Chartbook on Healthy Living: Slide Presentation
National Healthcare Quality and Disparities Report
Slide 1
National Healthcare Quality and Disparities Report
Chartbook on Healthy Living
April 2016
Slide 2
Organization of the Chartbook on Healthy Living
- Part of a series related to the National Healthcare Quality and Disparities Report (QDR).
- Contents:
- Overview of the QDR.
- Overview of Healthy Living, one of the priorities of the National Quality Strategy.
- Summary of trends and disparities in Healthy Living from the QDR.
- Tracking of individual measures of Healthy Living:
- Maternal and Child Health Care.
- Lifestyle Modification.
- Clinical Preventive Services.
- Functional Status Preservation and Rehabilitation.
- Supportive and Palliative Care.
Slide 3
National Healthcare Quality and Disparities Report
- Annual report to Congress mandated in the Healthcare Research and Quality Act of 1999 (P.L. 106-129).
- Provides a comprehensive overview of:
- Quality of health care received by the general U.S. population.
- Disparities in care experienced by different racial, ethnic, and socioeconomic groups.
- Assesses the performance of our health system and identifies areas of strengths and weaknesses along three main axes:
- Access to health care.
- Quality of health care.
- Priorities of the National Quality Strategy.
Slide 4
National Healthcare Quality and Disparities Report
- Based on more than 250 measures of quality and disparities covering a broad array of health care services and settings.
- Includes data from 2015 QDR, which generally cover 2001-2013.
- Produced with the help of an Interagency Work Group led by the Agency for Healthcare Research and Quality and submitted on behalf of the Secretary of Health and Human Services.
Slide 5
Chartbooks Organized Around Priorities of the National Quality Strategy
- Making care safer by reducing harm caused in the delivery of care.
- Ensuring that each person and family is engaged as partners in their care.
- Promoting effective communication and coordination of care.
- Promoting the most effective prevention and treatment practices for the leading causes of mortality, starting with cardiovascular disease.
- Working with communities to promote wide use of best practices to enable healthy living.
- Making quality care more affordable for individuals, families, employers, and governments by developing and spreading new health care delivery models.
Note: Healthy Living is one of the six national priorities identified by the National Quality Strategy (http://www.ahrq.gov/workingforquality/index.html).
Slide 6
Priority 5: Working with communities to promote wide use of best practices to enable healthy living
Long-Term Goals
The National Quality Strategy has identified three long-term goals related to healthy living:
- Promote healthy living and well-being through community interventions that result in improvement of social, economic, and environmental factors.
- Promote healthy living and well-being through interventions that result in adoption of the most important healthy lifestyle behaviors across the lifespan.
- Promote healthy living and well-being through receipt of effective clinical preventive services across the lifespan in clinical and community settings.
Note:
- The broad goal of promoting better health is one that is shared across the country, whether it is promoting healthy behaviors, such as being tobacco free, or fostering healthy environments that make it easier to exercise and get access to healthy food.
- Successful efforts to improve these health factors rely on implementing evidence-based interventions through strong partnerships between local health care providers, public health professionals, and individuals.
Slide 7
Chartbook Contents
- This chartbook includes:
- Summary of trends across measures of Healthy Living from the QDR.
- Figures illustrating select measures of Healthy Living.
- Introduction and Methods contains information about methods used in the chartbook.
- A Data Query tool (http://nhqrnet.ahrq.gov/inhqrdr/data/query) provides access to all data tables.
Slide 8
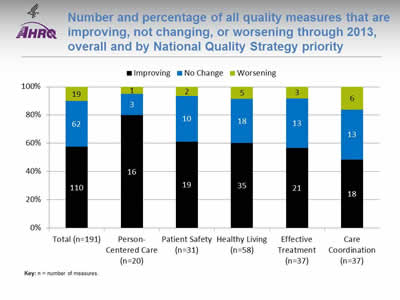
Number and percentage of all quality measures that are improving, not changing, or worsening through 2013, overall and by National Quality Strategy priority
Image: Chart shows number and percentage of all quality measures that are improving, not changing, or worsening through 2013:
| Quality Measures | Improving | No Change | Worsening |
|---|---|---|---|
| Total (n=191) | 110 | 62 | 19 |
| Person-Centered Care (n=20) | 16 | 3 | 1 |
| Patient Safety (n=31) | 19 | 10 | 2 |
| Healthy Living (n=58) | 35 | 18 | 5 |
| Effective Treatment (n=37) | 21 | 13 | 3 |
| Care Coordination (n=37) | 18 | 13 | 6 |
Key: n = number of measures.
