Chartbook on Care Coordination: Slide Presentation
National Healthcare Quality and Disparities Report
Slide 1
National Healthcare Quality and Disparities Report
Chartbook on Care Coordination
June 2016
Slide 2
National Healthcare Quality and Disparities Report
- Annual report to Congress mandated in the Healthcare Research and Quality Act of 1999 (P.L. 106-129).
- Provides a comprehensive overview of:
- Quality of health care received by the general U.S. population.
- Disparities in care experienced by different racial, ethnic, and socioeconomic groups.
- Assesses the performance of our health system and identifies areas of strengths and weaknesses along three main axes:
- Access to health care.
- Quality of health care.
- Priorities of the National Quality Strategy.
Slide 3
National Healthcare Quality and Disparities Report
- Based on more than 250 measures of quality and disparities covering a broad array of health care services and settings.
- Includes data from 2015 QDR, which generally cover 2001-2013.
- Produced with the help of an Interagency Work Group led by the Agency for Healthcare Research and Quality and submitted on behalf of the Secretary of Health and Human Services.
Slide 4
Key Findings of the 2015 QDR
- Access to care has improved dramatically.
- Quality of care continues to improve, but wide variation exists across the National Quality Strategy (NQS) priorities:
- Effective Treatment measures indicate improvements in overall performance and reductions in disparities.
- Care Coordination measures have lagged behind other priorities in overall performance.
- Patient Safety, Person-Centered Care, and Healthy Living measures have improved overall, but many disparities remain.
- Despite progress in some areas, disparities related to race and socioeconomic status persist among measures of access and all NQS priorities.
Notes:
- Improvements in access were led by sustained reductions in the number of Americans without health insurance and increases in the number of Americans with a usual source of medical care.
- Care Affordability measures are limited for summarizing performance and disparities.
- Disparities in access tend to be more common than disparities in quality.
Slide 5
Chartbooks Organized Around Priorities of the National Quality Strategy
- Making care safer by reducing harm caused in the delivery of care.
- Ensuring that each person and family is engaged as partners in their care.
- Promoting effective communication and coordination of care.
- Promoting the most effective prevention and treatment practices for the leading causes of mortality, starting with cardiovascular disease.
- Working with communities to promote wide use of best practices to enable healthy living.
- Making quality care more affordable for individuals, families, employers, and governments by developing and spreading new health care delivery models.
Note:
- Care Coordination is one of the six priorities identified by the National Quality Strategy (http://www.ahrq.gov/workingforquality/index.html).
Slide 6

Priority 3: Promoting effective communication and coordination of care
Long-Term Goals:
- Improve the quality of care transitions and communications across care settings.
- Improve the quality of life for patients with chronic illness and disability by following a current care plan that anticipates and addresses pain and symptom management, psychosocial needs, and functional status.
- Establish shared accountability and integration of communities and health care systems to improve quality of care and reduce health disparities.
Notes:
- The goal of care coordination is to create a delivery system that is less fragmented and more organized, where handoffs are clear and patients and clinicians have the information they need to optimize the patient-clinician partnership (NQS, 2011).
- When all of a patient's health care providers coordinate their efforts, it helps ensure that the patient receives appropriate care and support, when and how the patient needs and wants it.
- Effective care coordination models, such as patient-centered medical homes, have begun to show that they can deliver better quality care at lower costs in settings that range from small physician practices to large hospital centers.
Slide 7
Chartbook on Care Coordination
- This chartbook includes:
- Summary of trends across measures of Care Coordination from the QDR.
- Figures illustrating select measures of Care Coordination.
- Introduction and Methods contains information about methods used in the chartbook.
- A Data Query tool provides access to all data tables (https://nhqrnet.ahrq.gov/inhqrdr/data/query).
Slide 8
Trends in Care Coordination Measures
- Only 37 Care Coordination measures could be tracked over time.
- Eighteen showed improving quality.
- Six showed worsening quality.
- The remaining 13 showed no change.
- One measure improved quickly (average annual rate of change >10% per year):
- Hospital patients with heart failure who were given complete written discharge instructions.
Slide 9
Care Coordination Vision
- The vision is health care providers, patients, and caregivers all working together to "ensure that the patient gets the care and support he needs and wants, when and how he needs and wants it" (NQS, 2011).
Slide 10
Care Coordination Benefits
- Conscious, patient-centered coordination of care improves the person's experience and leads to better long-term health outcomes, as demonstrated by fewer unnecessary hospitalizations, repeated tests, and conflicting prescriptions, as well as clearer discourse between providers and patients about the best course of treatment (NQS, 2013).
Slide 11
Provider Communication and Care Coordination
- Six essential elements of provider-patient communication include:
- Having open discussion.
- Gathering information.
- Understanding the patient’s perspective.
- Sharing information.
- Reaching agreement on problems and plans.
- Providing closure (Dean, et al., 2014).
Slide 12
Measures of Care Coordination
- Transitions of care.
- Preventable emergency department visits.
- Potentially avoidable hospitalizations.
- Integration of medication information.
- Use of electronic health records.
Note:
- In addition to summarizing information on care coordination from the QDR, this chartbook tracks individual measures of care coordination, overall and for populations defined by age, race, ethnicity, income, education, insurance, and number of chronic conditions.
Slide 13
Transitions of Care
- The Centers for Medicare & Medicaid Services (CMS) defines a transition of care as the movement of a patient from one setting of care to another. Settings of care may include hospitals, ambulatory primary care practices, ambulatory specialty care practices, long-term care facilities, home health, and rehabilitation facilities.
- Transitions increase the risk of adverse events due to the potential for miscommunication as responsibility is given to new parties.
Note:
- Settings of care may include hospitals, ambulatory primary care practices, ambulatory specialty care practices, long-term care facilities, home health, and rehabilitation facilities.
Slide 14
Transitions of Care
- Hospital discharge is a complex process representing a time of significant vulnerability for patients.
- Safe and effective transfer of responsibility for a patient’s medical care relies on effective provider communication with patient comprehension of discharge instructions (Gallahue, et al., 2015).
Slide 15
Measures of Transitions of Care
- Hospitalized adult patients with heart failure who were given complete written discharge instructions.
- Communication about discharge information.
- Median hospital 30-day risk-standardized readmission rate.
Slide 16
Complete Written Discharge Instructions
- Effective care coordination begins by ensuring that accurate clinical information is available to support medical decisions by patients and providers.
- A common transition of care is hospital discharge.
- A successful transition depends on whether hospitals have adequately educated patients about key elements of care, such as diagnosis and followup plans (Horwitz, et al., 2013).
Slide 17
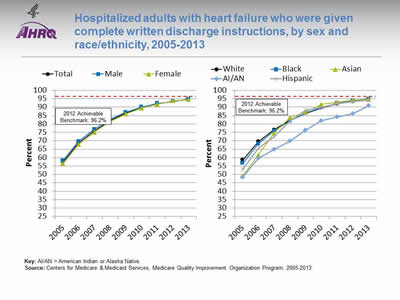
Hospitalized adults with heart failure who were given complete written discharge instructions, by sex and race/ethnicity, 2005-2013
Image: Charts show hospitalized adults with heart failure who were given complete written discharge instructions:
Left Chart:
| Sex | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|
| Total | 57.4 | 68.7 | 76.0 | 82.0 | 86.4 | 89.7 | 92.0 | 93.5 | 94.6 |
| Female | 56.4 | 67.8 | 75.1 | 81.3 | 85.9 | 89.4 | 91.7 | 93.7 | 94.5 |
| Male | 58.3 | 69.6 | 76.8 | 82.7 | 86.9 | 90.0 | 92.3 | 93.3 | 94.8 |
Right Chart:
| Race/Ethnicity | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|
| White | 58.6 | 69.5 | 76.6 | 82.2 | 86.3 | 89.6 | 91.9 | 93.4 | 94.7 |
| Black | 56.7 | 68.1 | 75.8 | 81.7 | 86.4 | 89.8 | 92.4 | 93.9 | 94.8 |
| Hispanic | 53.0 | 65.6 | 72.6 | 81.8 | 88.2 | 89.8 | 92.0 | 93.2 | 94.2 |
| AI/AN | 48.2 | 59.7 | 65.0 | 69.8 | 76.3 | 81.9 | 84.1 | 86.1 | 90.8 |
| Asian | 49.1 | 61.5 | 74.6 | 83.7 | 87.1 | 91.6 | 92.9 | 94.1 | 94.6 |
2012 Achievable Benchmark: 96.2%.
Key: AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Medicare Quality Improvement Organization Program, 2005-2013.
Notes:
- Importance: Heart failure is the most frequent hospital discharge diagnosis in the older adults. Annually more than 1 million patients are hospitalized with a primary diagnosis of heart failure accounting for a total Medicare expenditure exceeding $17 billion (Desai, 2012).
- Trends:
- From 2005 to 2013, the percentage of hospitalized adult patients with heart failure who were given complete written discharge instructions improved from 57.4% to 94.6%.
- Improvements were observed among both sexes and all racial/ethnic groups.
- Groups With Disparities:
- In all years, there were no statistically significant differences by sex.
- In all years, the percentage of hospitalized adult patients with heart failure who were given complete written discharge instructions was lower for American Indians and Alaska Natives (AI/ANs) than for Whites.
- Achievable Benchmark:
- The 2012 top 5 State achievable benchmark was 96.2%. The top 5 States that contributed to the achievable benchmark are Illinois, Maine, New Hampshire, New Jersey, and Ohio.
- At the current rates of increase, this benchmark could be attained overall and by both sexes in less than a year. All racial/ethnic groups could attain the benchmark in less than a year except AI/ANs, who could achieve the benchmark in about 1 year.
Slide 18
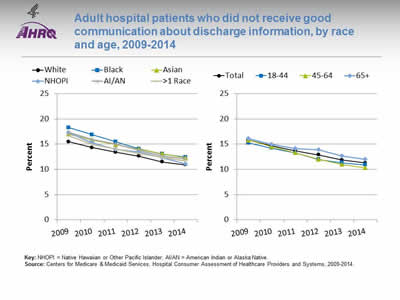
Adult hospital patients who did not receive good communication about discharge information, by race and age, 2009-2014
Image: Charts show adult hospital patients who did not receive good communication about discharge information:
Left Chart:
| Year | White | Black | Asian | NHOPI | AI/AN | >1 Race |
|---|---|---|---|---|---|---|
| 2009 | 15.5 | 18.2 | 17.0 | 17.2 | 17.4 | 16.7 |
| 2010 | 14.3 | 16.9 | 15.8 | 15.3 | 16.0 | 15.0 |
| 2011 | 13.4 | 15.5 | 14.9 | 14.0 | 15.0 | 14.1 |
| 2012 | 12.6 | 14.1 | 14.0 | 13.5 | 13.8 | 13.1 |
| 2013 | 11.5 | 13.0 | 13.1 | 12.3 | 12.7 | 12.4 |
| 2014 | 10.9 | 12.4 | 12.3 | 11.1 | 12.1 | 11.7 |
Right Chart:
| Year | Total | 18-44 | 45-64 | 65+ |
|---|---|---|---|---|
| 2009 | 15.8 | 15.2 | 15.8 | 16.1 |
| 2010 | 14.6 | 14.2 | 14.5 | 14.9 |
| 2011 | 13.7 | 13.2 | 13.3 | 14.1 |
| 2012 | 12.9 | 11.9 | 12.0 | 13.8 |
| 2013 | 11.8 | 11.3 | 11.0 | 12.6 |
| 2014 | 11.3 | 10.9 | 10.3 | 12.0 |
Key: NHOPI = Native Hawaiian or Other Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Hospital Consumer Assessment of Healthcare Providers and Systems,.2009-2014.
Notes:
- Importance: Health care provider–patient communication about prognosis and preferences for care is critical in helping patients adequately prepare for and plan future care, and physicians’ communication style may affect patients’ satisfaction, trust, willingness to cooperate, and health status.
- Trends:
- From 2009 to 2014, the percentage of adult hospital patients who did not receive good communication about discharge information improved from 15.8% to 11.3%.
- From 2009 to 2014, improvements were observed among all racial and age groups.
- Groups With Disparities:
- In all years, Black and Asian patients were less likely than White patients to receive good communication about discharge information.
- In all years except 2012, AI/AN patients were less likely than White patients to receive good communication about discharge information.
