |
| Patient telephone/ email followup |
The MA, triage LVN, health coach, or front desk person may perform these tasks, depending on the purpose. Direct patient-care followup is by the MA or LVN. Appointment reminders are primarily by the front desk with assistance from the x-ray tech and other staff. |
| Injections and venipuncture | This is performed by the MA or onsite phlebotomist. |
| Triaging phone calls and emails | MAs and triage nurses cover most emails and calls (e.g., for insurance, referrals, routine refills, health concerns). Health concerns are routed to the PCP via email, and PCPs determine if the patient requires a visit or if the issue can be addressed remotely via email or phone. MAs and triage nurses can consult PCPs. The triage nurse can take patient history, but cannot make recommendations. |
| Care and transition management of high-risk patients | RN outpatient case manager provided centrally. |
| Referral management | Referrals are by a PCP except for routine preventive services. Triage nurse or MA can start an order for routine services that are reviewed and sent by a PCP. |
| Medication titration | This is a PCP role. |
| Independent visits by non-providers (RN, MA, health coach) | Health coaches or an ancillary MA may have independent visits with patients. |
MA=medical assistant; MD=medical doctor; PA=physician assistant; PCP=primary care provider; HIPPA=Health Insurance Portability and Accountability Act; LVN=licensed vocational nurse; RN=registered nurse
Team Building and Training
The clinic manager at the WellMed at Medical Center clinic attributes the record of more than 4 years with no staff turnover to exceptional staff collegiality fostered through constant, open communication, and an emphasis on staff crosstraining (within licensure allowances) to fill in for other staff. This arrangement creates a true team environment in which staff members can cover for each other during busy times or help another staff member complete a task. It also allows for vacation and sick time to be covered without excess strain on other staff members and the clinic overall. Nonetheless, individual roles have specific training; the training we heard most about was the health coaches. They attend monthly, 30-minute WellMed-wide health coach calls focusing on topics relevant to their work such as MI and disease-specific training.
Access, Comprehensiveness, and Quality
Access
The WellMed Charitable Foundation, an independent nonprofit organization that serves seniors and caregivers, entirely funds one large senior center; two others are funded by a public-private partnership with the city of San Antonio. All services, including nurse and social worker access, are free to any community member.
Comprehensiveness
WellMed might be considered an aspiring “medical neighborhood.” It has a strong presence in the San Antonio community, with 84 clinics and 6 senior centers, 3 of which are directly connected to primary care clinics. WellMed provides services particularly tailored to a geriatric or senior population, including among the in-house specialty services those most frequently used by this population. The exception is behavioral health services, provided only marginally in the primary care clinics.
Community Linkages
The Alicia Trevino Lopez Senior Center is one of two centers co-located with WellMed primary care clinics. The center is a large facility with an intentionally open floor plan to invite seniors to ask about the activities. Carol Zernial, gerontologist and director of the WellMed Charitable Foundation, described the collaboration between the senior center and primary care as a “holistic approach, coordinating social services with the entire primary care team to establish behavior change and community support.” The center offers exercise equipment and a personal trainer, free meals, classes such as dancing and yoga, a large pool table room, a teaching kitchen with cooking and nutrition classes, an art studio in collaboration with a local senior living arts center, a movie room, and an e-library offering onsite downloading of electronic books by scanning barcodes. Onsite social workers offer connections to other community and caregiver support services.
The center adjoins a WellMed primary care clinic, a model they would like to encourage for all the senior centers. At the WellMed clinic adjacent to the Lopez center, primary care physicians prescribe exercise at the senior center and refer patients to senior center activities that might help with depression. The center is collecting data on center use and would like to study whether or not locating primary care clinics near senior centers increases access. Approximately 30% of center participants are WellMed patients. A WellMed nurse is onsite, available to all participants, not just WellMed patients. The center is currently testing a medication safety program for seniors, with caregiver outreach to improve medication adherence based on a program currently available in Canada.
The WellMed Charitable Foundation also funds nurses and social workers who rotate among all 65 San Antonio-area senior centers, offering medical and social services without fees. The RNs float among centers, but are regularly assigned to specific centers to develop relationships with participants. The RN service is seen as a cost-saving measure because, for example, controlling diabetes early helps reduce high medical costs. WellMed also provides transportation for medically or financially eligible patients through their Comfort Care Transportation program.
