Learn About the Comprehensive Unit-based Safety Program for Perinatal Safety
AHRQ Safety Program for Perinatal Care
Slide 1: AHRQ Safety Program for Perinatal Care
Learn About the Comprehensive Unit-based Safety Program for Perinatal Safety
Slide 2: CUSP and Perinatal Safety
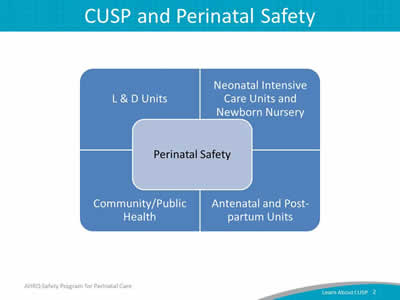
Image: A chart is shown with "Perinatal Safety" at the center. There are four sections of the chart surrounding "Perinatal Safety." They are: "L & D Units," "Neonatal Intensive Care Units and Newborn Nursery," "Community/Public Health," and "Antenatal and Postpartum Units."
Slide 3: Learning Objectives
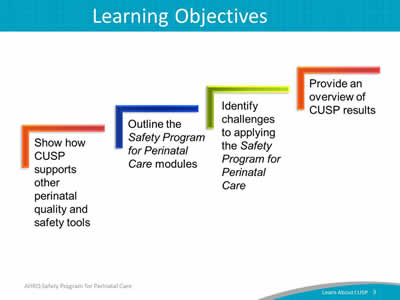
Image: Four ascending steps show the learning objectives:
- Show how CUSP supports other perinatal quality and safety tools.
- Outline the Safety Program for Perinatal Care modules designed for this program.
- Identify challenges to applying the Safety Program for Perinatal Care.
- Provide an overview of CUSP results.
Slide 4: Is Your Hospital Safe?
- Would you want a loved one to be a patient at your hospital? Your unit?
- Would you want to be a patient in the unit where you work?
- Can you say with 100 percent certainty that you believe that your hospital does everything it can to protect its patients?
Slide 5: Safety Program for Perinatal Care
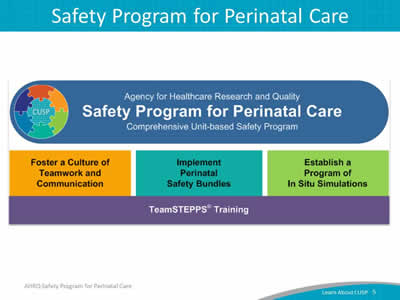
Image: Built on the foundation of TeamSTEPPS training, the AHRQ Safety Program for Perinatal Care or SPPC is built around three program pillars:
- Foster a culture of teamwork and communication.
- Implement perinatal safety bundles.
- Establish a program of in situ simulations.
The first program pillar provides general principles and approaches to fostering unit-based approaches for patient safety related to teamwork and communication. CUSP is the framework for this program pillar.
Slide 6: SPPC CUSP Modules
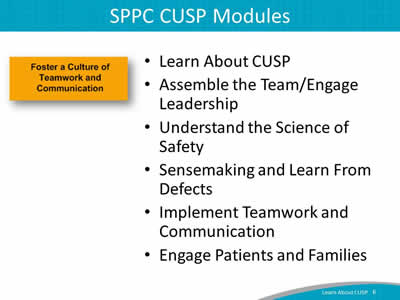
- Learn About CUSP.
- Assemble the Team/Engage Leadership.
- Understand the Science of Safety.
- Sensemaking and Learn From Defects.
- Implement Teamwork and Communication.
- Engage Patients and Families.
Foster a culture of teamwork and communication.
Slide 7: CUSP Aligns With and Supports Other Quality and Safety Tools
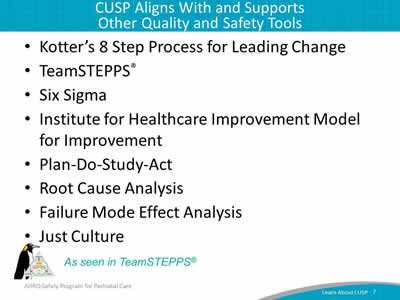
- Kotter's 8 Step Process for Leading Change.
- TeamSTEPPS®.
