System Redesign for Value in Safety-Net Hospitals and Systems: Challenges and Implications
Slide Presentation
Slide 1
System Redesign for Value in Safety-Net Hospitals and Systems: Challenges and Implications
Boston University School of Public Health
prepared for
Agency for Healthcare Research and Quality
ACTION II
The work reported here was done under AHRQ ACTION II Task Order Contract No. HHSA2902010000291 TO1. The views expressed here are solely those of the authors and do not represent any U.S. government agency or any institutions with which the authors are affiliated.
Note: For further information on this study, go to http://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/system/systemredesignsafetynet/systemredesign.pdf and http://healthaffairs.org/blog/2015/03/16/can-safety-net-hospital-systems-redesign-themselves-to-achieve-financial-viability/.
Slide 2

Presenters
- Michael I. Harrison, Ph.D.
Senior Social Scientist, Organizations and Systems
Center for Delivery, Organization, and Markets
Agency for Healthcare Research and Quality
- Carol VanDeusen Lukas, Ed.D.
Clinical Associate Professor
Department of Health Policy and Management
Boston University School of Public Health
Senior Investigator
Center for Healthcare Organization and Implementation Research
Department of Veterans Affairs
Images: Photographs of Michael I. Harrison and Carol VanDeusen Lukas.
Slide 3
Overview of this session
- Highlight challenges safety-net hospital systems face in the current health care environment.
- Suggest actions for federal agencies and private organizations to consider to support safety-net systems (SNSs).
- Discuss conclusions and potential strategies to address challenges.
Slide 4
AHRQ objectives in commissioning this project
- Learn more about how to foster effective and sustainable system redesign to increase value in SNSs.
- Identify external supports that SNSs are currently using.
- Identify additional forms of redesign support for consideration by government agencies and other external organizations.
Slide 5
Safety-net systems*
- Hospitals and their affiliated facilities and practices that:
- Serve high proportions of low-income, medically vulnerable patients.
- Have the highest shares of Medicaid and uninsured patients and lowest shares of privately insured patients in comparison with other U.S. hospital systems.
- Include but are not limited to publicly owned hospital systems.
* Institute of Medicine, Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press. 2001.
Slide 6
System redesign
- Improvement or redesign work that promotes alignment and synergy among quality improvement efforts to create changes that are well aligned across units and conditions.
- Coordinated multidimensional changes in management and delivery of care.
Strategic system redesign:
- Involves systemwide efforts to change the organization in ways that:
- Are aligned with strategic and business priorities.
- Support safety-net mission.
- Aim to enhance (or at least to preserve) the organization's competitive position.
Slide 7
Study team
- Boston University School of Public Health:
- Carol VanDeusen Lukas, Ed.D.
- Sally K. Holmes, M.B.A.
- Elisa Koppelman, M.P.H., M.S.W.
- Martin P. Charns, D.B.A.
- Cara Frigand, M.S.
- Gouri Gupte, Ph.D.
- Natasha Neal, M.P.H.
- Cambridge Health Alliance:
- Karen Hacker, M.D., M.P.H.
- Leah Zallman, M.D., M.P.H.
- Adriana Bearse, M.S.
- AHRQ Task Order Officer:
- Michael I. Harrison, Ph.D.
Slide 8
Study design
- Field studies of 8 SNSs:
- 7 urban, academic.
- 3 public.
- Outpatients visits per year: 374,000 - 1,850,000.
- Admissions per year: 12,000 - 82,000.
- Data collection: Oct 2012 to March 2013.
- Conversations with:
- Other SNSs.
- Resource providers.
- Industry leaders.
- Review of:
- Peer-reviewed literature.
- Gray literature—continuing updates.
- Guidance from an expert and stakeholder panel.
Slide 9

Expert and stakeholder panel members
Allison Bayer, M.B.A.
Executive Vice President and Chief Operating Officer
Cambridge Health Alliance
Michael Davies, M.D.
National Director for Systems Redesign
Department of Veterans Affairs
Jose L. Gonzalez, M.D., J.D., M.S.Ed.
Medical Director, Cook Children's Health Plan
Sandral Hullett, M.D., M.P.H.
Former CEO and Medical Director
Jefferson Health System/Cooper Green Hospital
Arnold Kaluzny, Ph.D.