Slide 19
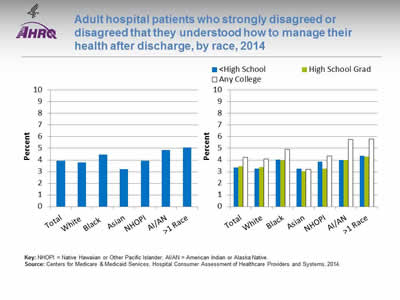
Adult hospital patients who strongly disagreed or disagreed that they understood how to manage their health after discharge, by race, 2014
Image: Charts show adult hospital patients who strongly disagreed or disagreed that they understood how to manage their health after discharge:
Left Chart:
- Total - 3.9.
- White - 3.8.
- Black - -4.5.
- Asian - 3.2.
- NHOPI - 3.9.
- AI/AN - 4.9.
- More than 1 Race - 5.1.
Right Chart:
| Race | <High School | High School Grad | Any College |
|---|---|---|---|
| Total | 3.4 | 3.5 | 4.3 |
| White | 3.2 | 3.4 | 4.1 |
| Black | 4.0 | 4.0 | 4.9 |
| Asian | 3.3 | 3.0 | 3.2 |
| NHOPI | 3.8 | 3.3 | 4.4 |
| AI/AN | 4.0 | 4.0 | 5.8 |
| >1 Race | 4.3 | 4.3 | 5.8 |
Key: NHOPI = Native Hawaiian or Other Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Hospital Consumer Assessment of Healthcare Providers and Systems, 2014.
Notes:
- Importance: Comprehension of and compliance with discharge instructions can reduce emergency department visits and rehospitalizations, improve postdischarge health outcomes, and decrease health care expenditures.
- Overall Rate: In 2014, 3.9% of hospital patients strongly disagreed or disagreed that they understood how to manage their health after discharge.
- Groups With Disparities:
- In 2014, Black, AI/AN, and multiple-race patients were more likely than White patients to strongly disagree or disagree that they understood how to manage their health after discharge.
- In 2014, White, Black, AI/AN, and multiple-race patients with any college education were more likely than patients with no college education to strongly disagree or disagree that they understood how to manage their health after discharge.
Slide 20
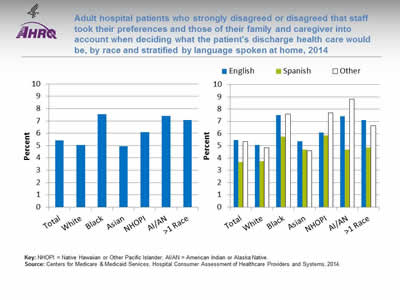
Adult hospital patients who strongly disagreed or disagreed that staff took their preferences and those of their family and caregiver into account when deciding what the patient's discharge health care would be, by race and stratified by language spoken at home, 2014
Image: Charts show adult hospital patients who strongly disagreed or disagreed that staff took their preferences and those of their family and caregiver into account when deciding what the patient's discharge health care would be:
Left Chart:
- Total - 5.4.
- White - 5.0.
- Black - 7.5.
- Asian - 4.9.
- NHOPI - 6.1.
- AI/AN - 7.4.
- More than 1 Race - 7.1
Right Chart:
| Race | English | Spanish | Other |
|---|---|---|---|
| Total | 5.5 | 3.7 | 5.3 |
| White | 5.1 | 3.8 | 4.9 |
| Black | 7.5 | 5.8 | 7.6 |
| Asian | 5.4 | 4.7 | 4.6 |
| NHOPI | 6.1 | 5.9 | 7.7 |
| AI/AN | 7.4 | 4.7 | 8.8 |
| >1 Race | 7.1 | 4.9 | 6.7 |
Key: NHOPI = Native Hawaiian or Other Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Hospital Consumer Assessment of Healthcare Providers and Systems, 2014.
Notes:
- Importance: Providing comprehensive, patient-centered discharge planning can help reduce readmission rates.
- Overall Rate: In 2014, 5.4% of hospital patients strongly disagreed or disagreed that staff took their preferences and those of their families and caregiver into account when deciding what the patient’s discharge health care would be.
- Groups With Disparities:
- In 2014, Black, NHOPI, AI/AN, and multiple-race patients were more likely than White patients to strongly disagree or disagree that staff took their preferences and those of their families and caregiver into account when deciding what the patient’s discharge health care would be.
- In 2014, White, Black, AI/AN, and multiple-race patients whose preferred language was Spanish were less likely than patients whose preferred language was English to strongly disagree or disagree that staff took their preferences and those of their families and caregiver into account when deciding what the patient’s discharge health care would be.
Slide 21
Readmissions
- Hospital readmission shortly after discharge is a marker of inpatient quality of care and a significant contributor to rising health care costs (Hasan, 2010).
- In 2013, approximately two-thirds of U.S. hospitals faced financial penalties from CMS because of excessively high 30-day readmission rates for acute myocardial infarction, heart failure, and pneumonia (Rau, 2013).
Slide 22
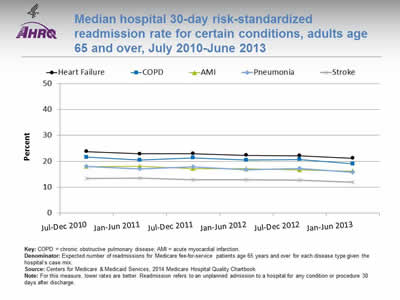
Median hospital 30-day risk-standardized readmission rate for certain conditions, adults age 65 and over, July 2010-June 2013
Image: Chart shows median hospital 30-day risk-standardized readmission rate for certain conditions:
| Date | Heart Failure | COPD | AMI | Pneumonia | Stroke |
|---|---|---|---|---|---|
| Jul-Dec 2010 | 23.8 | 21.6 | 18.0 | 18.0 | 13.4 |
| Jan-Jun 2011 | 22.9 | 20.5 | 18.1 | 17.1 | 13.5 |
| Jul-Dec 2011 | 23.0 | 21.4 | 17.2 | 17.9 | 12.9 |
| Jan-Jun 2012 | 22.3 | 20.5 | 17.1 | 16.7 | 12.9 |
| Jul-Dec 2012 | 22.2 | 20.7 | 16.7 | 17.3 | 12.8 |
| Jan-Jun 2013 | 21.2 | 19.0 | 16.2 | 15.8 | 12.0 |
Key: COPD = chronic obstructive pulmonary disease; AMI = acute myocardial infarction.
Denominator: Expected number of readmissions for Medicare fee-for-service patients age 65 years and over for each disease type given the hospital's case mix.
Source: Centers for Medicare & Medicaid Services, 2014 Medicare Hospital Quality Chartbook.
Notes: For this measure, lower rates are better. Readmission refers to an unplanned admission to a hospital for any condition or procedure 30 days after discharge.
- Importance: Although not all hospital readmissions are preventable, readmission rates may show whether a hospital is doing its best to deliver quality care, prevent complications, teach patients at discharge, and ensure that patients make a smooth transition to their home or another setting, such as a nursing home.
- Overall Rate: The median 30-day risk-standardized readmission rate in 2013 was 21.2% among patients with heart failure, 19.0% among patients with chronic obstructive pulmonary disease (COPD), 16.2% among patients with acute myocardial infarction (AMI), 15.8% among patients with pneumonia, and 12.0% among patients who had a stroke.
- Trends: From July-December 2010 to January-June 2013, the median 30-day risk-standardized readmission rate decreased 12% among patients with pneumonia and COPD, 11% among patients with heart failure, 10.5% among patients with stroke, and 10% among patients with AMI.
Slide 23
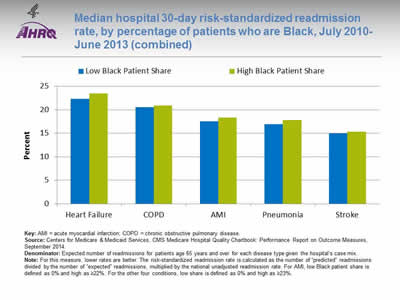
Median hospital 30-day risk-standardized readmission rate, by percentage of patients who are Black, July 2010-June 2013 (combined)
Image: Chart shows median hospital 30-day risk-standardized readmission rate, by percentage of patients who are Black:
| Heart Failure | COPD | AMI | Pneumonia | Stroke | |
|---|---|---|---|---|---|
| Low Black Patient Share | 22.3 | 20.5 | 17.5 | 16.9 | 15 |
| High Black Patient Share | 23.5 | 20.9 | 18.3 | 17.8 | 15.3 |
Key: AMI = acute myocardial infarction; COPD = chronic obstructive pulmonary disease.
Source: Centers for Medicare & Medicaid Services, CMS Medicare Hospital Quality Chartbook: Performance Report on Outcome Measures, September 2014.
Denominator: Expected number of readmissions for patients age 65 years and over for each disease type given the hospital's case mix.
Notes: For this measure, lower rates are better. The risk-standardized readmission rate is calculated as the number of "predicted" readmissions divided by the number of "expected" readmissions, multiplied by the national unadjusted readmission rate. For AMI, low Black patient share is defined as 0% and high as <22%. For the other four conditions, low share is defined as 0% and high as <23%.
- Importance: Although not all hospital readmissions are preventable, readmission rates may show whether a hospital is doing its best to deliver quality care, prevent complications, teach patients at discharge, and ensure that patients make a smooth transition to their home or another setting, such as a nursing home.
- Groups With Disparities:
- The 2010 to 2013 median 30-day risk-standardized readmission rate for hospitals with high shares of Black patients was highest for heart failure (23.5%) and chronic obstructive pulmonary disease (20.9%), lower for acute myocardial infarction (18.3%) and pneumonia (17.8%), and lowest for stroke (15.3%). These rates were similar to those for hospitals with low shares of Black patients.
Slide 24
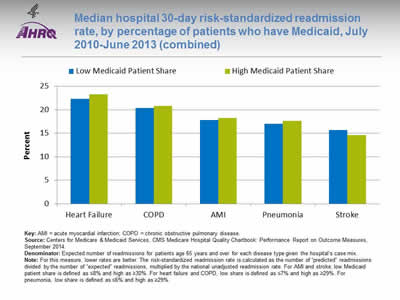
Median hospital 30-day risk-standardized readmission rate, by percentage of patients who have Medicaid, July 2010-June 2013 (combined)
Image: Chart shows median hospital 30-day risk-standardized readmission rate, by percentage of patients who have Medicaid:
| Heart Failure | COPD | AMI | Pneumonia | Stroke | |
|---|---|---|---|---|---|
| Low Medicaid Patient Share | 22.3 | 20.4 | 17.8 | 17 | 15.7 |
| High Medicaid Patient Share | 23.3 | 20.8 | 18.2 | 17.6 | 14.6 |
Key: AMI = acute myocardial infarction; COPD = chronic obstructive pulmonary disease.
Source: Centers for Medicare & Medicaid Services, CMS Medicare Hospital Quality Chartbook: Performance Report on Outcome Measures, September 2014.
Denominator: Expected number of readmissions for patients age 65 years and over for each disease type given the hospital's case mix.
Notes: For this measure, lower rates are better. The risk-standardized readmission rate is calculated as the number of "predicted" readmissions divided by the number of "expected" readmissions, multiplied by the national unadjusted readmission rate. For AMI and stroke, low Medicaid patient share is defined as ≤8% and high as ≥30%. For heart failure and COPD, low share is defined as ≤7% and high as ≥29%. For pneumonia, low share is defined as ≤6% and high as ≥29%.
- Importance: Although not all hospital readmissions are preventable, readmission rates may show whether a hospital is doing its best to deliver quality care, prevent complications, teach patients at discharge, and ensure that patients make a smooth transition to their home or another setting, such as a nursing home.
- Groups With Disparities:
- The 2010 to 2013 median 30-day risk-standardized readmission rate for hospitals with high Medicaid patient share was highest for heart failure (23.3%) and chronic obstructive pulmonary disease (20.8%), lower for acute myocardial infarction (18.2%) and pneumonia (17.6%), and lowest for stroke (14.6%). These rates were similar to those for hospitals with low Medicaid patient share.
Slide 25
Preventable Emergency Department Visits
- Emergency department (ED) visits are costly.
- Because some visits are preventable, they may indicate:
- Poor care management.
- Inadequate access to care.
- Poor choices on the part of patients (Dowd, et al., 2014).