Carol Zernial believes WellMed can expand the influence of primary care with senior centers and other partnerships and that the medical community does not have sole responsibility for primary care. She sees WellMed partnerships as a huge opportunity, citing the Chronic Care Model as a reason for community involvement in health care.
Quality
WellMed takes pride in their health care economics department that provides rich data to support quality initiatives. As each clinic site enters data, the quality department synthesizes quality assurance data and creates reports for various quality initiatives, including a “report card” for each PCP.
The larger WellMed organization holds twice-yearly learning sessions attended by a triad from each clinic: the clinic manager, lead physician, and a health coach. These regional meetings explain new initiatives and highlight specific principles of the organization's quality improvement mandate. PCPs translate these initiatives to their practices. If a new focus for advancing quality is emphasized, a new metric is created to monitor it.
Quality improvement (QI) among specialists and between primary care and specialist departments is supported by what WellMed calls compacts with specialty services rather than contracts. Data services provide report cards to specialists to allow comparison among departments and peer providers. The report cards show the number of referrals sent to another group to foster quality and positive competition.
Quality Improvement Efforts and Culture
On the 4th Thursday of the month, the Medical Center clinic closes from 12 to 5 o'clock for a clinic-wide meeting. All staff attend, so phones roll over to an answering service. Staff members meet in the waiting room so they can address patient walk-ins. Monthly meetings review PCP metrics in real time with the PCPs. PCPs said they are asked to “leave their feelings at home.” Primary care team members feel responsible for improving metrics, so improvement strategies are addressed as a team. The clinic does not have a formal quality team, so the entire staff is responsible for QI.
At the Medical Center clinic, MAs, LVNs, and health coaches meet weekly or every other week, depending on needs. They discuss current issues such as the ICD-10 rollout or common problems. The clinic manager leads these meetings in a round table-discussion format. The team says it has worked together for so long that much of the process-change work is organic and discussed via email. The clinic manager, health coaches, and LVNs hold ad hoc meetings to iron out workflow problems and design workflows for new processes.
A health system-wide WellMed efficiency and quality group called the New WellMed Experience Team circulates into clinics to identify inefficiencies using a “brown paper process.” The group draws a patient flow process on brown butcher paper on the wall, intentionally setting it up incorrectly to help engage staff on the workflow for this process at their clinic and how it might be improved.
The WellMed PCC meetings have a segment called the power hour in which each PCC team reviews counts of ER visits, hospitalizations, and readmissions, comparing them with goals set by each clinic for quality initiatives. The meeting ends with a quality score review from the PCP report card, tracking each provider's quality scores on a whiteboard for a transparent sharing of scores. PCC team members are asked to strategize about processes to improve low scores.
Implications for Primary Care Staffing Models
WellMed has had significant success at designing care for aging populations. Its integrated, “one-stop shopping” model of care is convenient for seniors and may be a model for efficient and effective care in the following ways:
- Integrated systems with employed primary care and specialist staff offer efficiencies in care coordination and continuity of care across settings.
- Integrated palliative care services can cut costs and achieve higher patient satisfaction for extremely ill patients.
- Health services tailored to geriatric populations can improve comprehensiveness and convenience of care.
- Primary care teams with no RNs can deliver care to high-risk populations effectively if communication between PCPs and central care management services is optimized.
- Integrating primary care with Senior Centers further integrates health care into the lives of patients.
WellMed has disseminated its care model rapidly and successfully in Texas and Florida. Aside from geographic or cultural considerations that might affect spread, the following lessons might be valuable across settings:
- Crosstraining can be an essential component of sustainability in primary care.
- Employing standard work practices enables efficiencies across settings.
- Partnering with community agencies in providing social and health services is an effective spread mechanism.
Acknowledgements
We thank the leadership at WellMed, especially Drs. Chris Arnold and Elizabeth Glazier, and the entire staff of Medical Center Clinic for hosting a site visit for the AHRQ New Models of Primary Care Workforce and Financing project. A special thank you to Daniel Calderon, public relations lead strategist at WellMed for organizing our visit.