Notes: For most measures, trend data are available from 2001-2002 through 2013. For each measure with at least four estimates over time, unweighted log-linear regression is used to calculate average annual percentage change and to assess statistical significance. Measures are aligned so that positive change indicates improved access to care.
- Improving = Rates of change are positive at 1% per year or greater and are statistically significant.
- No Change = Rates of change are less than 1% per year or are not statistically significant.
- Worsening = Rates of change are negative at -1% per year or greater and are statistically significant.
- Through 2013, across a broad spectrum of measures of health care quality, 60% showed improvement (black).
- About 80% of measures of Person-Centered Care improved.
- About 60% of measures of Effective Treatment, Healthy Living, and Patient Safety improved.
- Fewer than half of measures of Care Coordination improved.
- There are insufficient numbers of reliable measures of Care Affordability to summarize this way.
Slide 9
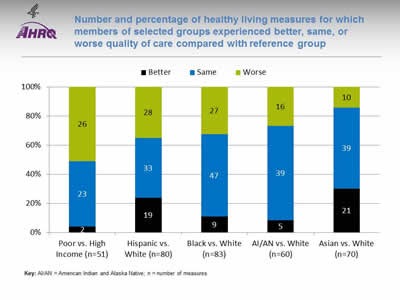
Number and percentage of healthy living measures for which members of selected groups experienced better, same, or worse quality of care compared with reference group
Image: Chart shows number and percentage of healthy living measures for which members of selected groups experienced better, same, or worse quality of care:
| Quality | Poor vs. High Income (n=51) | Hispanic vs. White (n=80) | Black vs. White (n=83) | AI/AN vs. White (n=60) | Asian vs. White (n=70) |
|---|---|---|---|---|---|
| Better | 2 | 19 | 9 | 5 | 21 |
| Same | 23 | 33 | 47 | 39 | 39 |
| Worse | 26 | 28 | 27 | 16 | 10 |
Key: AI/AN = American Indian and Alaska Native; n = number of measures.
Notes: Poor indicates family income less than the Federal poverty level; High Income indicates family income four times the Federal poverty level or greater. Numbers of measures differ across groups because of sample size limitations. For most measures, data from 2012 are shown. The relative difference between a selected group and its reference group is used to assess disparities.
- Better = Selected group received better quality of care than reference group. Differences are statistically significant, are equal to or larger than 10%, and favor the selected group.
- Same = Selected group and reference group received about the same quality of care. Differences are not statistically significant or are smaller than 10%.
- Worse = Selected group received worse quality of care than reference group. Differences are statistically significant, are equal to or larger than 10%, and favor the reference group.
- People in poor households received worse care than people in high-income households for about half of healthy living measures.
- Hispanics, Blacks, and American Indians and Alaska Natives received worse care than Whites for about one-third of health living measures.
Slide 10
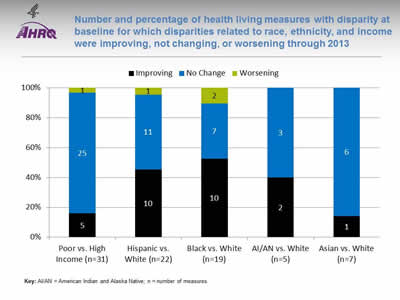
Number and percentage of health living measures with disparity at baseline for which disparities related to race, ethnicity, and income were improving, not changing, or worsening through 2013
Image: Chart shows number and percentage of health living measures with disparity at baseline for which disparities related to race, ethnicity, and income were improving, not changing, or worsening through 2013:
| Disparity | Poor vs. High Income (n=31) | Hispanic vs. White (n=22) | Black vs. White (n=19) | AI/AN vs. White (n=5) | Asian vs. White (n=7) |
|---|---|---|---|---|---|
| Worsening | 1 | 1 | 2 | ||
| No Change | 25 | 11 | 7 | 3 | 6 |
| Improving | 5 | 10 | 10 | 2 | 1 |
Key: AI/AN = American Indian and Alaska Native; n = number of measures.