Professor Emeritus of Health Policy and Management
Director Emeritus of Public Health Leadership Program
UNC Gillings School of Global Public Health
Uma R. Kotagal, M.D.
Senior Vice President for Safety Quality and Transformation Cincinnati Children's Hospital Medical Center
Lori Melichar, M.A., Ph.D.
Senior Program Officer
Robert Wood Johnson Foundation
John Oswald, Ph.D., M.P.H.
Assistant Vice President, Research
America's Essential Hospitals
(Formerly National Association of Public Hospitals and Health Systems)
Lillian Shirley, B.S.N., M.P.H., M.P.A.
Director
Multnomah County Health Department
Bruce Siegel, M.D., M.P.H.
President and Chief Executive Officer
America's Essential Hospitals
Slide 10

Safety-net external environment
- External forces drive leaders' decisions about business strategy and system design.
- SNSs operate in a complex environment of:
- Health reform.
- Accountability to multiple organizations.
- Local market dynamics.
- Federal, state, and local funding.
- Myriad policies and regulations in the changing context of new payment and care delivery experiments.
Slide 11
Take-away conclusions
- As SNSs face increasing challenges, earlier solutions for success and survival may not work.
- Strategic redesign is needed to meet the challenges of the present environment.
- But strategic redesign may not be enough to bring SNSs to stable financial positions.
- External resources can assist in redesign efforts.
- Consensus is needed on the future role of SNSs.
Slide 12
As SNSs face increasing challenges, earlier solutions may not work
- SNSs have long coped with high demand for their services with limited funding.
- In the past SNSs found creative ways to keep afloat financially, often through negotiations and longstanding relationships with government payers.
- Now SNSs are challenged to adhere to new requirements, adjust funding streams, and reconfigure care in new ways.
Slide 13
Strategic redesign needed to meet the challenges of the present environment
- As first steps, SNSs need to:
- Redesign their care delivery and clinical processes to meet new requirements and expectations.
- Strengthen their operations and infrastructure to improve efficiency and capacity.
- Safety-net systems:
- Have long experience in process improvement using quality improvement tools.
- Are less likely to have experience and infrastructure for broader system redesign across departments and diseases, and linked to business strategies.
Slide 14
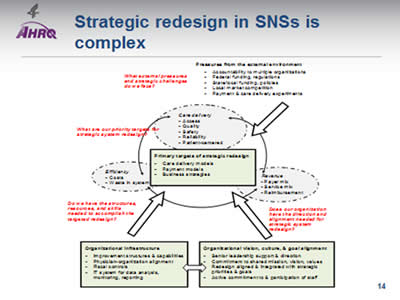
Strategic redesign in SNSs is complex
Image: Diagram showing safety-net system external environment, including, for example Federal and State funding and policies and market competition, as well as the interrelationship between care delivery, revenue, and efficiency. They're shown in a circle with two-way arrows between them. Also shown are elements of organizational capacity for system redesign, such as senior leadership support and staff commitment and organizational building blocks, such as financial controls and physician alignment. These interact with each other and influence the primary targets of redesign and improvement, which are business strategies, payment models, care delivery models, and process improvement.
Slide 15
Challenge 1: Underdeveloped system redesign capacity and improvement infrastructure
Potential strategies to address the challenge:
- Improve safety-net access to existing training and improvement resources by reducing financial barriers to entry.
- Examples: Offer sliding fee scales, discounts for groups, or more subsidized fellowships for safety-net institutions.
- Offer training that supports the development of improvement infrastructures and organizational capacity for strategic redesign.
- Example: Include theory and tools for organizational change and for improvement as a management philosophy).
Slide 16
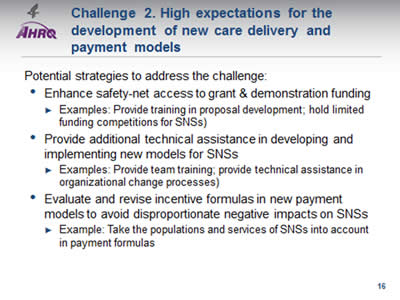
Challenge 2. High expectations for the development of new care delivery and payment models
Potential strategies to address the challenge:
- Enhance safety-net access to grant & demonstration funding.
- Examples: Provide training in proposal development; hold limited funding competitions for SNSs).