Slide 26
Importance of Preventing Emergency Department Visits
- ED visits for conditions that are preventable or treatable with appropriate primary care lower health system efficiency and raise costs (Enard & Ganelin, 2013).
- An estimated 13% to 27% of ED visits in the United States could be managed in physician offices, clinics, and urgent care centers, saving $4.4 billion annually (Weinick, et al., 2010).
Slide 27
Measures of Preventable Emergency Department Visits
- ED visits with a principal diagnosis related to mental health, alcohol, or substance abuse.
- ED visits with a principal diagnosis of dental conditions.
- ED visits for asthma, ages 18-39.
- ED visits for asthma, ages 2-17.
Slide 28
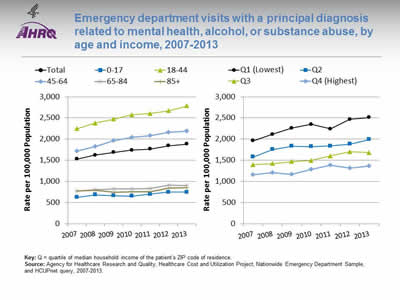
Emergency department visits with a principal diagnosis related to mental health, alcohol, or substance abuse, by age and income, 2007-2013
Image: Charts show emergency department visits with a principal diagnosis related to mental health, alcohol, or substance abuse:
Left Chart:
| Age | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|
| Total | 1527.8 | 1624.1 | 1687.4 | 1738.7 | 1766.8 | 1841.1 | 1883 |
| 0-17 | 621.8 | 684 | 663.3 | 655.3 | 697.5 | 745.6 | 748.6 |
| 18-44 | 2244.1 | 2379.5 | 2471.1 | 2576 | 2607.4 | 2670.7 | 2788.9 |
| 45-64 | 1720.1 | 1824.4 | 1966.4 | 2037.4 | 2077.5 | 2165 | 2189.8 |
| 65-84 | 773.7 | 807.6 | 826.5 | 824.4 | 828.8 | 914.8 | 904.4 |
| 85+ | 769.5 | 790.8 | 748.6 | 757.5 | 757.9 | 843.2 | 851.6 |
Right Chart:
| Income | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|
| Q1 (Lowest) | 1961.1 | 2114.5 | 2263.2 | 2347.8 | 2242.6 | 2466.6 | 2510 |
| Q2 | 1576.4 | 1756.3 | 1834.2 | 1821.4 | 1838 | 1880.8 | 1989.2 |
| Q3 | 1396.7 | 1422.3 | 1471.4 | 1492.6 | 1600.9 | 1702.1 | 1681.1 |
| Q4 (Highest) | 1153.7 | 1203.8 | 1168.4 | 1288.3 | 1386.5 | 1314.6 | 1362.3 |
Key: Q = quartile of median household income of the patient's ZIP code of residence.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department Sample, and HCUPnet query, 2007-2013.
Notes:
- Importance: Frequent ED users with mental health and addiction challenges are in dire need of effective treatment and case management. Further, pediatric emergency physicians may struggle to provide effective care and consider the ED ill suited to ensure continuity of care when treating alcohol-related issues among adolescents.
- Trends:
- From 2007 to 2013, the overall rate of ED visits with a principal diagnosis related to mental health, alcohol, or substance abuse increased from 1,527.8 to 1,883.0 per 100,000 population.
- From 2007 to 2013, the rate of ED visits with a principal diagnosis related to mental health, alcohol, or substance abuse increased among all age and income groups.
- Groups With Disparities:
- In all years, individuals in the highest income quartile were less likely than individuals in all other income groups to have an ED visit with a principal diagnosis related to mental health, alcohol, or substance abuse.
- In all years, individuals ages 0-17 and 65 and over were significantly less likely than individuals ages 18-44 to have an ED visit with a principal diagnosis related to mental health, alcohol, or substance abuse.
Slide 29
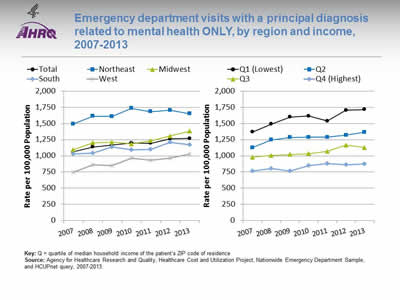
Emergency department visits with a principal diagnosis related to mental health only, by region and income, 2007-2013
Image: Charts show emergency department visits with a principal diagnosis related to mental health only:
Left Chart:
| Region | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|
| Total | 1063.5 | 1135.6 | 1169.5 | 1196.7 | 1193.1 | 1260.8 | 1268.7 |
| Northeast | 1493.5 | 1609.9 | 1607.8 | 1734.8 | 1681.5 | 1704.9 | 1650.3 |
| Midwest | 1095.7 | 1200.7 | 1210.5 | 1186.1 | 1232.7 | 1307.1 | 1380.5 |
| South | 1031.1 | 1039.3 | 1135.2 | 1091.1 | 1098.3 | 1209 | 1173.2 |
| West | 746.6 | 860.2 | 851.7 | 964.4 | 934.4 | 963.7 | 1031.1 |
Right Chart:
| Income | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|
| Q1 (Lowest) | 1368.9 | 1488.6 | 1597.5 | 1613.2 | 1536.9 | 1703 | 1715 |
| Q2 | 1127.9 | 1244.2 | 1284.5 | 1287.4 | 1285.7 | 1318.4 | 1365.9 |
| Q3 | 978.3 | 1003.7 | 1022.5 | 1035.2 | 1068.8 | 1164.5 | 1128.3 |
| Q4 (Highest) | 763.3 | 806.4 | 763.5 | 849 | 883.9 | 859.1 | 872.5 |
Key: Q = quartile of median household income of the patient's ZIP code of residence
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department Sample, and HCUPnet query, 2007-2013.
Notes:
- Importance: Adults with mental health disorders are less likely to care for their chronic medical conditions and have worse outcomes of co-occurring chronic diseases compared with patients without mental health disorders. They are also more likely to have frequent ED visits.
- Trends:
- From 2007 to 2013, the overall rate of ED visits with a principal diagnosis related to mental health increased from 1,063.5 to 1,268.7 per 100,000 population.
- Groups With Disparities:
- In all years, individuals in the highest income quartile were less likely than individuals in all other income groups to have an ED visit with a principal diagnosis related to mental health.
- In 2013, the rate of ED visits with a principal diagnosis related to mental health was lowest for individuals in the West (1,031.1 per 100,000 population) and highest in the Northeast (1,650.3 per 100,000 population).
- In 6 of 7 years, residents of micropolitan areas were more likely than residents of large fringe metropolitan areas (suburbs) to have an ED visit with a principal diagnosis related to mental health (data not shown).
Slide 30
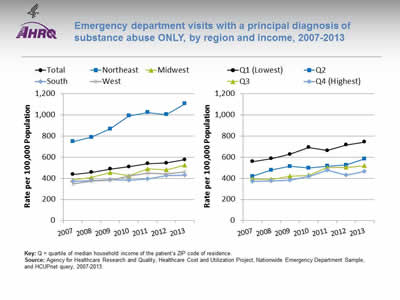
Emergency department visits with a principal diagnosis of substance abuse only, by region and income, 2007-2013
Image: Charts show emergency department visits with a principal diagnosis of substance abuse only:
Left Chart:
| Region | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|
| Total | 437.7 | 457.7 | 487.5 | 510.2 | 540 | 545 | 577.7 |
| Northeast | 748.4 | 788.9 | 867.4 | 990.9 | 1022.7 | 1004.4 | 1105.5 |
| Midwest | 383.7 | 407.2 | 454.8 | 424.3 | 490.4 | 480.1 | 525.8 |
| South | 371 | 377.9 | 388.7 | 385 | 393.8 | 427.6 | 430.5 |
| West | 349.5 | 374.7 | 383.7 | 421.4 | 449.8 | 443.1 | 461.7 |
Right Chart:
| Income | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|
| Q1 (Lowest) | 558.4 | 586.3 | 627.4 | 692.4 | 662.8 | 715.5 | 744.7 |
| Q2 | 419.3 | 477.9 | 514.8 | 499 | 515.2 | 526.6 | 584.1 |
| Q3 | 393.2 | 390.4 | 421 | 430 | 501.5 | 504.3 | 520.6 |
| Q4 (Highest) | 372.4 | 376.5 | 384.3 | 416.7 | 478.3 | 431.6 | 465 |
Key: Q = quartile of median household income of the patient's ZIP code of residence.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department Sample, and HCUPnet query, 2007-2013.
Notes:
- Importance:
- In 2011, the Drug Abuse Warning Network estimated that about 2.5 million ED visits resulted from medical emergencies involving drug misuse or abuse. Of all drug misuse or abuse ED visits, about 1.25 million ED visits, or 50%, involved illicit drugs, about 1.24 million, or 50%, involved nonmedical use of pharmaceuticals, and about 0.61 million, or 25%, involved drugs combined with alcohol.
- According to the Centers for Disease Control and Prevention, the United States is experiencing an epidemic of drug overdose deaths. Since 2000, the rate of deaths from drug overdoses has increased 137%, including a 200% increase in the rate of overdose deaths involving opioids. The rate of drug overdose deaths increased significantly for both sexes, people ages 25-44 and 55 and over, non-Hispanic Whites, non-Hispanic Blacks, and residents of the Northeastern, Midwestern, and Southern regions (Rudd, et al., 2016).
- Trends:
- From 2007 to 2013, the overall rate of ED visits with a principal diagnosis related to substance abuse increased from 437.7 to 577.7 per 100,000 population.
- Groups With Disparities:
- In 2013, the rate of ED visits with a principal diagnosis of substance abuse was lowest for individuals in the South (430.5 per 100,000 population) and highest in the Northeast (1,105.5 per 100,000 population).
- In all years, individuals in the highest income quartile were less likely than individuals in all other income groups to have an ED visit with a principal diagnosis related to substance abuse.
Slide 31
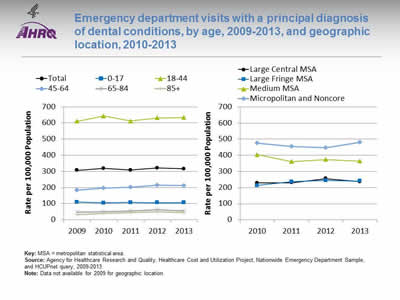
Emergency department visits with a principal diagnosis of dental conditions, by age, 2009-2013, and geographic location, 2010-2013
Image: Charts show emergency department visits with a principal diagnosis of dental conditions:
Left Chart:
| Age | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Total | 307 | 318.3 | 308.2 | 321 | 316.1 |
| 0-17 | 110 | 104.8 | 106.9 | 106.1 | 106.3 |
| 18-44 | 611 | 643.2 | 611.8 | 630.8 | 633.7 |
| 45-64 | 184 | 196.7 | 202.8 | 214.7 | 211 |
| 65-84 | 46 | 49.9 | 54.2 | 61.5 | 55 |
| 85+ | 33 | 39.7 | 44.8 | 49.5 | 45 |
Right Chart:
| Location | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|
| Large Central MSA | 228.8 | 229.7 | 255.9 | 236.2 |
| Large Fringe MSA | 212.7 | 236.1 | 244 | 239.8 |
| Medium MSA | 403.5 | 360.7 | 374.1 | 363.7 |
| Micropolitan and Noncore | 476.3 | 455.8 | 446.8 | 480 |
Key: MSA = metropolitan statistical area.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department Sample, and HCUPnet query, 2009-2013.
Notes: Data not available for 2009 for geographic location.
- Importance: Dental conditions such as dental caries, pulpal lesions, and gingival or periodontal conditions are treated routinely in dental office settings. When neglected, these minor localized infections can progress to form cellulitis or systemic infection and can even result in death. Evidence shows that care provided in hospital settings is less effective in managing oral health complaints and therefore may represent a highly inefficient use of limited hospital resources.
- Trends:
- From 2009 to 2013, the overall rate of emergency department visits with a principal diagnosis related to dental conditions increased from 307.0 to 316.1 per 100,000 population.
- Groups With Disparities:
- In 2013, the rate of ED visits with a principal diagnosis of dental conditions was lowest for individuals age 85 and over (45.0 per 100,000 population) and highest for individuals ages 18-44 (633.7 per 100,000 population).
- In all years, residents of micropolitan and noncore areas were more likely than residents of large fringe metropolitan areas to have an ED visit with a principal diagnosis of dental conditions.