Notes: Poor indicates family income less than the Federal poverty level; High Income indicates family income four times the Federal poverty level or greater. Number of measures differs across groups because of sample size limitations. For most measures, trend data are available from 2001-2002 to 2013.
For each measure with a disparity at baseline, average annual percentage changes were calculated for select populations and reference groups. Measures are aligned so that positive rates indicate improvement in care. Differences in rates between groups were used to assess trends in disparities.
- Worsening = Disparities are getting larger. Differences in rates between groups are statistically significant and reference group rates exceed population rates by at least 1% per year.
- No Change = Disparities are not changing. Differences in rates between groups are not statistically significant or differ by less than 1% per year.
- Improving = Disparities are getting smaller. Differences in rates between groups are statistically significant and population rates exceed reference group rates by at least 1% per year.
- Through 2013, about 40% of disparities at baseline for Hispanics and American Indians and Alaska Natives were getting smaller (black).
- More than half of disparities at baseline for Blacks were getting smaller.
- About 15% of disparities at baseline for Asians and people living in poor households were getting smaller.
Slide 11
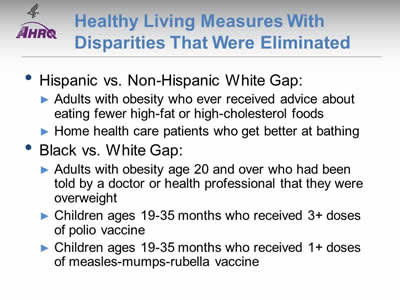
Healthy Living Measures With Disparities That Were Eliminated
- Hispanic vs. Non-Hispanic White Gap:
- Adults with obesity who ever received advice about eating fewer high-fat or high-cholesterol foods.
- Home health care patients who get better at bathing.
- Black vs. White Gap:
- Adults with obesity age 20 and over who had been told by a doctor or health professional that they were overweight.
- Children ages 19-35 months who received 3+ doses of polio vaccine.
- Children ages 19-35 months who received 1+ doses of measles-mumps-rubella vaccine.
Slide 12
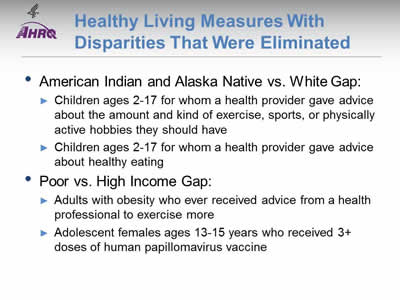
Healthy Living Measures With Disparities That Were Eliminated
- American Indian and Alaska Native vs. White Gap:
- Children ages 2-17 for whom a health provider gave advice about the amount and kind of exercise, sports, or physically active hobbies they should have.
- Children ages 2-17 for whom a health provider gave advice about healthy eating.
- Poor vs. High Income Gap:
- Adults with obesity who ever received advice from a health professional to exercise more.
- Adolescent females ages 13-15 years who received 3+ doses of human papillomavirus vaccine.
Slide 13
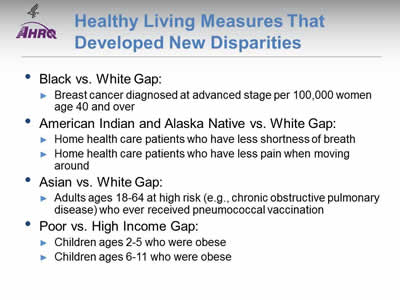
Healthy Living Measures That Developed New Disparities
- Black vs. White Gap:
- Breast cancer diagnosed at advanced stage per 100,000 women age 40 and over.
- American Indian and Alaska Native vs. White Gap:
- Home health care patients who have less shortness of breath.
- Home health care patients who have less pain when moving around.