- Provide additional technical assistance in developing and implementing new models for SNSs.
- Examples: Provide team training; provide technical assistance in organizational change processes).
- Evaluate and revise incentive formulas in new payment models to avoid disproportionate negative impacts on SNSs.
- Example: Take the populations and services of SNSs into account in payment formulas.
Slide 17
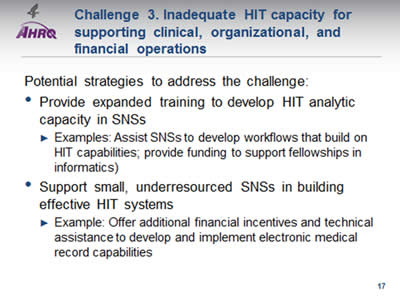
Challenge 3. Inadequate HIT capacity for supporting clinical, organizational, and financial operations
Potential strategies to address the challenge:
- Provide expanded training to develop HIT analytic capacity in SNSs.
- Examples: Assist SNSs to develop workflows that build on HIT capabilities; provide funding to support fellowships in informatics).
- Support small, underresourced SNSs in building effective HIT systems.
- Example: Offer additional financial incentives and technical assistance to develop and implement electronic medical record capabilities.
Slide 18
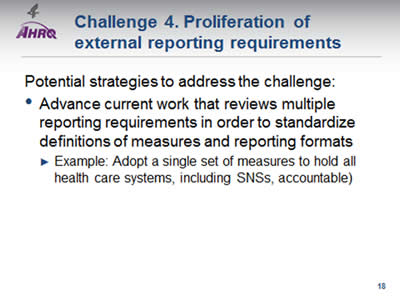
Challenge 4. Proliferation of external reporting requirements
Potential strategies to address the challenge:
- Advance current work that reviews multiple reporting requirements in order to standardize definitions of measures and reporting formats.
- Example: Adopt a single set of measures to hold all health care systems, including SNSs, accountable.
Slide 19
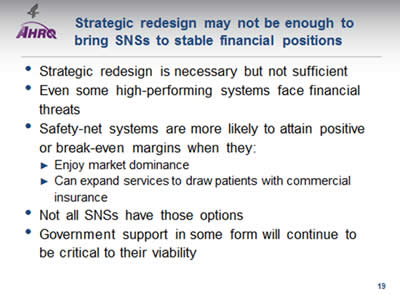
Strategic redesign may not be enough to bring SNSs to stable financial positions
- Strategic redesign is necessary but not sufficient.
- Even some high-performing systems face financial threats.
- Safety-net systems are more likely to attain positive or break-even margins when they:
- Enjoy market dominance.
- Can expand services to draw patients with commercial insurance.
- Not all SNSs have those options.
- Government support in some form will continue to be critical to their viability.
Slide 20
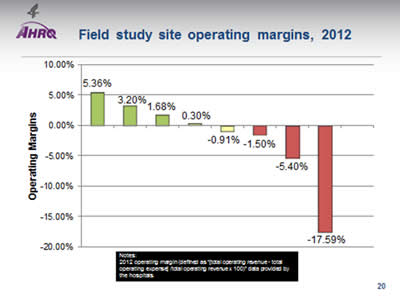
Field Study Site Operating Margins, 2012
Image: Chart shows operating margin for sites:
| Site | Operating Margins |
|---|---|
| Site H | 5.36% |
| Site E | 3.20% |
| Site G | 1.68% |
| Site F | 0.30% |
| Site C | -0.91% |
| Site B | -1.50% |
| Site D | -5.40% |
| Site A | -17.59% |
Notes: 2012 operating margin (defined as "[total operating revenue - total operating expense] /total operating revenue x 100)" data provided by the hospitals.
Slide 21
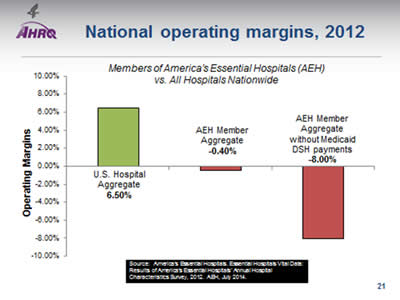
National Operating Margins, 2012
Image: Chart shows operating margins for Members of America's Essential Hospitals (AEH) vs. All Hospitals Nationwide:
| Hospital Aggregate | Operating Margin |
|---|---|
| U.S. Hospital Aggregate | 6.50% |
| AEH Member Aggregate | -0.40% |
| AEH Member Aggregate without Medicaid DSH payments | -8.00% |
Source: America's Essential Hospitals. Essential Hospitals Vital Data: Results of America's Essential Hospitals' Annual Hospital Characteristics Survey, 2012. AEH, July 2014.