Slide 32
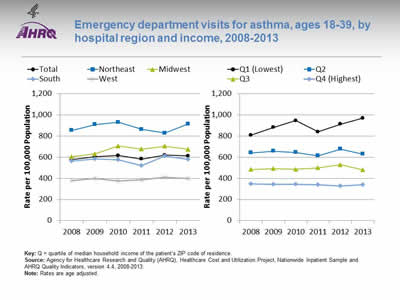
Emergency department visits for asthma, ages 18-39, by hospital region and income, 2008-2013
Image: Charts show emergency department visits for asthma, ages 18-39:
Left Chart:
| Region | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|
| Total | 578.0 | 604.2 | 616.3 | 582.0 | 619.2 | 613.1 |
| Northeast | 854.4 | 909.3 | 931.0 | 864.6 | 829.3 | 914.8 |
| Midwest | 604.6 | 631.6 | 706.2 | 677.9 | 705.5 | 674.4 |
| South | 564.4 | 583.5 | 576.5 | 522.6 | 611.4 | 577.9 |
| West | 378.6 | 397.0 | 376.4 | 388.4 | 408.8 | 400.7 |
Right Chart:
| Income | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|
| Q1 (Lowest) | 808.6 | 881.3 | 947.4 | 839.5 | 913.0 | 969.6 |
| Q2 | 641.8 | 656.7 | 644.9 | 613.8 | 677.7 | 630.4 |
| Q3 | 483.7 | 491.4 | 485.8 | 499.6 | 530.2 | 480.6 |
| Q4 (Highest) | 348.3 | 343.3 | 342.4 | 341.2 | 327.6 | 338.8 |
Key: Q = quartile of median household income of the patient's ZIP code of residence.
Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project, Nationwide Inpatient Sample and AHRQ Quality Indicators, version 4.4, 2008-2013.
Notes: Rates are age adjusted.
- Importance: Asthma exacerbations were responsible for approximately 2 million ED visits in 2012. ED visits for asthma exacerbation suggest a failure of prevention-oriented care since most asthma exacerbations are preventable with high-quality long-term management.
- Trends:
- From 2008 to 2013, the overall rate of ED visits for asthma increased from 578.0 to 613.1 per 100,000 population.
- Groups With Disparities:
- From 2008 to 2013, rates of ED visits for asthma were highest in the Northeast and lowest in the West. In 2013, the rate of ED visits for asthma in the Northeast was 914.8 per 100,000 population, followed by the Midwest (674.4 per 100,000 population), the South (577.9 per 100,000 population), and the West (400.7 per 100,000 population).
- In all years, adults with the highest income were significantly less likely than all other income groups to have an ED visit for asthma.
Slide 33

Emergency department visits for asthma, ages 2-17, by hospital region and income, 2008-2013
Image: Charts show emergency department visits for asthma, ages 2-17:
Left Chart:
| Region | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|
| Total | 851.9 | 963.7 | 902.5 | 932.1 | 994.0 | 930.3 |
| Northeast | 1197.2 | 1330.8 | 1243.7 | 1199.5 | 1235.3 | 1297.6 |
| Midwest | 787.2 | 853.3 | 753.4 | 879.1 | 1023.6 | 868.8 |
| South | 856.2 | 1013.8 | 1006.8 | 1058.7 | 1019.8 | 922.8 |
| West | 667.7 | 738.6 | 646 | 603.6 | 768.8 | 752.5 |
Right Chart:
| Income | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|
| Q1 (Lowest) | 1195.6 | 1411.8 | 1339.9 | 1254.5 | 1500.3 | 1568.7 |
| Q2 | 916.2 | 1040.1 | 993.8 | 990.6 | 1034.9 | 889.8 |
| Q3 | 731.1 | 773.8 | 732.9 | 851 | 837.6 | 743.8 |
| Q4 (Highest) | 553.1 | 604.7 | 524.6 | 621.2 | 587.5 | 516.4 |
Key: Q = quartile of median household income of the patient's ZIP code of residence.
Source: Agency for Healthcare Research and Quality (AHRQ), Center for Delivery, Organization, and Markets, Healthcare Cost and Utilization Project, Nationwide Inpatient Sample and AHRQ Quality Indicators, version 4.4, 2008-2013.
Notes:
- Importance: Asthma exacerbations were responsible for approximately 2 million ED visits in 2012. ED visits for asthma exacerbation suggest a failure of prevention-oriented care since most asthma exacerbations are preventable with high-quality long-term management.
- Trends:
- From 2008 to 2013, the overall rate of emergency department visits for asthma increased from 851.9 to 930.3 per 100,000 population.
- Groups With Disparities:
- From 2008 to 2013, rates of ED visits for asthma were highest in the Northeast and lowest in the West. In 2013, the rate of ED visits for asthma in the Northeast was 1,297.6 per 100,000 population, followed by the South (922.8 per 100,000 population), the Midwest (868.8 per 100,000 population), and the West (752.5 per 100,000 population).
- In all years, children in households in the highest income quartile were significantly less likely than all other income groups to have an ED visit for asthma.
Slide 34
Potentially Avoidable Hospitalizations
- Hospitalizations due to ambulatory care-sensitive conditions (ACSCs) such as hypertension and pneumonia should be largely prevented if ambulatory care is provided in a timely and effective manner.
- Evidence suggests that effective primary care is associated with lower ACSC hospitalization (also referred to as avoidable hospitalization) (Gao, et al., 2014).
Slide 35
Potentially Avoidable Hospitalization Measures
- Potentially avoidable hospitalizations for acute and chronic conditions.
- Admissions with perforated appendix.
- Admissions with hypertension.
Slide 36
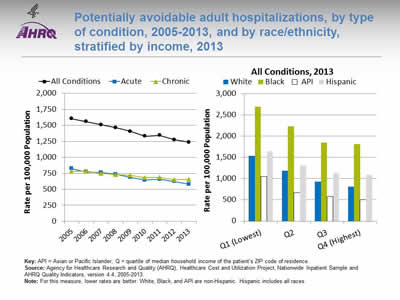
Potentially avoidable adult hospitalizations, by type of condition, 2005-2013, and by race/ethnicity, stratified by income, 2013
Image: Charts show potentially avoidable adult hospitalizations, by type of condition:
Left Chart:
| Conditions | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|
| All Conditions | 1604.7 | 1556.8 | 1510.4 | 1464.3 | 1404.2 | 1329.4 | 1345.4 | 1274.1 | 1236.3 |
| Acute | 822.9 | 771.0 | 760.9 | 736.4 | 685.8 | 645.4 | 657.0 | 621.5 | 580.4 |
| Chronic | 781.8 | 785.9 | 749.5 | 728.0 | 718.4 | 684.0 | 688.4 | 652.6 | 655.9 |
Right Chart (All Conditions):
| Income | White | Black | API | Hispanic |
|---|---|---|---|---|
| Q1 (Lowest) | 1536.3 | 2695.9 | 1056.4 | 1641.5 |
| Q2 | 1187 | 2230.4 | 666.3 | 1309 |
| Q3 | 930.3 | 1855 | 580.2 | 1131.4 |
| Q4 (Highest) | 815.2 | 1810.9 | 504.2 | 1085 |
Key: API = Asian or Pacific Islander; Q = quartile of median household income of the patient's ZIP code of residence.
Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project, Nationwide Inpatient Sample and AHRQ Quality Indicators, version 4.4, 2005-2013.
Notes: For this measure, lower rates are better. White, Black, and API are non-Hispanic. Hispanic includes all races.
- Importance: Early intervention to prevent complications and address exacerbations of ambulatory care-sensitive conditions, such as diabetes, chronic obstructive pulmonary disease (COPD), asthma, and congestive heart failure, through good primary care may prevent the need for hospitalization.
- Trends:
- From 2005 to 2013, the rate of potentially avoidable hospitalizations for all conditions, excluding COPD, fell from 1,604.7 to 1,236.3 per 100,000 population.
- The rate for acute conditions decreased from 822.9 to 580.4 per 100,000 population, and the rate for chronic conditions, excluding COPD, fell from 781.8 to 655.9 per 100,000 population.
- Groups With Disparities:
- In 2013, in all income groups, rates of potentially avoidable hospitalizations for all conditions were higher for Blacks than Whites and lower for Asians and Pacific Islanders (APIs) than Whites.
- In 2013, rates if potentially avoidable hospitalizations for all conditions was 1536.3 per 100,000 population for Whites in the lowest income groups and 1810.9 per 100,000 population for Blacks in the highest income group.
Slide 37
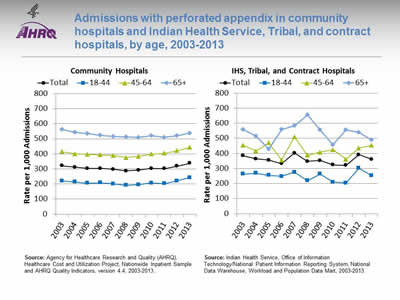
Admissions with perforated appendix in community hospitals and Indian Health Service (IHS), Tribal, and contract hospitals, by age, 2003-2013
Image: Charts show admissions with perforated appendix in community hospitals and Indian Health Service, Tribal, and contract hospitals:
Left Chart (Community Hospitals):
| Age | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 321.6 | 311.5 | 303.9 | 303.4 | 297.2 | 287.3 | 292.1 | 303.8 | 301.3 | 318.1 | 338.4 |
| 18-44 | 219.8 | 214.1 | 205.5 | 208.7 | 201.8 | 191.5 | 196.1 | 206.9 | 202.4 | 220.0 | 242.4 |
| 45-64 | 414.8 | 400.3 | 397.0 | 392.4 | 389.1 | 375.4 | 384.0 | 398.7 | 404.5 | 421.0 | 443.2 |
| 65+ | 563.4 | 542.0 | 533.9 | 522.8 | 516.4 | 512.9 | 508.8 | 519.5 | 511.0 | 521.2 | 536.1 |
Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project, Nationwide Inpatient Sample and AHRQ Quality Indicators, version 4.4, 2003-2013.
Right Chart (IHS, Tribal, and Contract Hospitals):
| Age | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 384.4 | 363.3 | 355.8 | 332.6 | 402.7 | 347.7 | 353.4 | 324.1 | 321 | 392.1 | 360.8 |
| 18-44 | 263.6 | 268.7 | 254.8 | 247.8 | 275.4 | 219.8 | 263.5 | 208.9 | 204 | 302.2 | 253.4 |
| 45-64 | 453.2 | 415.9 | 469.8 | 356.2 | 509.7 | 387.9 | 407.9 | 424.6 | 361 | 436.1 | 454 |
| 65+ | 560 | 514.3 | 428.6 | 560 | 583.3 | 656.3 | 555.6 | 457.1 | 555.6 | 538.5 | 489.4 |
Source: Indian Health Service, Office of Information Technology/National Patient Information Reporting System, National Data Warehouse, Workload and Population Data Mart, 2003-2013.
Notes:
- Importance: Appendicitis is the most common indication for an urgent intra-abdominal surgery. The misdiagnosis of appendicitis is costly in terms of patients’ pain and suffering, as well as in the cost to the hospital of extended treatments and care.
- Trends:
- From 2003 to 2013, the rate of perforated appendixes in community hospitals increased from 321.6 to 338.4 per 1,000 admissions.
- From 2003 to 2013, the rate of perforated appendixes in IHS hospitals decreased from 384.4 to 360.8 per 1,000 admissions.
- Groups With Disparities:
- In 2013, for IHS facilities, the rates of perforated appendixes for ages 45-64 and age 65 and over were higher than for those ages 18-44 (454.0 and 489.4 per 1,000 admissions, respectively, compared with 253.4 per 1,000 admissions).
- In all years, rates of perforated appendixes for males were higher than for females at non-IHS hospitals; rates were higher for males than for females in 9 of 11 years at IHS hospitals (data not shown).