- Asian vs. White Gap:
- Adults ages 18-64 at high risk (e.g., chronic obstructive pulmonary disease) who ever received pneumococcal vaccination.
- Poor vs. High Income Gap:
- Children ages 2-5 who were obese.
- Children ages 6-11 who were obese.
Slide 14
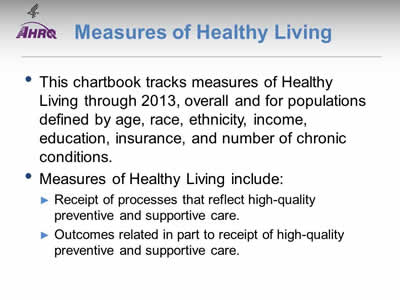
Measures of Healthy Living
- This chartbook tracks measures of Healthy Living through 2013, overall and for populations defined by age, race, ethnicity, income, education, insurance, and number of chronic conditions.
- Measures of Healthy Living include:
- Receipt of processes that reflect high-quality preventive and supportive care.
- Outcomes related in part to receipt of high-quality preventive and supportive care.
Slide 15
Services That Promote Healthy Living
- Much valuable health care is delivered to prevent disease, disability, and discomfort rather than to treat specific clinical conditions.
- These services improve health and quality of life and are often better characterized by stage over a lifespan rather than by organ system.
Slide 16
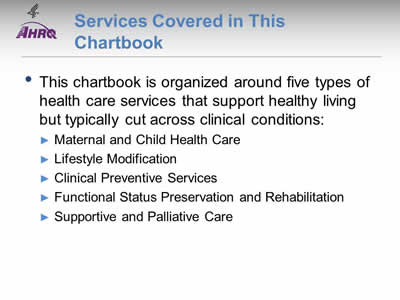
Services Covered in This Chartbook
- This chartbook is organized around five types of health care services that support healthy living but typically cut across clinical conditions:
- Maternal and Child Health Care.
- Lifestyle Modification.
- Clinical Preventive Services.
- Functional Status Preservation and Rehabilitation.
- Supportive and Palliative Care.
Slide 17
Chartbook on Healthy Living
Maternal and Child Health Care
Slide 18
Maternal and Child Health Care Measures
- Access:
- Periods of uninsurance.
- Effectiveness:
- Prenatal care.
- Receipt of recommended immunizations by young children.
- Children's vision screening.
- Well-child visits in the last year.
- Receipt of meningococcal vaccine by adolescents.
- Receipt of human papillomavirus (HPV) vaccination by adolescents.
Slide 19
Maternal and Child Health Care Measures
- Person-Centered Care:
- Children who had a doctor's office or clinic visit in the last 12 months who reported poor communication with health providers.
- Patient Safety:
- Birth trauma—injury to neonates.
- Care Coordination:
- Children and adolescents whose health provider usually asks about prescription medications and treatments from other doctors.
- Emergency department (ED) visits with a principal diagnosis related to mental health, alcohol, or substance abuse.
- ED visits for asthma.
Slide 20
Access: Children and Adolescents With Periods of Uninsurance
- Coverage gaps ("uninsurance") are a significant factor in children's access to and use of care, as well as their health outcomes.1-3
- Resources through the Children's Health Insurance Program Reauthorization Act (CHIPRA) are designed to increase Medicaid/CHIP enrollment:
- Outreach programs.
- Simplified enrollment strategies.4
- Coverage gaps are still found for as many as 40% of new CHIP enrollees5 despite changes in State enrollment, renewal, and outreach processes.