- Six Sigma.
- Institute for Healthcare Improvement Model for Improvement.
- Plan-Do-Study-Act.
- Root Cause Analysis.
- Failure Mode Effect Analysis.
- Just Culture.
Image: TeamSTEPPS penguin and logo—as seen in TeamSTEPPS®.
Slide 8: The CUSP Model
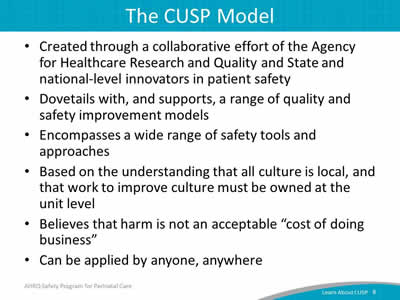
- Created through a collaborative effort of the Agency for Healthcare Research and Quality and State and national-level innovators in patient safety.
- Dovetails with, and supports, a range of quality and safety improvement models.
- Encompasses a wide range of safety tools and approaches.
- Based on the understanding that all culture is local, and that work to improve culture must be owned at the unit level.
- Believes that harm is not an acceptable "cost of doing business".
- Can be applied by anyone, anywhere.
Slide 9: A Collaborative Effort1
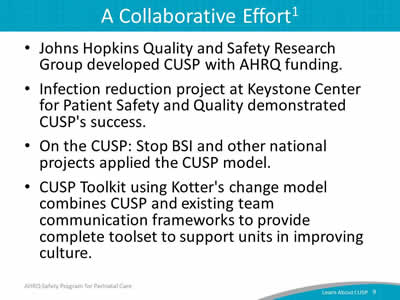
- Johns Hopkins Quality and Safety Research Group developed CUSP with AHRQ funding.
- Infection reduction project at Keystone Center for Patient Safety and Quality demonstrated CUSP's success.
- On the CUSP: Stop BSI and other national projects applied the CUSP model.
- CUSP Toolkit using Kotter's change model combines CUSP and existing team communication frameworks to provide complete toolset to support units in improving culture.
Slide 10: CUSP Supports Kotter's Eight Steps of Change2
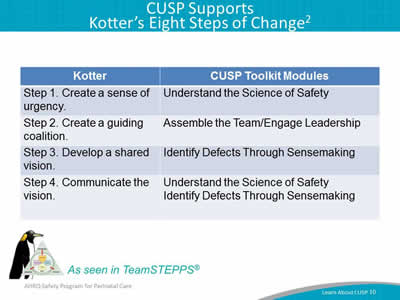
| Kotter | CUSP Toolkit Modules |
|---|---|
| Step 1. Create a sense of urgency. | Understand the Science of Safety |
| Step 2. Create a guiding coalition. | Assemble the Team/Engage Leadership |
| Step 3. Develop a shared vision. | Identify Defects Through Sensemaking |
| Step 4. Communicate the vision. | Understand the Science of Safety Identify Defects Through Sensemaking |
Image: TeamSTEPPS penguin and logo—as seen in TeamSTEPPS®.
Slide 11: CUSP Supports Kotter's Eight Steps of Change2
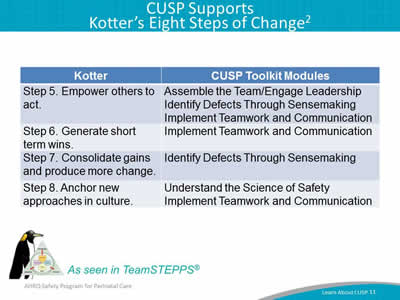
| Kotter | CUSP Toolkit Modules |
|---|---|
|
Step 5. Empower others to act. |
Assemble the Team/Engage Leadership Identify Defects Through Sensemaking Implement Teamwork and Communication |
|
Step 6. Generate short term wins. |
Implement Teamwork and Communication |
|
Step 7. Consolidate gains and produce more change. |
Identify Defects Through Sensemaking |
|
Step 8. Anchor new approaches in culture. |
Understand the Science of Safety Implement Teamwork and Communication |
Image: TeamSTEPPS penguin and logo—as seen in TeamSTEPPS®.