Slide 38
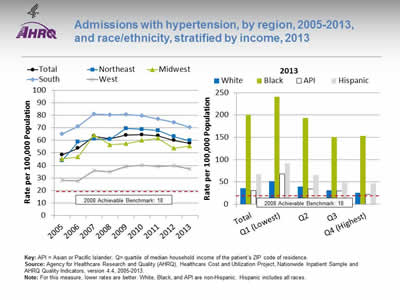
Admissions with hypertension, by region, 2005-2013, and race/ethnicity, stratified by income, 2013
Image: Charts show admissions with hypertension:
Left Chart:
| Region | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|
| Total | 48.4 | 53.7 | 63.4 | 61.2 | 64.1 | 64.4 | 63.6 | 60.1 | 57.8 |
| Northeast | 43.7 | 58.6 | 61.1 | 60.9 | 69.5 | 68.9 | 67.8 | 63.1 | 59.6 |
| Midwest | 45.3 | 46.8 | 64.1 | 56.5 | 57.3 | 60.0 | 61.7 | 53.7 | 55.6 |
| South | 65.1 | 71.0 | 80.9 | 80.3 | 80.6 | 79.6 | 77.2 | 74.3 | 70.5 |
| West | 28.1 | 27.7 | 35.9 | 35.0 | 39.3 | 40.0 | 39.3 | 39.9 | 37.3 |
Right Chart (2013):
| Income | White | Black | API | Hispanic |
|---|---|---|---|---|
| Total | 35.8 | 200.5 | 30.9 | 67.8 |
| Q1 (Lowest) | 51.9 | 241.3 | 68.3 | 91.6 |
| Q2 | 39.4 | 193.7 | 34.1 | 65.5 |
| Q3 | 31.1 | 150.1 | 30.1 | 52.4 |
| Q4 (Highest) | 25.9 | 153 | 21.8 | 47 |
2008 Achievable Benchmark: 18.
Key: API = Asian or Pacific Islander; Q = quartile of median household income of the patient's ZIP code of residence.
Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project, Nationwide Inpatient Sample and AHRQ Quality Indicators, version 4.4, 2005-2013.
Notes: For this measure, lower rates are better. White, Black, and API are non-Hispanic. Hispanic includes all races.
- Importance: Hypertensive emergency is a condition that affects approximately 1% of all patients with chronic hypertension (Kuppasani & Reddi, 2010). Among hypertensive individuals, in 2011-2012, only 51.9% had their blood pressure controlled to below 140/90 mmHg (Nwankwo, et al., 2013). Hypertension is an important risk factor for cardiovascular diseases, and uncontrolled hypertension is present in 69% of patients with a first myocardial infarction, 77% with a first stroke, and 74% with chronic heart failure (Aronow, 2012).
- Trends:
- From 2005 to 2013, the overall rate of avoidable admissions for hypertension increased from 48.4 to 57.8 per 100,000 population.
- From 2005 to 2013, rates of avoidable admission for hypertension got worse for residents of the Northeast, Midwest, and West. There were no statistically significant changes for residents of the South.
- Groups With Disparities:
- Overall in 2013, rates of avoidable admission for hypertension were higher for Blacks and Hispanics than for Whites (200.5 and 67.8, respectively, compared with 35.8 per 100,000 population). Rates were lower for API s compared with Whites (30.9 vs. 35.8 per 100,000 population).
- In 2013, in all income groups, rates of avoidable admission for hypertension were higher for Blacks and Hispanics than for Whites. There were no statistically significant differences by income between APIs and Whites.
- Achievable Benchmark:
- The 2011 top 4 State achievable benchmark was 18%. The top 4 States that contributed to the achievable benchmark are Montana, Oregon, Utah, and Vermont.
- No group is making progress toward the benchmark.
Slide 39
Integration of Medication Information
- Poor communication between providers and between providers and patients, within and across care settings, has been identified as a source of medication error.
- Improving communication is a key aspect of decreasing medication errors and improving patient safety (Kitson, et al., 2013).
Slide 40
Integration of Medication Information
- Disparities in access to health information, services, and technology can result in:
- Less use of preventive services.
- Poorer chronic disease management.
- Higher hospitalization rates.
- Poorer reported health status (Berkman, et al., 2004).
- Patients need to understand their medication (indications, administration, adverse effects) to safely and effectively use it. But important medication information is given to patients in a haphazard way (Persell, 2013).
Slide 41
Integration of Medication Information Measures
- People under age 65 with a usual source of care whose health provider usually asks about prescription medications and treatments from other doctors.
- Hospitals with electronic exchange of patient medication history with hospitals outside their system.
- Hospitals with electronic exchange of patient medication history with ambulatory providers outside their system.
Slide 42
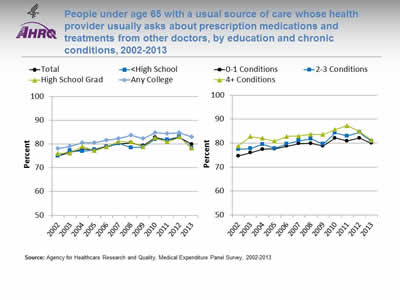
People under age 65 with a usual source of care whose health provider usually asks about prescription medications and treatments from other doctors, by education and chronic conditions, 2002-2013
Image: Charts show people under age 65 with a usual source of care whose health provider usually asks about prescription medications and treatments from other doctors:
Left Chart:
| Education | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 75.1 | 76.4 | 77.8 | 77.7 | 79 | 80.1 | 80.5 | 79.3 | 82.8 | 81.7 | 82.7 | 79.9 |
| Any College | 78.1 | 79 | 80.6 | 80.6 | 81.6 | 82.3 | 83.6 | 82.2 | 84.7 | 84.3 | 84.7 | 83 |
| High School Grad | 76 | 76.2 | 79 | 77.2 | 78.8 | 81.1 | 80.8 | 78.8 | 82.6 | 80.8 | 82.9 | 78.2 |
| <High School | 75 | 77.2 | 76.9 | 77.5 | 78.7 | 80.2 | 78.5 | 78.7 | 82 | 81.8 | 83.1 | 78.3 |
Right Chart:
| No. of Chronic Conditions | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-1 Conditions | 74.7 | 76.0 | 77.4 | 77.6 | 78.7 | 79.8 | 79.9 | 78.8 | 82.1 | 80.9 | 82.1 | 79.9 |
| 2-3 Conditions | 77.4 | 77.7 | 79.5 | 77.8 | 79.7 | 81.0 | 81.8 | 79.6 | 84.3 | 83.0 | 84.5 | 80.7 |
| 4+ Conditions | 78.8 | 82.7 | 82.0 | 80.8 | 82.8 | 83.0 | 83.7 | 83.6 | 85.7 | 87.3 | 84.9 | 81.3 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
Notes:
- Importance: Different providers may prescribe medications for the same patient. Patients must track all their medications, but medication information can be confusing, especially for patients on multiple medications. When care is not well coordinated and some providers do not know about all of a patient's medications, patients are at greater risk for adverse events related to drug interactions, overdosing, or underdosing. Medication information generated in different settings might not be sent to a patient's primary care provider, so the patient is the primary source of medication information. Actively gathering and managing all of a patient's medical information is an important part of care coordination.
- Trends:
- From 2002 to 2013, the percentage of people with a usual source of care whose health provider usually asked about prescription medications and treatments from other doctors improved from 75.1% to 79.9%.
- The percentage of people with a usual source of care whose health provider usually asked about prescription medications and treatments from other doctors showed improvement for patients of all educational levels and all groups with chronic conditions.
- Groups With Disparities:
- In 8 of 12 years, people with less than a high school education were less likely than people with any college to be asked about prescription medications and treatments from other doctors.
- In 7 of 12 years, high school graduates were less likely than people with any college to be asked about prescription medications and treatments from other doctors.
Slide 43
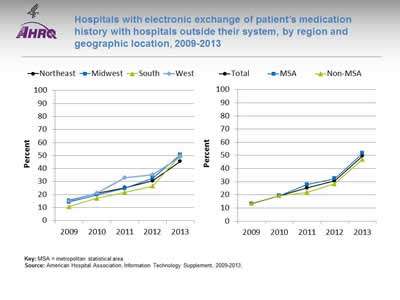
Hospitals with electronic exchange of patient's medication history with hospitals outside their system, by region and geographic location, 2009-2013
Image: Charts show hospitals with electronic exchange of patient's medication history with hospitals outside their system:
Left Chart:
| Region | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Northeast | 15.6 | 21 | 25.3 | 30.5 | 45.6 |
| Midwest | 14.3 | 19.9 | 24.8 | 32.6 | 50.7 |
| South | 10.8 | 17.2 | 21.8 | 26.5 | 50.4 |
| West | 15 | 21.1 | 32.9 | 35.3 | 49 |
Right Chart:
| Location | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Total | 13.4 | 19.4 | 25.2 | 30.7 | 49.6 |
| MSA | 13.3 | 19.4 | 27.8 | 32.4 | 51.7 |
| Non-MSA | 13.5 | 19.4 | 22 | 28.5 | 47 |
Key: MSA = metropolitan statistical area.
Source: American Hospital Association, Information Technology Supplement, 2009-2013.
Notes:
- Importance: Health information exchange enables patients’ health information to follow them between delivery settings in order to support care coordination and avoid duplication of services. There is broad consensus that such connectivity is critical to improving care and reducing health care costs.
- Trends:
- From 2009 to 2013, the percentage of hospitals with electronic exchange of patient’s medication history with hospitals outside their system increased from 13.4% to 49.6%.
- From 2009 to 2013, the percentage of hospitals with electronic exchange of patient’s medication history with hospitals outside their system more than tripled for residents of all regions.
- From 2009 to 2013, the percentage of metropolitan hospitals that electronically exchanged patient medication history with hospitals outside their system significantly increased from 13.3% to 51.7%. The percentage of nonmetropolitan hospitals that electronically exchanged medication history increased from 13.5% to 47.0%.
- Differences:
- In 2013, hospitals in the Midwest were most likely to have electronic exchange with hospitals outside their system, followed by the South, West, and Northeast (50.7%, 50.4%, 49.0%, and 45.6%, respectively).
Slide 44
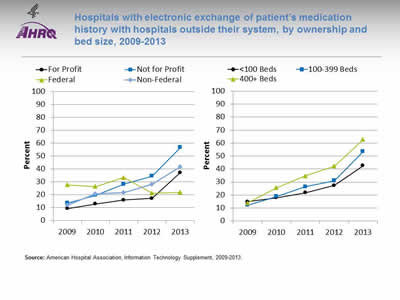
Hospitals with electronic exchange of patient's medication history with hospitals outside their system, by ownership and bed size, 2009-2013
Image: Charts show hospitals with electronic exchange of patient's medication history with hospitals outside their system:
Left Chart:
| Hospital Type | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| For Profit | 9.4 | 12.9 | 16.0 | 17.2 | 37.2 |
| Not for Profit | 13.6 | 19.7 | 28.3 | 34.5 | 56.8 |
| Federal | 27.7 | 26.4 | 33.3 | 21.3 | 22 |
| Non-Federal | 12.0 | 20.6 | 21.8 | 28.3 | 41.8 |
Right Chart:
| Hospital Size | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| <100 Beds | 14.8 | 17.9 | 21.7 | 27.3 | 42.6 |
| 100-399 Beds | 12.1 | 18.9 | 26.4 | 31.1 | 53.5 |
| 400+ Beds | 13.9 | 25.6 | 34.8 | 42.3 | 62.7 |
Source: American Hospital Association, Information Technology Supplement, 2009-2013.
Notes:
- Importance: Health information exchange enables patients’ health information to follow them between delivery settings in order to support care coordination and avoid duplication of services. There is broad consensus that such connectivity is critical to improving care and reducing health care costs.
- Trends:
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with hospitals outside their system increased:
- From 9.4% to 37.2% for for-profit hospitals.
- From 13.6% to 56.8% for not-for-profit hospitals.
- From 12.0% to 41.8% for non-Federal hospitals.
- For Federal hospitals, the percentage decreased from 27.7% to 22.0%.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with hospitals outside their system increased:
- From 14.8% to 42.6% for hospitals with fewer than 100 beds.
- From 12.1% to 53.5% for hospitals with 100-399 beds.
- From 13.9% to 62.7% for hospitals with 400 or more beds.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with hospitals outside their system increased:
- Differences:
- In 4 of 5 years, hospitals with fewer than 100 beds were less likely than large hospitals (400+ beds) to exchange information with hospitals outside their system.
- In 3 of 5 years, hospitals with 100-399 beds were less likely than large hospitals (400+ beds) to exchange information with hospitals outside their system.