Slide 21
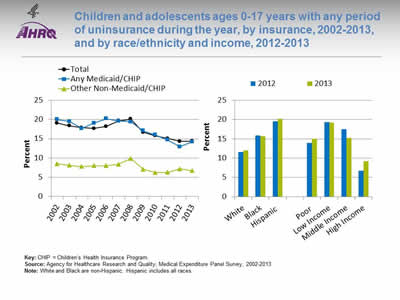
Children and adolescents ages 0-17 years with any period of uninsurance during the year, by insurance, 2002-2013, and by race/ethnicity and income, 2012-2013
Image: Charts show children and adolescents ages 0-17 years with any period of uninsurance during the year, by insurance and by race/ethnicity and income:
Left Chart:
| Year | Total | Other Non-Medicaid/CHIP | Any Medicaid/CHIP |
|---|---|---|---|
| 2002 | 19.1 | 8.5 | 20 |
| 2003 | 18.4 | 8.1 | 19.5 |
| 2004 | 17.9 | 7.8 | 17.7 |
| 2005 | 17.7 | 8 | 19.1 |
| 2006 | 18.2 | 8 | 20.2 |
| 2007 | 19.7 | 8.4 | 19.6 |
| 2008 | 20.1 | 9.9 | 19.4 |
| 2009 | 16.7 | 7.1 | 17.1 |
| 2010 | 15.8 | 6.2 | 16 |
| 2011 | 15.1 | 6.3 | 14.7 |
| 2012 | 14.3 | 7.2 | 12.9 |
| 2013 | 14.4 | 6.7 | 14.2 |
Right Chart:
| Characteristics | 2012 | 2013 |
|---|---|---|
| White | 11.6 | 12 |
| Black | 15.9 | 15.7 |
| Hispanic | 19.6 | 20.2 |
| Poor | 13.9 | 15 |
| Low Income | 19.3 | 19.2 |
| Middle Income | 17.5 | 15.3 |
| High Income | 6.7 | 9.2 |
Key: CHIP = Children's Health Insurance Program.
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Overall: In 2013, the percentage of children and adolescents ages 0-17 with any period of uninsurance during the year was 14.4%.
- Trends:
- The overall percentage of children and adolescents ages 0-17 years with any period of uninsurance during the year declined from 19.1% in 2002 to 14.4% in 2013.
- Among children and adolescents with any Medicaid or CHIP insurance, the percentage with any period of uninsurance during the year declined from 20.0% in 2002 to 14.2% in 2013.
- Groups With Disparities:
- In 2012 and 2013, White children were less likely to have a period of uninsurance than Black and Hispanic children.
- In 2012 and 2013, children in families with high incomes were less likely than children in every other income category to have a period of uninsurance.
Slide 22
Effectiveness Measures
- Early and adequate prenatal care.
- Receipt of recommended immunizations by young children.
- Children's vision screening.
- Well-child visits in the last year.
- Receipt of meningococcal vaccine by adolescents.
- Receipt of human papillomavirus (HPV) vaccination by adolescents.
Slide 23
Prevention: Early and Adequate Prenatal Care
- A Healthy People 2020 objective is for 77.6% of pregnant women to receive early and adequate prenatal care:
- Definition is based on Adequacy of Prenatal Care Utilization Index.
- For a given pregnancy, the target number of prenatal visits considered adequate is determined by the start date of prenatal care and the infant's gestational age at birth.
Slide 24
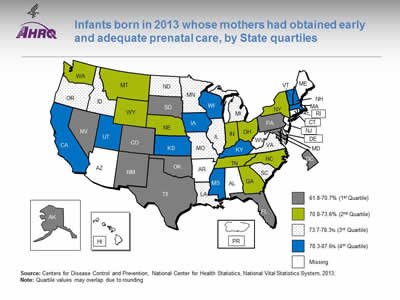
Infants born in 2013 whose mothers had obtained early and adequate prenatal care, by State quartiles
Image: Map of the United States is color-coded by state to show overall rankings by quartile of infants born to women who received early and adequate prenatal care.
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 2013.
Notes: Quartile values may overlap due to rounding.
Because of changes between the 1998 and 2003 versions of birth certificates, prenatal care timing and adequacy were evaluated only for the District of Columbia and the 41 States using the 2003 standard birth certificate for all of 2013. Data for 2013 were only available for these 42 State-equivalent jurisdictions, so national estimates were not generated. However, these 42 jurisdictions accounted for more than 86% of live births in the United States in 2013. The State-equivalent jurisdictions (AL, AR, AZ, CT, HI, ME, NJ, PR, RI, and WV) not using the 2003 version of the birth certificate did not have data available for this measure and are categorized as "missing" on the map.
