On This Page:
- Slide 1. Facts About Falls
- Slide 2. Facts About Falls (continued)
- Slide 3. Facts About Falls (continued)
- Slide 4. Intrinsic Fall Risk Factors
- Slide 5. Intrinsic Fall Risk Factors (continued)
- Slide 6. Intrinsic Fall Risk Factors (continued)
- Slide 7. Extrinsic Fall Risk Factors
- Slide 8. Extrinsic Fall Risk Factors (continued)
- Slide 9. Extrinsic Fall Risk Factors (continued)
- Slide 10. Physical Restraints
- Slide 11. Consequences of Falls
- Slide 12a. Staff Strategies to Reduce Fall Risk
- Slide 12b. Staff Strategies to Reduce Fall Risk (continued)
- Slide 13. How You Can Help
- Slide 14. Remove Clutter
- Slide 15. Provide Safe Footwear
- Slide 16. Promote Safety During Transfer
- Slide 17. Use Low Blood Pressure Precautions
Slide 1. Facts About Falls

Opening slide of this Falls Management Program presentation.
Slide 2 Facts About Falls (continued)
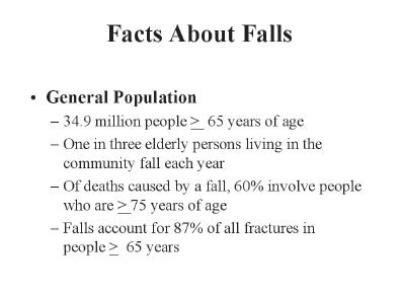
- General Population
- 34.9 million people ≥65 years of age
- One in three elderly persons living in the community fall each year
- Of deaths caused by a fall, 60% involve people who are ≥75 years of age
- Falls account for 87% of all fractures in people ≥65 years of age
Slide 3. Facts About Falls (continued)
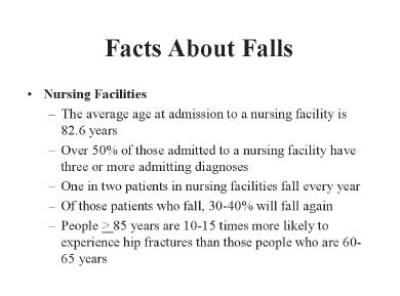
- Nursing Facilities
- The average age at admission to a nursing facility is 82.6 years
- Over 50% of those admitted to a nursing facility have three or more admitting diagnoses
- One in two patients in nursing facilities fall every year
- Of those patients who fall, 30-40% will fall again
- People ≥85 years are 10-15 times more likely to experience hip fractures than those people who are 60-65 years
Slide 4. Intrinsic Fall Risk Factors
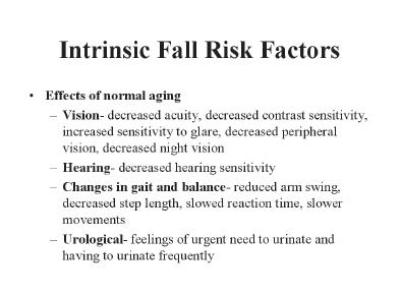
- Effects of Normal Aging
- Vision - decreased acuity, decreased contrast sensitivity, increased sensitivity to glare, decreased peripheral vision, decreased night vision
- Hearing - decreased hearing sensitivity
- Changes in gait and balance - reduced arm swing, decreased step length, slowed reaction time, slower movements
- Urological - feelings of urgent need to urinate and having to urinate frequently
Slide 5. Intrinsic Fall Risk Factors (continued)
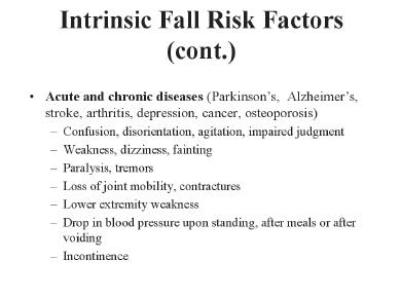
- Acute and Chronic Diseases (Parkinson's, Alzheimer's, stroke, arthritis, depression, cancer, osteoporosis)
- Confusion, disorientation, agitation, impaired judgment
- Weakness, dizziness, fainting
- Paralysis, tremors
- Loss of joint mobility, contractures
- Lower extremity weakness
- Drop in blood pressure upon standing, after meals or after voiding
- Incontinence
Slide 6. Intrinsic Fall Risk Factors (continued)
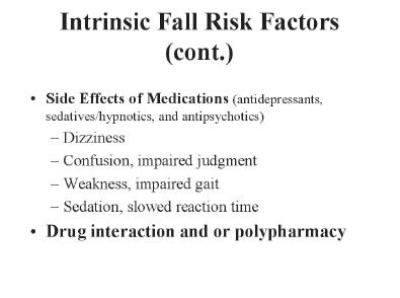
- Side Effects of Medications (antidepressants, sedatives/hypnotics, and antipsychotics)
- Dizziness
- Confusion, impaired judgment
- Weakness, impaired gait
- Sedation, slowed reaction time
- Drug interaction and/or polypharmacy