Slide 12: Introduction to Just Culture Principles
Introduction to Just Culture Principle
Slide 13: Understand Just Culture
Image: Opening shot of Just Culture video with the words "Click to play".
Go to Link Below To Play Video:
http://www.ahrq.gov/professionals/education/curriculum-tools/cusptoolkit/videos/07a_just_culture/index.html
Slide 14: Just Culture3
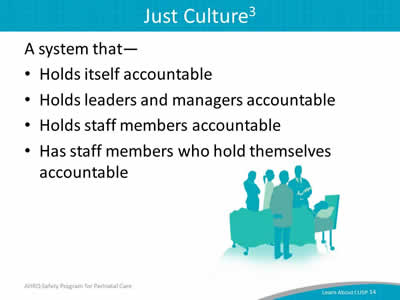
A system that—
- Holds itself accountable.
- Holds leaders and managers accountable.
- Holds staff members accountable.
- Has staff members who hold themselves accountable.
Image: A patient in a hospital bed surrounded by the health care team.
Slide 15: Understanding Risk and Human Behavior3
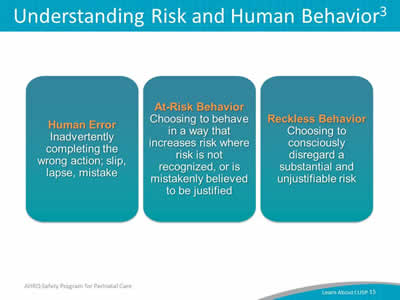
Image: Human Error refers to inadvertently doing something other than what should have been done, such as a slip, lapse, or mistake. At-risk behavior entails choosing to behave in a way that increases risk where risk isn't recognized, or is mistakenly believed to be justified. Reckless behavior is a choice to consciously disregard a substantial and unjustifiable risk.
Slide 16: Managing Error and Risk3
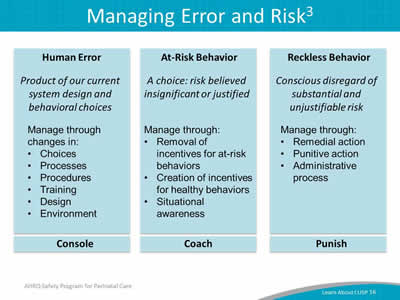
Image: Three text boxes contain the following:
Human Error
Product of our current system design and behavioral choices.
Manage through changes in:
- Choices
- Processes
- Procedures
- Training
- Design
- Environment.
Console
At-Risk Behavior
A choice: risk believed insignificant or justified.
Manage through:
- Removal of incentives for at-risk behaviors.
- Creation of incentives for healthy behaviors.
- Situational awareness.
Coach
Reckless Behavior
Conscious disregard of substantial and unjustifiable risk.
Manage through:
- Remedial action
- Punitive action
- Administrative process.
Punish
Slide 17: Systems and Behaviors Work Together To Improve Outcomes3
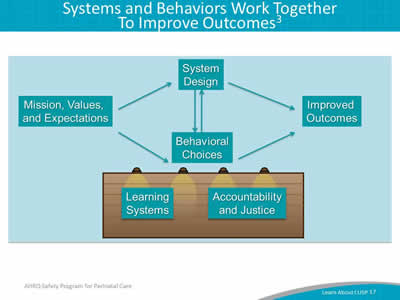
Image: Both system design and behavioral choices have an impact on patient safety. Learning systems, like mission values and expectations, impact system design and in turn, behavioral choices. These inputs also influence the accountability and justice of the environment to bring about improved outcomes.
Slide 18: Systems and Behaviors Work Together To Improve Outcomes3
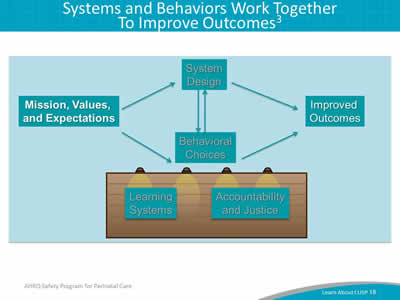
Image: Both system design and behavioral choices have an impact on patient safety. Learning systems, like mission values and expectations, impact system design and in turn, behavioral choices. These inputs also influence the accountability and justice of the environment to bring about improved outcomes.
