Implement Teamwork and Communication for Perinatal Safety
AHRQ Safety Program for Perinatal Care
Slide 1: AHRQ Safety Program for Perinatal Care
Implement Teamwork and Communication for Perinatal Safety
Slide 2: Learning Objectives
Image: Four ascending steps show the learning objectives:
- Recognize the importance of effective communication.
- Identify barriers to communication.
- Describe the connection between communication and medical errors.
- Identify and apply effective communication strategies from CUSP and TeamSTEPPS®.
Slide 3: Basic Components and Process of Communication1
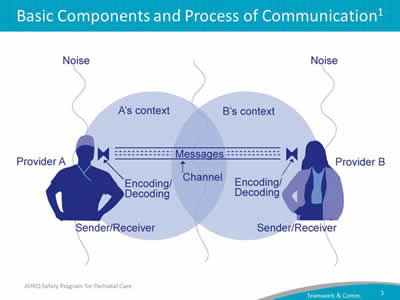
Image: This slide shows a blue silhouette illustration of two health care professionals, a man on the left in his circle (Provider A and A's context) and a woman on the right in her circle (Provider B and B's context). Messages flow back and forth between them (the "Channel") and each person ("Sender/Receiver") is engaged in encoding and decoding these messages. There is outside "noise" pictured entering each Provider's field of communication, which can interfere with the context and clarity of the message.
Graphic description of the basic components and process of communication. The communication that takes place between two people is exposed to many roadblocks in between its transmission from one individual to another. First, the message is encoded, or created, by the sender who then transmits the message to the receiver, who then must decode, or process, the message. While the message is being transmitted, it is exposed to noise interference that impacts the context and clarity of the message that is sent and received.
Slide 4: Four Key Components of Effective Communication2
Images: Effective communication is complete, clear, brief, and timely. TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 5: Elements That Affect Communication and Information Exchange
- Interruptions.
- Task absorption.
- Verbal abuse.
- Fatigue.
- Not following plan of care.
- Ambiguous orders or directions.
- Change in team members.
- Work load.
- Language barriers.
Image: Team members separated by barrier representing possible challenges to disrupting effective communication.
Slide 6: Root Causes of Maternal and Perinatal Deaths and Injuries 2004-20123
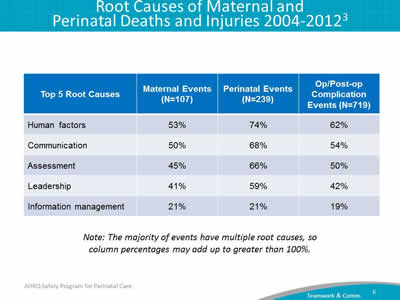
| Top 5 Root Causes | Maternal Events (N=107) | Perinatal Events (N=239) | Op/Post-op Complication Events (N=719) |
|---|---|---|---|
| Human factors | 53% | 74% | 62% |
| Communication | 50% | 68% | 54% |
| Assessment | 45% | 66% | 50% |
| Leadership | 41% | 59% | 42% |
| Information management | 21% | 21% | 19% |
Note: The majority of events have multiple root causes, so column percentages may add up to greater than 100%.
Slide 7: Barriers to Team Effectiveness2
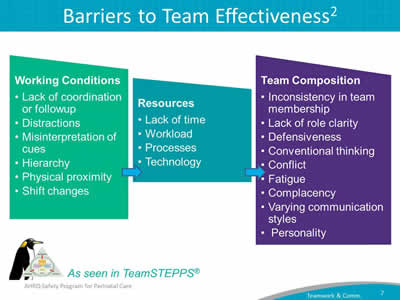
Images: Environmental barriers include: lack of coordination or follow up, distractions, misinterpretation of cues, hierarchy, lack of clarity on roles and responsibilities, physical proximity and shift changes.
Resource barriers include lack of time, workload, processes and technology.
Team composition barriers include inconsistency in team membership, lack of role clarity, defensiveness, conventional thinking, conflict, fatigue, complacency, varying communication styles and personality.
TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 8: Positive Outcomes of Effective Teamwork on Health Care4
- Reduced length of stay.
- Higher quality of care.
- Better patient outcomes.
- Greater ability to meet family member needs.
- Improved patient experience with care scores.
- Lower nurse turnover.
Image: A nurse and physician collaborating beside their patient and the patient's family member.
Slide 9: Shadowing
Helps—
- Team members gain perspective of other roles.
- Identify issues affecting teamwork and communication that may affect patient care, patient care delivery, and outcomes.
Who should shadow?