Slide 45
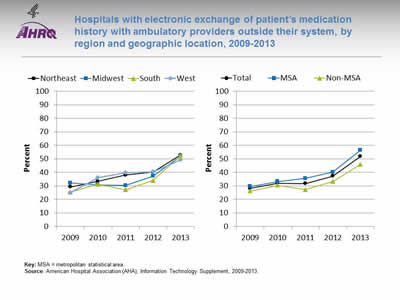
Hospitals with electronic exchange of patient's medication history with ambulatory providers outside their system, by region and geographic location, 2009-2013
Image: Charts show hospitals with electronic exchange of patient's medication history with ambulatory providers outside their system:
Left Chart:
| Region | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Northeast | 29.2 | 33.4 | 38.0 | 40.2 | 52.8 |
| Midwest | 32.2 | 30.6 | 30.3 | 37.3 | 52 |
| South | 25.4 | 31.2 | 27.1 | 34.1 | 52.3 |
| West | 24.9 | 36.1 | 39.9 | 40.5 | 49.4 |
Right Chart:
| Location | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Total | 28.2 | 32.1 | 31.8 | 37.2 | 51.8 |
| MSA | 29.6 | 33.3 | 35.6 | 40.2 | 56.4 |
| Non-MSA | 26.2 | 30.5 | 27.2 | 33.3 | 45.9 |
Key: MSA = metropolitan statistical area.
Source: American Hospital Association (AHA), Information Technology Supplement, 2009-2013.
Notes:
- Importance: Health information exchange enables patients’ health information to follow them between delivery settings in order to support care coordination and avoid duplication of services. There is broad consensus that such connectivity is critical to improving care and reducing health care costs.
- Trends:
- From 2009 to 2013, the percentage of hospitals with electronic exchange of patient medication history with ambulatory providers outside their system increased from 28.2% to 51.8%.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with ambulatory providers outside their system increased:
- From 29.2% to 52.8% in the Northeast.
- From 32.2% to 52.0% in the Midwest.
- From 25.4% to 52.3% in the South.
- From 24.9% to 49.4% in the West.
- From 2009 to 2013, the percentage of metropolitan hospitals that electronically exchanged patient medication history with ambulatory providers outside their system significantly increased from 29.6% to 56.4%. The percentage of nonmetropolitan hospitals that electronically exchanged patient medication history increased from 26.2% to 45.9%.
- Differences:
- In 2013, hospitals in metropolitan areas (56.4%) were more likely to exchange information with ambulatory providers outside their system than hospitals in nonmetropolitan areas (45.9%).
Slide 46
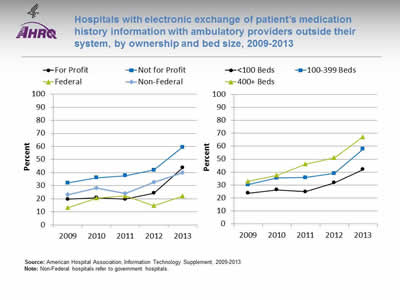
Hospitals with electronic exchange of patient's medication history information with ambulatory providers outside their system, by ownership and bed size, 2009-2013
Image: Charts show hospitals with electronic exchange of patient's medication history information with ambulatory providers outside their system:
Left Chart:
| Hospital Type | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| For Profit | 19.6 | 20.8 | 19.7 | 24.3 | 43.7 |
| Not for Profit | 32.0 | 36.0 | 37.7 | 42 | 59.4 |
| Federal | 13.2 | 20.5 | 22.2 | 14.7 | 22 |
| Non-Federal | 23.0 | 28.1 | 24.2 | 32.5 | 39.8 |
Right Chart:
| Hospital Size | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| <100 Beds | 23.7 | 26.4 | 24.9 | 31.8 | 42.1 |
| 100-399 Beds | 30.4 | 35.5 | 35.8 | 39 | 57.8 |
| 400+ Beds | 32.9 | 37.5 | 46.2 | 51.1 | 67.3 |
Source: American Hospital Association, Information Technology Supplement, 2009-2013.
Notes: Non-Federal hospitals refer to government hospitals.
- Importance: Health information exchange enables patients’ health information to follow them between delivery settings in order to support care coordination and avoid duplication of services. There is broad consensus that such connectivity is critical to improving care and reducing health care costs.
- Trends:
- From 2009 to 2013, the percentage of hospitals that electronically exchanged medication history with ambulatory providers outside their system increased:
- From 19.6% to 43.7% for for-profit hospitals.
- From 32.0% to 59.4% for not-for-profit hospitals.
- From 13.2% to 22% for Federal hospitals.
- From 23.0% to 39.8% for non-Federal hospitals.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged patient medication history with hospitals outside their system increased:
- From 23.7% to 42.1% for hospitals with fewer than 100 beds.
- From 30.4% to 57.8% for hospitals with 100-399 beds.
- From 32.9% to 67.3% for hospitals with 400 or more beds.
- From 2009 to 2013, the percentage of hospitals that electronically exchanged medication history with ambulatory providers outside their system increased:
- Differences:
- In all years, not-for-profit hospitals were more likely to have electronic exchange with ambulatory providers outside their system than for-profit and Federal hospitals.
- In all years, hospitals with fewer than 100 beds were less likely than hospitals with 400 or more beds to electronically exchange medication history with ambulatory providers outside their system.
Slide 47
Use of Electronic Health Records
- Electronic health records (EHRs) can improve the quality and safety of health care.
- The adoption and effective use of health information technology can:
- Help reduce medical errors and adverse events.
- Enable better documentation and file organization.
- Provide patients with information that assists their adherence to medication regimens and scheduled appointments.
- Assist doctors in tracking their treatment protocols (IOM, 2010).
Slide 48
Electronic Health Record Measures
- Patients who reported that it was very important for them to get their own medical information electronically.
- Patients who reported that it was very important that doctors and other health providers be able to share their medical information with other providers electronically.
- Hospitals with fully implemented electronic medical record system.
- Hospitals with computerized systems that allow electronic clinical documentation.
- Hospitals with computerized systems that allow results viewing.
- Hospitals with computerized systems that allow decision support.
- Hospitals with computerized systems that allow computerized provider order entry (CPOE).
Slide 49
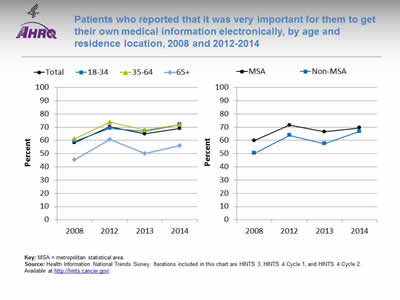
Patients who reported that it was very important for them to get their own medical information electronically, by age and residence location, 2008 and 2012-2014
Image: Charts show patients who reported that it was very important for them to get their own medical information electronically:
Left Chart:
| Age | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| Total | 58.3 | 70.3 | 64.9 | 69.1 |
| 18-34 | 59.4 | 69.2 | 67 | 72.1 |
| 35-64 | 61.3 | 73.9 | 67.9 | 72 |
| 65+ | 45.5 | 60.8 | 50.1 | 56.2 |
Right Chart:
| Location | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| MSA | 59.9 | 71.6 | 66.5 | 69.5 |
| Non-MSA | 50.3 | 63.8 | 57.5 | 66.9 |
Key: MSA = metropolitan statistical area.
Source: Health Information National Trends Survey. Iterations included in this chart are HINTS 3, HINTS 4 Cycle 1, and HINTS 4 Cycle 2. Available at http://hints.cancer.gov/.
Notes:
- Importance: The 2009 U.S. Health Information Technology for Economic and Clinical Health (HITECH) Act called for the creation of a meaningful use incentive program to provide financial support to providers and health systems that adopt electronic health record (EHR) technologies. Stage 2 of the meaningful use incentive program requires the active engagement of patients and their families with patient portal technology in managing their own health information and care coordination (Ford, et al., 2016).
- Trends:
- From 2008 to 2014, the percentage of patients who reported that it was very important for them to get their own medical information electronically increased from 58.3% to 69.1%.
- From 2009 to 2014, the percentage of patients in metropolitan areas who reported that it was very important for them to get their own medical information electronically increased from 59.9% to 69.5%. Among residents of nonmetropolitan areas, the percentage increased from 50.3% to 66.9%.
- Differences Between Groups:
- In all years, patients age 65 and over were less likely than patients ages 35-64 to report that it was very important for them to get their own medical information electronically.
- In all years except 2014, residents of nonmetropolitan areas were less likely than residents of metropolitan areas to report that it was very important for them to get their own medical information electronically.
Slide 50
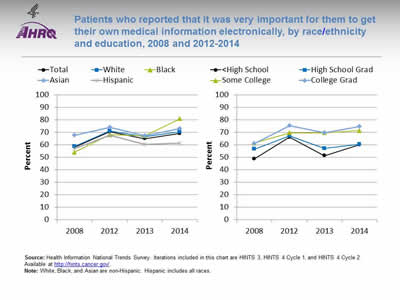
Patients who reported that it was very important for them to get their own medical information electronically, by race/ethnicity and education, 2008 and 2012-2014
Image: Charts show patients who reported that it was very important for them to get their own medical information electronically:
Left Chart:
| Race/Ethnicity | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| Total | 58.3 | 70.3 | 64.9 | 69.1 |
| White | 58.8 | 71.1 | 66.4 | 70.3 |
| Black | 54.1 | 68.1 | 67.2 | 80.9 |
| Asian | 67.6 | 73.8 | 67.2 | 73 |
| Hispanic | 57.1 | 67.6 | 60.2 | 61.2 |
Right Chart:
| Education | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| <High School | 48.8 | 66.1 | 51.3 | 60.1 |
| High School Grad | 56.5 | 67.1 | 57.1 | 60.3 |
| Some College | 61.3 | 69.5 | 69.6 | 71.4 |
| College Grad | 60.8 | 75.1 | 69.5 | 74.5 |
Source: Health Information National Trends Survey. Iterations included in this chart are HINTS 3, HINTS 4 Cycle 1, and HINTS 4 Cycle 2. Available at http://hints.cancer.gov/.
Notes: White, Black, and Asian are non-Hispanic. Hispanic includes all races.
- Importance: The 2009 U.S. Health Information Technology for Economic and Clinical Health (HITECH) Act called for the creation of a meaningful use incentive program to provide financial support to providers and health systems that adopt electronic health record technologies. Stage 2 of the meaningful use incentive program requires the active engagement of patients and their families with patient portal technology in managing their own health information and care coordination (Ford, et al., 2016).
- Trends:
- From 2008 to 2014, the percentage of patients who reported that it was very important for them to get their own medical information electronically increased:
- From 58.8% to 70.3% for Whites.
- From 54.1% to 80.9% for Blacks.
- From 67.6% to 73.0% for Asians.
- From 57.1% to 61.2% for Hispanics.
- From 2008 to 2014, the percentage of patients who reported that it was very important for them to get their own medical information electronically increased:
- From 60.8% to 74.5% for college graduates.
- From 61.3% to 71.4% for patients with some college education.
- From 56.5% to 60.3% for high school graduates.
- From 48.8% to 60.1% for patients with less than a high school education.
- From 2008 to 2014, the percentage of patients who reported that it was very important for them to get their own medical information electronically increased:
- Differences Between Groups:
- In 2013, Black patients were more likely than White patients to report that it was very important for them to get their own medical information electronically.
- In 2013 and 2014, Hispanic patients were less likely than White patients to report that it was very important for them to get their own medical information electronically.
Slide 51
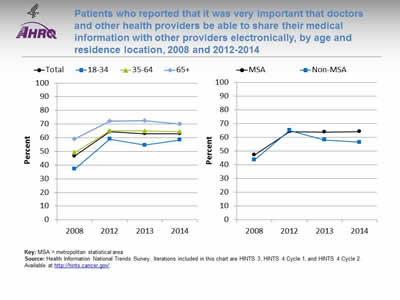
Patients who reported that it was very important that doctors and other health providers be able to share their medical information with other providers electronically, by age and residence location, 2008 and 2012-2014
Image: Charts show patients who reported that it was very important that doctors and other health providers be able to share their medical information with other providers electronically:
Left Chart:
| Age | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| Total | 46.7 | 64.4 | 63 | 63 |
| 18-34 | 37.2 | 59.1 | 54.7 | 58.5 |
| 35-64 | 49.3 | 65.1 | 64.9 | 64.5 |
| 65+ | 59.2 | 72.3 | 72.4 | 70 |
Right Chart:
| Location | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| MSA | 47.3 | 64.3 | 64 | 64.3 |
| Non-MSA | 43.6 | 65.1 | 58.2 | 56.6 |
Key: MSA = metropolitan statistical area.