Slide 22
Challenge 5. Financial uncertainty and threats to financial viability
Potential strategies to address the challenge:
- Create incentives to target enhanced Medicaid payments to safety-net hospitals that are most dependent on Medicaid revenue.
- Examples: Provide targeted Medicaid rate increases; tie rate enhancement for SNSs to performance).
- Improve targeting of Medicare and Medicaid disproportionate share payments to support safety-net hospitals with the highest proportion of uninsured patients.
- Continue Medicaid waivers to support safety-net hospital transformation.
Slide 23
Challenge 6. Fundamental questions and conflicting views on the role and status of SNSs under health care reform
Potential strategies to address the challenge:
- Convene a consensus building process.
- Example: A colloquium of policymakers and stakeholders, with discussion informed by previous research.
Slide 24
Publications and presentations
- Zallman L, Bearse A, Neal N, Lukas CV, Hacker K. Physician alignment to system redesign goals at safety net systems in the new health care era: experiences at eight institutions. Jt Comm J Qual Pat Saf. In press.
- Lukas CV, Holmes SK, Koppelman E, Gupte G, Neal N, Frigand C, Charns MP, Harrison MI. Strategic system redesign in safety-net systems: meeting the challenges of a changing healthcare environment. San Diego: Academy Health Annual Research Meeting, June 15, 2014.
- Lukas CV, Holmes SK, Koppelman E, Neal N, Charns MP, Frigand C, Gupte G. Enhancing process improvement effectiveness: system redesign in safety-net systems. Orlando: Scientific Forum, IHI 25th Annual National Forum, December 9, 2013.
2 manuscripts in preparation.
Slide 25
Selected references
Adler-Milstein J, DesRoches CM, Furukawa MF, et al. More than half of U.S. hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff 2014;33(9):1664-71.
Clark J, Singer S, Kane N, et al. From striving to thriving: systems thinking, strategy, and the performance of safety net hospitals. Health Care Manage Rev 2013;38(3):211-23.
Coughlin TA, Long SK, Sheen E, et al. How five leading safety-net hospitals are preparing for the challenges and opportunities of health care reform. Health Aff 2012;31(8):1690-7.
Cunningham PJ, Bazzoli GJ, Katz A. Caught in the competitive crossfire: safety-net providers balance margin and mission in a profit-driven health care market. Health Aff 2008;27(5):374-82.
Gilman M, Adams EK, Hockenberry JM, et al. California safety-net hospitals likely to be penalized by ACA value, readmission, and meaningful use programs. Health Aff 2014;33(8):1314-22.
Kane NM, Singer SJ, Clark JR, et al. Strained local and state government finances among current realities that threaten public hospitals' profitability. Health Aff 2012;31(8):1680-9.
Neuhausen K, Davis AC, Needleman J, et al. Disproportionate-share hospital payment reductions may threaten the financial stability of safety-net hospitals. Health Aff 2014;33(6):988-96.
Rosenbaum S, Hall MA. The health care safety net in the context of national health insurance reform. In: The health care safety net in a post-reform world. New Brunswick, NJ: Rutgers University Press; 2012. p. 153-216.
Singh S, Lin Y-L, Nattinger AB, et al. Variation in the risk of readmission among hospitals: the relative contribution of patient, hospital, and inpatient provider characteristics. J Gen Intern Med 2014;29(4):572-8.
Slide 26
Discussion…
Slide 27
Contact information
Carol VanDeusen Lukas, Ed.D.
Clinical Associate Professor
Department of Health Policy & Management
Boston University School of Public Health
Email: cvlukas@bu.edu
Michael I. Harrison, Ph.D.
Senior Social Scientist, Organizations and Systems
Center for Delivery, Organization, and Markets
Agency for Healthcare Research and Quality
Email: Michael.Harrison@ahrq.hhs.gov