- Staff of patient care units where culture scores indicate a poor score in teamwork and safety.
- Units with little collaboration between disciplines.
Slide 10: Selected TeamSTEPPS Tools2
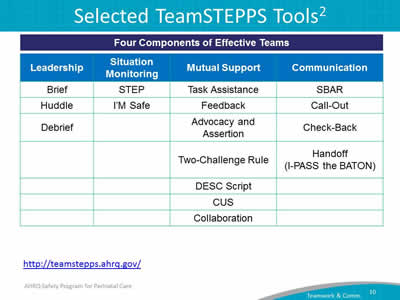
| Leadership | Situation Monitoring | Mutual Support | Communication |
|---|---|---|---|
| Brief | STEP | Task Assistance | SBAR |
| Huddle | I’M Safe | Feedback | Call-Out |
| Debrief | Advocacy and Assertion | Check-Back | |
| Two-Challenge Rule | Handoff (I-PASS the BATON) |
||
| DESC Script | |||
| CUS | |||
| Collaboration |
https://www.ahrq.gov/teamstepps-program/index.html
Slide 11: Briefing1,2
A briefing is a discussion between two or more people, often a team, using succinct information pertinent to an event. A briefing immediately—
- Maps out the care plan.
- Identifies each team member's role and responsibilities.
- Heightens awareness of the situation.
- Permits the team to plan for the unexpected.
- Allows team members' needs and expectations to be met.
- Sets the tone for the day.
- Encourages team members' participation.
Images: Silhouette drawing, in shades of blue, of four medical professionals standing in a group and conferring. TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 12: Huddle1,2
- Employs ad hoc planning to re-establish situational awareness, reinforce plans that are already in place, and assess any need to adjust the plan.
- Gathers team members to review patient data and decide on a course of action.
- Can be requested by any team member at any time.
- Frequently uses the SBAR tool (a framework for effective communication).
Images: Group of doctors huddled together. And TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 13: Debriefing1,2
Informal information exchange session designed to improve team performance and effectiveness after each review.
Debriefings Answer:
- What went well?
- What did we learn?
- What do we need to improve or change for next time?
Debriefing Checklist:
- Is communication clear?
- Are roles and responsibilities understood?
- Is situational awareness maintained?
- Is the workload distributed equally?
- Is task assistance requested or offered?
- Were errors made or avoided?
- Are resources available?
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 14: STEP2
- Status of the patient.
- Team members.
- Environment.
- Progress toward goal.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®
Slide 15: I'm Safe2
- I - illness.
- M - medication.
- S - stress.
- A - alcohol and drugs.
- F - fatigue.
- E - eating and elimination.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 16: Task Assistance2
- Team members protect each other from work overload situations.
- Effective teams place all offers and requests for assistance in the context of patient safety.
- Team members foster a climate where it is expected that assistance will be actively sought and offered.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 17: Feedback2
- Timely—given soon after the target behavior has occurred.
- Respectful—focus on behaviors, not personal attributes.
- Specific—be specific about what behaviors need correcting.
- Directed toward improvement—provide directions for future improvement.
- Considerate—consider a team member's feelings and deliver negative information with fairness and respect.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 18: Advocacy and Assertion2
- Advocacy and assertion are used to support the patient when a team member's viewpoints do not coincide with those of the decision maker.
- When advocating for the patient, team members should assert their opinion in a firm and respectful manner, providing evidence or data to support their concerns.
- An assertive statement should—
- Open the discussion.
- State the concern.
- State the problem—real or perceived.
- Offer a solution.
- Obtain an agreement.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 19: Two-Challenge Rule2
- Used when there is an information conflict and an initial assertion is ignored.
- Rule requires team members to state their observation at least twice to ensure that their interests and observations are being addressed.
- The Two-Challenge Rule empowers any team member to stop the action if he or she senses, or discovers, an essential safety breach that hinders patient well-being.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 20: DESC Script1
A constructive approach for handling and managing personal conflict, the DESC script helps unit teams resolve these disputes.
- Describe the specific situation.
- Express your concerns about the action.
- Suggest other alternatives.
- Consensus should be stated.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 21: CUS1
I am CONCERNED!
I am UNCOMFORTABLE!
This is a SAFETY ISSUE!
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 22: Collaboration1
- Achieves a mutually satisfying solution resulting in the best outcome.
- Win-Win-Win for patient care team (includes the patient, team members, and team).
- Commitment to a common mission.
- Meets goals without compromising relationships.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 23: SBAR1,2
Provides a framework for effective communication between team members for the following information—
- Situation―What is happening with the patient?