Source: Health Information National Trends Survey. Iterations included in this chart are HINTS 3, HINTS 4 Cycle 1, and HINTS 4 Cycle 2. Available at http://hints.cancer.gov/.
Notes:
- Importance: Richer information flowing between and within practices can enhance primary care provider decisionmaking and improve care coordination (Cross, et al., 2015).
- Trends:
- From 2008 to 2014, the percentage of patients who reported that it was very important that health providers be able to share their medical information with other providers electronically increased from 46.7% to 63.0%.
- From 2008 to 2014, the percentage of patients of metropolitan areas who reported that it was very important that health providers be able to share their medical information with other providers electronically increased from 47.3% to 64.3%. The percentage for residents of nonmetropolitan areas increased from 43.6% to 56.6%.
- Differences Between Groups:
- In all years, patients ages 18-34 were less likely than patients age 65 and over to report that it was very important that health providers be able to share their medical information with other providers electronically.
- In 2013 and 2014, patients in metropolitan areas more likely than patients in nonmetropolitan areas to report that it was very important that health providers be able to share their medical information with other providers electronically.
Slide 52
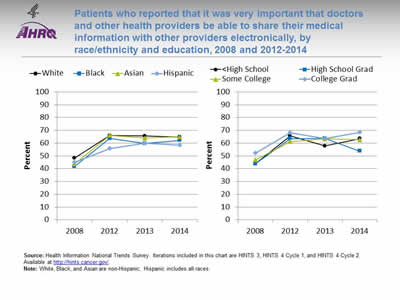
Patients who reported that it was very important that doctors and other health providers be able to share their medical information with other providers electronically, by race/ethnicity and education, 2008 and 2012-2014
Image: Charts show patients who reported that it was very important that doctors and other health providers be able to share their medical information with other providers electronically:
Left Chart:
| Race/Ethnicity | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| White | 48.4 | 65.9 | 65.6 | 64.8 |
| Black | 41.8 | 63.7 | 59.7 | 62.1 |
| Asian | 43.8 | 66.1 | 64 | 64.9 |
| Hispanic | 45.1 | 55.6 | 59.9 | 58.3 |
Right Chart:
| Education | 2008 | 2012 | 2013 | 2014 |
|---|---|---|---|---|
| <High School | 43.7 | 65.7 | 57.7 | 63.4 |
| High School Grad | 43.7 | 63.4 | 63.7 | 53.7 |
| Some College | 46.8 | 61.2 | 63.3 | 62.7 |
| College Grad | 52.2 | 68.1 | 63.6 | 68.4 |
Source: Health Information National Trends Survey. Iterations included in this chart are HINTS 3, HINTS 4 Cycle 1, and HINTS 4 Cycle 2. Available at http://hints.cancer.gov/.
Notes: White, Black, and Asian are non-Hispanic. Hispanic includes all races.
- Importance: Richer information flowing between and within practices can enhance primary care provider decisionmaking and improve care coordination (Cross, et al., 2015).
- Trends:
- From 2008 to 2014, the percentage of patients who reported that it was very important that health providers be able to share their medical information with other providers electronically increased:
- From 48.4% to 64.8% for Whites.
- From 41.8% to 62.1% for Blacks.
- From 43.8% to 64.9% for Asians.
- From 45.1% to 58.3% for Hispanics.
- From 2008 to 2014, the percentage of patients who reported that it was very important that health providers be able to share their medical information with other providers electronically increased:
- From 52.2% to 68.4% for college graduates.
- From 46.8% to 62.7% for patients with some college.
- From 43.7% to 53.7% for high school graduates.
- From 43.7% to 63.4% for patients with less a high school education.
- From 2008 to 2014, the percentage of patients who reported that it was very important that health providers be able to share their medical information with other providers electronically increased:
- Differences Between Groups:
- From 2012 to 2014, Hispanic patients were less likely than White patients to report that it was very important that health providers be able to share their medical information with other providers electronically.
Slide 53
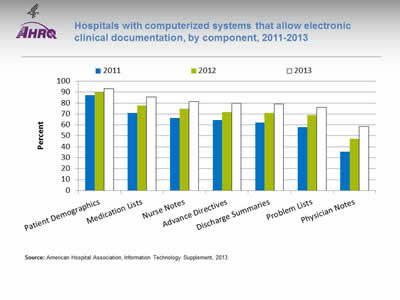
Hospitals with computerized systems that allow electronic clinical documentation, by component, 2011-2013
Image: Chart shows hospitals with computerized systems that allow electronic clinical documentation:
| Component | 2011 | 2012 | 2013 |
|---|---|---|---|
| Patient Demographics | 87.1 | 89.9 | 93 |
| Medication Lists | 71 | 77.7 | 85.4 |
| Nurse Notes | 66.5 | 74.6 | 81.4 |
| Advance Directives | 64.3 | 71.5 | 79.7 |
| Discharge Summaries | 62.1 | 70.9 | 79.1 |
| Problem Lists | 58 | 68.9 | 76.2 |
| Physician Notes | 35.5 | 47.5 | 58.4 |
Source: American Hospital Association, Information Technology Supplement, 2013.
Notes:
- Importance: Compared with paper, electronic provider documentation allows faster and more complete access to the patient record and may improve communication among members of the health care team. Some evidence exists that electronic documentation may be associated with improved patient outcomes and decreased costs (Hripcsak, et al., 2011).
- Overall Rate: In 2013, 52.4% of hospitals had a computerized system for electronic clinical documentation, an increase from 29.6% in 2011 (data not shown).
- Trends:
- From 2011 to 2013, among hospitals with computerized systems that allow electronic clinical documentation, each component improved as follows:
- Patient demographics, 87.1% to 93.0%.
- Medication lists, 71.0% to 85.4%.
- Nursing notes, 66.5% to 81.4%.
- Advance directives, 64.3% to 79.7%.
- Discharge summaries, 62.1% to 79.1%.
- Problem lists, 58.0% to 76.2%.
- Physician notes, 35.5% to 58.4%.
- From 2011 to 2013, among hospitals with computerized systems that allow electronic clinical documentation, each component improved as follows:
Slide 54
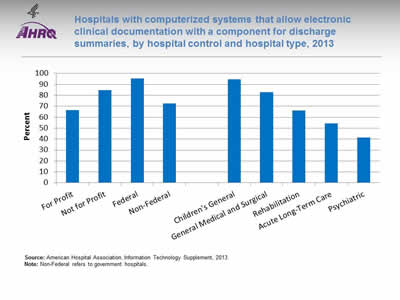
Hospitals with computerized systems that allow electronic clinical documentation with a component for discharge summaries, by hospital control and hospital type, 2013
Image: Chart shows hospitals with computerized systems that allow electronic clinical documentation with a component for discharge summaries:
- For Profit - 66.6.
- Not for Profit - 84.7.
- Federal - 95.5.
- Non-Federal - 72.5.
- Children's General - 94.5.
- General Medical and Surgical - 83.
- Rehabilitation - 66.2.
- Acute Long-Term Care - 54.3.
- Psychiatric - 41.3.
Source: American Hospital Association, Information Technology Supplement, 2013.
Notes: Non-Federal refers to government hospitals.
- Importance: Compared with paper, electronic provider documentation allows faster and more complete access to the patient record and may improve communication among members of the health care team. Some evidence exists that electronic documentation may be associated with improved patient outcomes and decreased costs.
- Differences:
- In 2013, 66.6% of for-profit hospitals, 84.7% of not-for-profit hospitals, 95.5% of hospitals run by the Federal Government, and 72.5% of non-Federal hospitals and had a computerized system for electronic clinical documentation with a component for discharge summaries.
- In 2013, 94.5% of children’s general, 83.0% of general medical and surgical, 66.2% of rehabilitation, 54.3% of acute long-term care, and 41.3% of psychiatric hospitals had a computerized system for electronic clinical documentation with a component for discharge summaries.
Slide 55
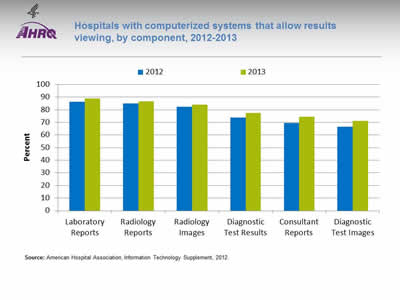
Hospitals with computerized systems that allow results viewing, by component, 2012-2013
Image: Chart shows hospitals with computerized systems that allow results viewing:
| Component | 2012 | 2013 |
|---|---|---|
| Laboratory Reports | 86.2 | 89.1 |
| Radiology Reports | 85 | 86.8 |
| Radiology Images | 82.3 | 84.2 |
| Diagnostic Test Results | 73.9 | 77.5 |
| Consultant Reports | 69.6 | 74.4 |
| Diagnostic Test Images | 66.7 | 71.3 |
Source: American Hospital Association, Information Technology Supplement, 2012.
Notes:
- Importance: Use of EHRs directly affects the communication and management of laboratory information in patient care, particularly results reporting and test order management (Henricks, 2011).
- Overall Rate: In 2013, 64.1% of hospitals had a computerized system that allows results viewing, an increase from 58.2% in 2012 (data not shown).
- Trends:
- From 2012 to 2013, among hospitals with computerized systems that allow results viewing, the percentage of hospitals with the following components increased:
- Laboratory reports, from 86.2% to 89.1%.
- Radiology reports, from 85.0% to 86.8%.
- Radiology images, from 82.3% to 84.2%.
- Diagnostic test results, from 73.9% to 77.5%.
- Consultant reports, from 69.6% to 74.4%.
- Diagnostic test images, from 66.7% to 71.3%.
- From 2012 to 2013, among hospitals with computerized systems that allow results viewing, the percentage of hospitals with the following components increased:
Slide 56
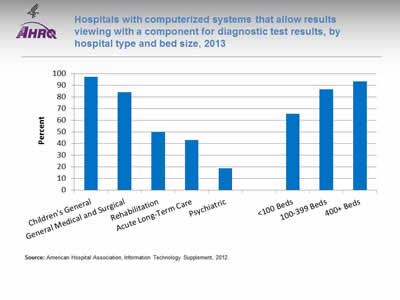
Hospitals with computerized systems that allow results viewing with a component for diagnostic test results, by hospital type and bed size, 2013
Image: Chart shows hospitals with computerized systems that allow results viewing with a component for diagnostic test results:
- Children's General - 97.3.
- General Medical and Surgical - 84.1.
- Rehabilitation - 50.
- Acute Long-Term Care - 43.2.
- Psychiatric - 18.8.
- <100 Beds - 65.5.
- 100-399 Beds - 86.8.
- 400+ Beds - 93.4.
Source: American Hospital Association, Information Technology Supplement, 2012.
Notes:
- Importance: Use of EHRs directly affects the communication and management of laboratory information in patient care, particularly reporting results and test order management (Henricks, 2011).
- Differences:
- In 2013, 97.3% of children’s general, 84.1% of general medical and surgical, 50.0% of rehabilitation, 43.2% of acute long-term care, and 18.8% of psychiatric hospitals had a computerized system for results viewing with a component for diagnostic test results.
- In 2013, among hospitals with computerized systems for results viewing, the percentage with a component for diagnostic test results was highest in hospitals with more than 400 beds (93.4%), followed by hospitals with 100-399 beds (86.8%), and hospitals with fewer than 100 beds (65.5%).
Slide 57
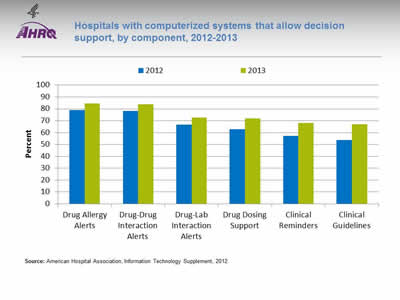
Hospitals with computerized systems that allow decision support, by component, 2012-2013
Image: Chart shows hospitals with computerized systems that allow decision support:
| Component | 2012 | 2013 |
|---|---|---|
| Drug Allergy Alerts | 79 | 84.5 |
| Drug-Drug Interaction Alerts | 78.3 | 83.9 |
| Drug-Lab Interaction Alerts | 66.6 | 72.7 |
| Drug Dosing Support | 62.9 | 71.8 |
| Clinical Reminders | 57.3 | 68.1 |
| Clinical Guidelines | 53.8 | 67 |
Source: American Hospital Association, Information Technology Supplement, 2012.