Slide 7. Extrinsic Fall Risk Factors
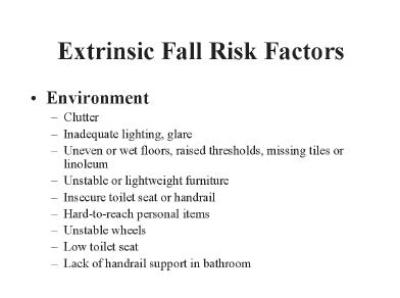
- Environment
- Clutter
- Inadequate lighting, glare
- Uneven or wet floors, raised thresholds, missing tiles or linoleum
- Unstable or lightweight furniture
- Insecure toilet seat or handrail
- Hard-to-reach personal items
- Unstable wheels
- Low toilet seat
- Lack of handrail support in bathroom
Slide 8. Extrinsic Fall Risk Factors (continued)
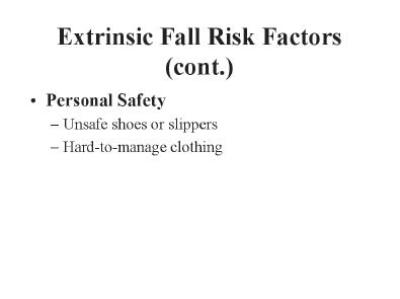
- Personal Safety
- Unsafe shoes or slippers
- Hard-to-manage clothing
Slide 9. Extrinsic Fall Risk Factors (continued)
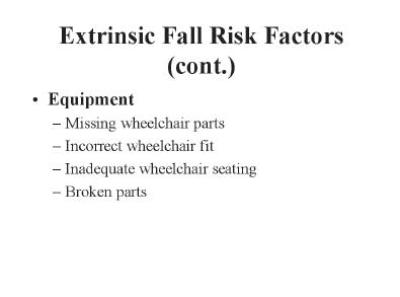
- Equipment
- Missing wheelchair parts
- Incorrect wheelchair fit
- Inadequate wheelchair seating
- Broken parts
Slide 10. Physical Restraints
Physical restraints increase the likelihood of serious injury resulting from a fall.
Not a method of fall prevention
Slide 11. Consequences of Falls
- Serious injury such as hip fracture
- Increased risk of death associated with hospitalization and complications
- Loss of independence and decreased ability to function
- Loss of self-confidence and fear of falling
- Reduced quality of life
- Increased need for care
Slide 12a. Staff Strategies To Reduce Fall Risk
- Falls assessment to determine problems with medications, behavior, vision, gait, and mobility, or presence of postural hypotension
- Medical evaluation
- Medication review
- Gait and balance training
Slide 12b. Staff Strategies To Reduce Fall Risk (continued)
- Hip protectors
- Individualized wheelchair seating
- Low beds, mats
- ½ or ¼ side rails
- Toileting
- Alarms/sensors
- Activities and exercise programs
- Behavioral strategies
Slide 13. How You Can Help
- Remove clutter from room and bathroom
- Provide safe shoes and slippers
- Promote safety during transfer and bathroom use
- Use low blood pressure precautions when needed
Remove clutter from room and bathroom - Provide safe shoes and slippers - Promote safety during transfer and bathroom use - Use low blood pressure precautions when needed
Slide 14. Remove Clutter
- Help keep pathways around bed and to bathroom clear
- Provide only stable furniture from home
- Remove items no longer needed
Slide 15. Provide Safe Footwear
- Shoes and slippers should have tread, fit well, have a firm shape, and have low, even heels.
Examples: tennis shoes with Velcro fasteners, oxford style shoes, canvas or leather slip-on shoes, fitted, soft slippers with tread.
Slide 16. Promote Safety During Transfer
- Call for help when unsure about safety
- Provide easy-to-manage clothing with elastic waist and Velcro fasteners
- Lock wheelchair brakes before transfer
- Keep all seating items in wheelchair
Slide 17. Use Low Blood Pressure Precautions
For residents with low blood pressure:
- Sit on edge of bed and dangle feet before rising
- Flex feet backwards several times before rising
- Do not tilt head backwards
- Get up slowly and use assistance - Report dizziness