Slide 19: Systems and Behaviors Work Together To Improve Outcomes3
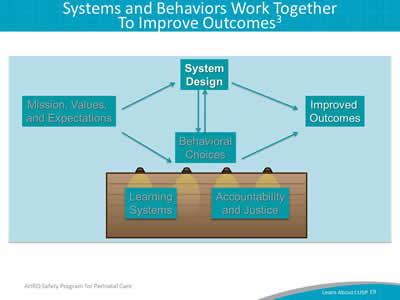
Image: Both system design and behavioral choices have an impact on patient safety. Learning systems, like mission values and expectations, impact system design and in turn, behavioral choices. These inputs also influence the accountability and justice of the environment to bring about improved outcomes.
Slide 20: Systems and Behaviors Work Together To Improve Outcomes3
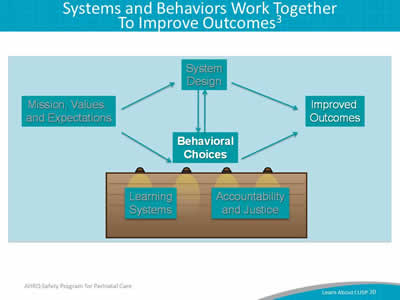
Image: Both system design and behavioral choices have an impact on patient safety. Learning systems, like mission values and expectations, impact system design and in turn, behavioral choices. These inputs also influence the accountability and justice of the environment to bring about improved outcomes.
Slide 21: Systems and Behaviors Work Together To Improve Outcomes3
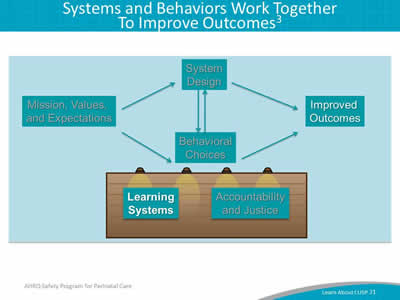
Image: Both system design and behavioral choices have an impact on patient safety. Learning systems, like mission values and expectations, impact system design and in turn, behavioral choices. These inputs also influence the accountability and justice of the environment to bring about improved outcomes.
Slide 22: Systems and Behaviors Work Together To Improve Outcomes3
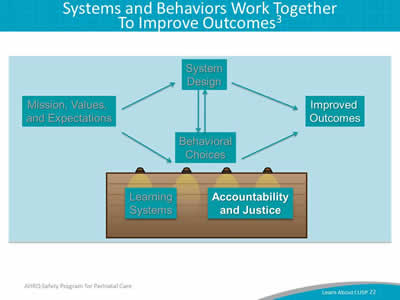
Image: Both system design and behavioral choices have an impact on patient safety. Learning systems, like mission values and expectations, impact system design and in turn, behavioral choices. These inputs also influence the accountability and justice of the environment to bring about improved outcomes.
Slide 23: Engineering System Design To Support Behavior Choices3
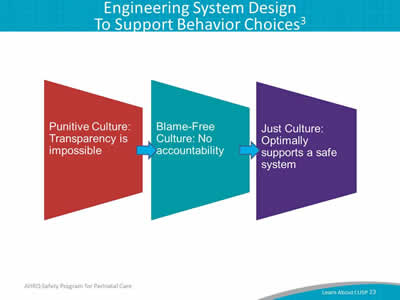
Image: Three trapezoids are shown in a sequence, with arrows pointing from one to the next. They are captioned (from left to right):
Punitive culture: transparency is impossible.
Blame-free culture: no accountability.
Just culture: optimally supports a system of safety.
Slide 24: Leadership Team's Role in Applying Just Culture Principles
- Have a procedure in place for employees to follow.
- Ensure employees are properly trained and have clear expectations.
- Offer positive reinforcement at the monthly Learning From Defects meeting.