Notes:
- Importance: Clinical decision support (CDS) systems, which provide appropriate, timely, patient-specific reminders and information, are essential to cope with the growth in medical knowledge. When implemented effectively, CDS has been shown to improve quality and can be particularly effective for increasing appropriate use of evidence-based preventive services (Wright, et al., 2015).
- Overall Rate: In 2013, 56.0% of hospitals had a computerized system for clinical decision support, an increase from 44.9% in 2012 (data not shown).
- Trends:
- From 2012 to 2013, among hospitals with computerized systems that allow clinical decision support, the percentage with the following components improved:
- Drug allergy alerts, from 79.0% to 84.5%.
- Drug-drug interaction alerts, from 78.3% to 83.9%.
- Drug-lab interaction alerts, from 66.6% to 72.7%.
- Drug dosing support, from 62.9% to 71.8%.
- Clinical reminders, from 57.3% to 68.1%.
- Clinical guidelines, from 53.8% to 67.0%.
- From 2012 to 2013, among hospitals with computerized systems that allow clinical decision support, the percentage with the following components improved:
Slide 58
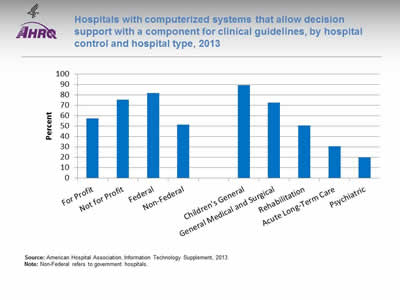
Hospitals with computerized systems that allow decision support with a component for clinical guidelines, by hospital control and hospital type, 2013
Image: Chart shows hospitals with computerized systems that allow decision support with a component for clinical guidelines:
- For Profit - 57.3.
- Not for Profit - 75.4.
- Federal - 81.8.
- Non-Federal - 51.3.
- Children's General - 89.4.
- General Medical and Surgical - 72.4.
- Rehabilitation - 50.6.
- Acute Long-Term Care - 30.7.
- Psychiatric - 19.9.
Source: American Hospital Association, Information Technology Supplement, 2013.
Notes: Non-Federal refers to government hospitals.
- Importance: CDS systems, which provide appropriate, timely, patient-specific reminders and information, are essential to cope with the growth in medical knowledge. When implemented effectively, CDS has been shown to improve quality and can be particularly effective for increasing appropriate use of evidence-based preventive services (Wright, et al.).
- Differences:
- In 2013, 57.3% of for-profit hospitals, 75.4% of not-for-profit hospitals, 81.8% of hospitals run by the Federal Government, and 51.3% of non-Federal hospitals had a component for clinical guidelines.
- In 2013, 89.4% of children’s general, 72.4% of general medical and surgical, 50.6% of rehabilitation, 30.7% of acute long-term care, and 19.9% of psychiatric hospitals had a component for clinical guidelines.
Slide 59
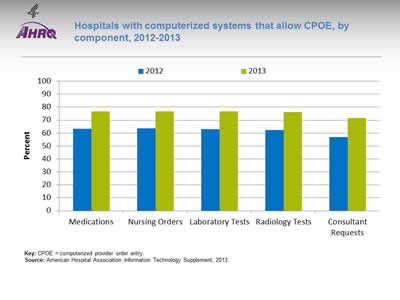
Hospitals with computerized systems that allow CPOE, by component, 2012-2013
Image: Chart shows hospitals with computerized systems that allow CPOE:
| Component | 2012 | 2013 |
|---|---|---|
| Medications | 63.2 | 76.8 |
| Nursing Orders | 63.6 | 76.8 |
| Laboratory Tests | 62.8 | 76.6 |
| Radiology Tests | 62.4 | 76 |
| Consultant Requests | 56.8 | 71.7 |
Key: CPOE = computerized provider order entry.
Source: American Hospital Association, Information Technology Supplement, 2013.
Notes:
- Importance: CPOE is associated with a 13% to 99% reduction in medication errors and a 30% to 84% reduction in adverse drug events (ADEs) (Ammenwerth, et al., 2008).
- Overall Rate: In 2013, 69.9% of hospitals had a computerized system for CPOE, an increase from 55.2% in 2012 (data not shown).
- Groups With Disparities:
- From 2012 to 2013, among hospitals with computerized systems that allow CPOE, the percentage with the following components improved:
- Medications, from 63.2% to 76.8%.
- Nursing orders, from 63.6% to 76.8%.
- Laboratory tests, from 62.8% to 76.6%.
- Radiology tests, from 62.4% to 76.0%.
- Consultant requests, from 56.8% to 71.7%.
- From 2012 to 2013, among hospitals with computerized systems that allow CPOE, the percentage with the following components improved:
Slide 60
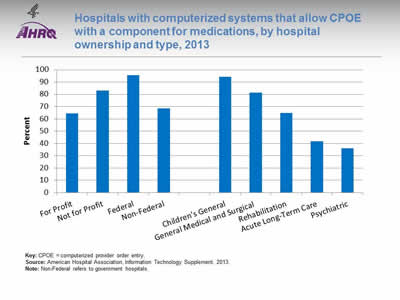
Hospitals with computerized systems that allow CPOE with a component for medications, by hospital ownership and type, 2013
Image: Chart shows hospitals with computerized systems that allow CPOE with a component for medications:
- For Profit - 64.3.
- Not for Profit - 82.9.
- Federal - 95.5.
- Non-Federal - 68.6.
- Children's General - 94.4.
- General Medical and Surgical - 81.4.
- Rehabilitation - 64.8.
- Acute Long-Term Care - 41.9.
- Psychiatric - 35.9.
Key: CPOE = computerized provider order entry.
Source: American Hospital Association, Information Technology Supplement, 2013.
Notes: Non-Federal refers to government hospitals.
- Importance: CPOE is associated with a 13% to 99% reduction in medication errors and a 30% to 84% reduction in adverse drug events (ADEs) (Ammenwerth, et al., 2008).
- Differences:
- In 2013, 64.3% of for-profit hospitals, 82.5% of not-for-profit hospitals, 95.5% of hospitals run by the Federal Government, and 68.6% of non-Federal hospitals had a component for medications.
- In 2013, 94.4% of children’s general, 81.4% of general medical and surgical, 64.8% of rehabilitation, 41.9% of acute long-term care, and 35.9% of psychiatric hospitals had a component for medications.
Slide 61
References
Ammenwerth E, Schnell-Inderst P, Machan C, et al. The effect of electronic prescribing on medication errors and adverse drug events: a systematic review. J Am Med Inform Assoc 2008 Sep-Oct;15(5):585-600. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2528040/. Accessed June 16, 2016.
Aronow WS. Treatment of systemic hypertension. Am J Cardiovasc Dis 2012;2(3):160-70. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3427981/. Accessed June 16, 2016.
Berkman ND, DeWalt DA, Pignone MP, et al. Literacy and health outcomes: summary. Evidence Report/Technology Assessment No. 87. Rockville, MD: Agency for Healthcare Research and Quality; 2004. AHRQ Publication No. 04-E007-1. http://www.ncbi.nlm.nih.gov/books/NBK37134/. Accessed June 16, 2016.
Cross DA, Cohen GR, Nong P, et al. Improving EHR capabilities to facilitate stage 3 meaningful use care coordination criteria. AMIA Annu Symp Proc 2015 Nov 5;2015:448-55. eCollection 2015. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4765570/. Accessed June 16, 2016.
Dean M, Oetzel J, Sklar DP. Communication in acute ambulatory care. Acad Med 2014 Dec;89(12):1617-22.
Desai AS, Stevenson LW. Rehospitalization for heart failure. Circulation 2012;126:501-6.
Dowd B, Karmarker M, Swenson T, et al. Emergency department utilization as a measure of physician performance. Am J Med Qual 2014;29(2):135-43. http://ajm.sagepub.com/content/29/2/135.long. Accessed June 16, 2016.
Enard KR, Ganelin DM. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. J Healthc Manag 2013;58(6);412-28. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4142498/. Accessed June 16, 2016.
Ford EW, Hesse BW, Huerta TR. Personal Health Record Use in the United States: Forecasting Future Adoption Levels. J Med Internet Res 2016 Mar 30;18(3):e73. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4830902/. Accessed June 16, 2016.
Forster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting patients after discharge from hospital. Ann Intern Med 2003;138(3):161-7.
Note: All Web pages listed in references were accessed June 16, 2016.
Slide 62

References
Gallahue FE, Betz AE, Druck J, et al. Ready for discharge? A survey of discharge transition-of-care education and evaluation in emergency medicine residency programs. West J Emerg Med 2015;16(6):879-84.
Gao J, Moran E, Li YF, et al. Predicting potentially avoidable hospitalizations. Med Care 2014 Feb;52(2):164-71.
Hasan O, Meltzer DO, Shaykevih SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med 2010;25(3):211-9. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2839332/. Accessed June 16, 2016.
HealthIT.gov. EHR Incentives and Certification. May 13, 2015. Available at https://www.healthit.gov/providers-professionals/meaningful-use-definition-objectives. Accessed June 16, 2016.
Henricks WH. "Meaningful use" of electronic health records and its relevance to laboratories and pathologists. J Pathol Inform 2011 Feb 11;2:7. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3049251/. Accessed June 16, 2016.
Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med 2013;173(18):1715-22. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3836871/. Accessed June 16, 2016.
Hripcsak G, Vawdrey DK, Fred MR, et al. Use of electronic clinical documentation: time spent and team interactions. J Am Inform Assoc 2011;18:112-7.
Institute of Medicine, Board of Health Care Services. Future directions for the National Healthcare Quality and Disparities Reports. Washington, DC: National Academies Press; 2010.
Kitson NA, Price M, Lau FY, et al. Developing a medication communication framework across continuums of care using the Circle of Care Modeling approach. BMC Health Serv Res 2013 Oct 17;13:418. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3853098/. Accessed June 16, 2016.
Kuppasani K, Reddi AS. Emergency or urgency? Effective management of hypertensive crises. JAAPA 2010 Aug;23(8):44-49.
Note: All Web pages listed in references were accessed June 16, 2016.
Slide 63
References
Nwankwo T, Yoon SS, Burt V, et al. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS data brief, no 133. Hyattsville, MD: National Center for Health Statistics. 2013. DHHS Publication No. 2014-1209. http://www.cdc.gov/nchs/data/databriefs/db133.pdf (777.33 KB). Accessed June 16, 2016.
Persell SD, Eder M, Friesema E, et al. EHR-based medication support and nurse-led medication therapy management: rationale and design for a three-arm clinic randomized trial. J Am Heart Assoc 2013 October;2(5):e000311. Published online 2013 Oct 25. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3835237/. Accessed June 16, 2016.
Rau J. Nearly 1,500 hospitals penalized under Medicare program rating quality. Kaiser Health News 2013 Nov 14. http://kaiserhealthnews.org/news/value-based-purchasing-medicare. Accessed June 16, 2016.
Rudd RA, Aleshire N, Zibbell JE, et al. Increases in drug and opoid overdose deaths—United States, 2000-2014. MMWR 2016;64(50):1378-82.
U.S. Department of Health and Human Services. 2011 report to Congress: national strategy for quality improvement in health care. Washington, DC: HHS; March 2011. http://www.ahrq.gov/workingforquality/reports/annual-reports/nqs2011annlrpt.htm. Accessed June 16, 2016.
U.S. Department of Health and Human Services. 2013 annual progress report to Congress: national strategy for quality improvement in health care. Washington, DC: HHS; July 2013, updated July 2014. http://www.ahrq.gov/workingforquality/reports/annual-reports/nqs2013annlrpt.htm. Accessed June 16, 2016.
Weinick RM, Burns RM, Mehrotra A. How many emergency department visits could be managed at urgent care centers and retail clinics? Health Aff 2010;29(9):1630-6. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3412873/. Accessed June 16, 2016.
Wright A, Sittig DF, Ash JS, et al. Lessons learned from implementing service-oriented clinical decision support at four sites: a qualitative study. Int J Med Inform 2015 Nov;84(11):901-11. http://www.sciencedirect.com/science/article/pii/S1386505615300320. Accessed June 16, 2016.
Note: All Web pages listed in references were accessed June 16, 2016.