- Background―What is the clinical background or context?
- Assessment―What do I think the problem is?
- Recommendation―What would I recommend?
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 24: Callout2
A strategy to communicate critical information to all team members to prepare them for upcoming procedures.
- Informs all team members simultaneously.
- Helps team members anticipate next steps.
- Directs responsibility to a specific individual accountable for carrying out the task.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 25: Check-Back1,2
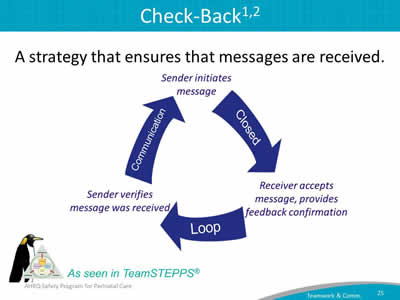
A strategy that ensures that messages are received.
Images: Diagram illustrates a strategy that ensures that messages are received. The diagram shows a communication loop with three large blue arrows roughly arranged in a circular pattern. The left arrow points up and says, "Communication," when "Sender initiates message." The right arrow points down and says, "Closed," when "Receiver accepts message, provides feedback confirmation." The bottom arrow in the pattern points left and says, "Loop," when "Sender verifies message was received."
Diagram depicting how check back works:
The sender initiates a message to the receiver, who loops back their understanding and feedback to the sender. The sender then verifies that the message was received.
TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 26: Handoff1
- Transfer of information, along with authority and responsibility, during transitions in care across the continuum.
- Includes an opportunity to ask questions, clarify, and confirm.
- Tool used: I PASS the BATON:
- Introduction.
- Patient.
- Assessment.
- Situation.
- Safety Concern.
- Background.
- Actions.
- Timing.
- Ownership.
- Next.
Images: Two doctors talking together. TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 27: Situational Awareness1
When team members have situational awareness, they—
- Know the game plan through briefings and team management (e.g., workload and workflow management, task coordination, policies, and procedures).
- Have an understanding of what's going on and what is likely to happen next.
- Check back and verify information.
- Provide ongoing updates—briefings, callouts, and check-backs.
- Implement team huddles.
Image: TeamSTEPPS logo and penguin—as seen in TeamSTEPPS®.
Slide 28: Implement Teamwork and Communication: What the Team Needs To Do
- Identify opportunities to improve teamwork and communication by reviewing barriers the team identified while learning from a safety defect.
- Discuss with frontline providers how and where they want to improve communication.
- Select a tool that best addresses providers' concerns.
- Use teamwork and communication tools and incorporate them into team meetings and other relevant project processes.
Slide 29: Additional CUSP Tools
- Team Checkup Tool.
- Culture Checkup Tool.
Slide 30: Summary
- Effective communication plays an integral role in the delivery of high-quality, patient-centered care.
- Barriers to efficient teamwork and communication influence the outcomes of the unit team.
- Research supports the connection between communication errors and patient care delivery.
- CUSP and TeamSTEPPS employ successful tools and strategies that unit teams can implement to improve the effectiveness of teamwork and communication on their units.
Slide 31: References
- (Adapted from) Dayton E, Henriksen K. Communication failure: basic components, contributing factors, and the call for structure. Joint Commission Journal of Quality and Patient Safety 2007 Jan;33(1):34-47. PMID: 17283940.
- Agency for Healthcare Research and Quality, Department of Defense. TeamSTEPPS. https://www.ahrq.gov/teamstepps-program/index.html
- Joint Commission on Accreditation of Healthcare Organizations. Sentinel Events Statistics. Root Causes of Sentinel Events, 2005. http://www.jointcommission.org/sentinel_event.aspx.
- Shortell SM, Marstellar JA, Lin M et al. The role of perceived team effectiveness in improving chronic illness care. Med Care 2004 Nov; 42:1040-1048. PMID: 15586830.
Slide 32: Disclaimers

Every effort was made to ensure the accuracy and completeness of this resource. However, the U.S. Department of Health and Human Services makes no warranties regarding errors or omissions and assumes no responsibility or liability for loss or damage resulting from the use of information contained within.
The U.S. Department of Health and Human Services cannot endorse, or appear to endorse derivate or excerpted materials, and it cannot be held liable for the content or use of adapted resources. Any adaptations of this resource must include a disclaimer to this effect.
Reference to any specific commercial products, process, service, manufacturer, company, or trademark does not constitute endorsement or recommendation by the U.S. Government, HHS, or AHRQ of the linked Web resources or the information, products, or services contained therein. The Agency does not exercise any control over the content on these sites.