Slide 25: CUSP Is Compatible With TeamSTEPPS4
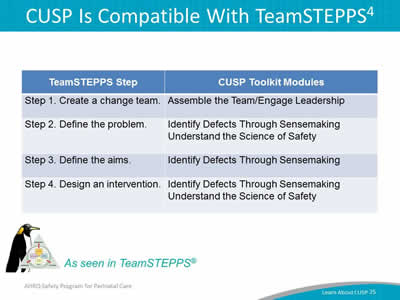
| TeamSTEPPS Step | CUSP Toolkit Modules |
|---|---|
| Step 1. Create a change team. | Assemble the Team/Engage Leadership |
| Step 2. Define the problem. | Identify Defects Through Sensemaking Understand the Science of Safety |
| Step 3. Define the aims. | Identify Defects Through Sensemaking |
| Step 4. Design an intervention. | Identify Defects Through Sensemaking Understand the Science of Safety |
Image: TeamSTEPPS penguin and logo—as seen in TeamSTEPPS®.
Slide 26: CUSP is Compatible With TeamSTEPPS4
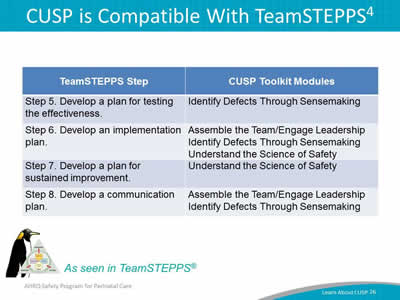
| TeamSTEPPS Step | CUSP Toolkit Modules |
|---|---|
| Step 5. Develop a plan for testing the effectiveness. | Identify Defects Through Sensemaking |
| Step 6. Develop an implementation plan. | Assemble the Team/Engage Leadership Identify Defects Through Sensemaking Understand the Science of Safety |
| Step 7. Develop a plan for sustained improvement. | Understand the Science of Safety |
| Step 8. Develop a communication plan. | Assemble the Team/Engage Leadership Identify Defects Through Sensemaking |
Image: TeamSTEPPS penguin and logo—as seen in TeamSTEPPS®.
Slide 27: CUSP Results
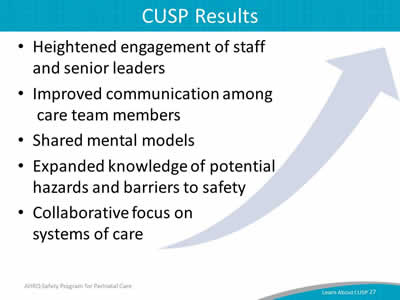
- Heightened engagement of staff and senior leaders.
- Improved communication among care team members.
- Shared mental models.
- Expanded knowledge of potential hazards and barriers to safety.
- Collaborative focus on systems of care.
Slide 28: Summary
- CUSP integrates with and supports a broad range of quality and safety models.
- Communication is cited as a root cause of most errors.
- Individuals across an organization can use CUSP and expect measurable results.
Slide 29: References
- Health Research & Educational Trust, Johns Hopkins University Quality and Safety Research Group, Michigan Health & Hospital Association Keystone Center for Patient Safety and Quality. Eliminating CLABSI: A National Patient Safety Imperative. A Progress Report on the National On the CUSP: Stop BSI Project. AHRQ Publication No. 11-0037-EF. Rockville, MD: Agency for Healthcare Research and Quality; April 2011.
- Kotter J, Rathgeber H. Our Iceberg Is Melting: Changing and Succeeding Under Any Conditions: 1st ed. New York; St. Martin's Press; 2006.
- Griffith S. Just Culture. Plano, TX: Outcome Engineering; 2011.
- Agency for Healthcare Research and Quality, Department of Defense. TeamSTEPPS. http://www.ahrq.gov/teamstepps/index.html.
Slide 30: Disclaimers
Every effort was made to ensure the accuracy and completeness of this resource. However, the U.S. Department of Health and Human Services makes no warranties regarding errors or omissions and assumes no responsibility or liability for loss or damage resulting from the use of information contained within.
The U.S. Department of Health and Human Services cannot endorse, or appear to endorse derivate or excerpted materials, and it cannot be held liable for the content or use of adapted resources. Any adaptations of this resource must include a disclaimer to this effect.
Reference to any specific commercial products, process, service, manufacturer, company, or trademark does not constitute endorsement or recommendation by the U.S. Government, HHS, or AHRQ of the linked Web resources or the information, products, or services contained therein. The Agency does not exercise any control over the content on these sites.