To classify the adequacy of prenatal care services, the reported number of visits is compared with the expected number of visits for the period between when care began and the delivery date. Completeness of reporting varies by item and State. In 2013, two States were missing responses on more than 10% of the birth certificates (GA-15.9%; NV-12.9%). The impact of the comparatively high level of unknown data is not clear. Comparisons including information from these States should be made with caution. More detailed information is available in the 2013 Natality Data Users Guide: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/natality/UserGuide2013.pdf (1.4 MB).
- Overall: This map shows overall rankings by quartile in the percentage of infants born to women who received early and adequate prenatal care in 2013, for Washington, DC, and 41 States. Values ranged from 61.8% to 87.6%.
- Differences by State: Interquartile ranges follow:
- First quartile (lowest): 61.8%-70.7% (AK, CO, DC, FL, MD, NM, NV, OK, PA, SD, TX).
- Second quartile (second lowest): 70.8%-73.6% (GA, IN, MT, NE, NY, NC, OH, TN, WA, WY).
- Third quartile (second highest): 73.7%-78.3% (DE, ID, IL, LA, MI, MN, MO, ND, OR, SC, VA).
- Fourth quartile (highest): 78.3%-87.6 % (CA, IA, KS, KY, MA, MS, NH, UT, VT, WI).
Slide 25
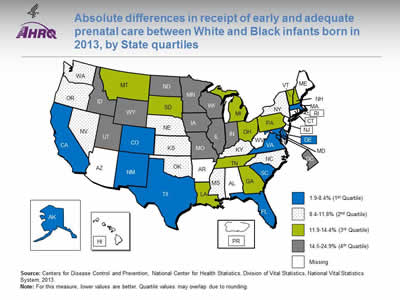
Absolute differences in receipt of early and adequate prenatal care between White and Black infants born in 2013, by State quartiles
Image: Map of the United States is color-coded by state to show rankings by quartile for the absolute differences between percentages of White and Black infants whose mothers received early and adequate prenatal care.
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Vital Statistics, National Vital Statistics System, 2013.
Notes: For this measure, lower values are better. Quartile values may overlap due to rounding.
Because of changes between the 1998 and 2003 versions of birth certificates, prenatal care timing and adequacy were evaluated only for the District of Columbia and the 41 States using the 2003 standard birth certificate for all of 2013. Data for 2013 were only available for these 42 State-equivalent jurisdictions, so national estimates were not generated. However, these 42 jurisdictions accounted for more than 86% of live births in the United States in 2013. The State-equivalent jurisdictions (AL, AR, AZ, CT, HI, ME, NJ, PR, RI, and WV) not using the 2003 version of the birth certificate did not have data available for this measure and are categorized as "missing" on the map.
To classify the adequacy of prenatal care services, the reported number of visits is compared with the expected number of visits for the period between when care began and the delivery date. Completeness of reporting varies by item and State. In 2013, two States were missing responses on more than 10% of the birth certificates (GA-15.9%; NV-12.9%). The impact of the comparatively high level of unknown data is not clear. Comparisons including information from these States should be made with caution. More detailed information is available in the 2013 Natality Data Users Guide: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/natality/UserGuide2013.pdf (1.4 MB).
- Overall: This map shows overall State-equivalent rankings by quartile for the absolute differences between percentages of White and Black infants born in 2013 whose mothers obtained early and adequate prenatal care. Differences ranged from 1.9% to 24.9% (lower is better).
- Differences by State: Interquartile ranges follow:
- First quartile (smallest absolute difference): 1.9%-8.4% (AK, CA, CO, DE, FL, MA, MD, NM, SC, TX, VA).
- Second quartile: 8.4%-11.8 (KS, KY, MS, NE, NV, NY, NC, OK, OR, WA).
- Third quartile: 11.9%-14.4% (GA, LA, MI, MT, NH, OH, PA, SD, TN, VT).
- Fourth quartile (largest absolute difference): 14.5%-24.9% (DC, ID, IL, IN, IA, MN, MO, ND, UT, WI, WY).
Slide 26

Prevention: Receipt of Recommended Vaccinations by Young Children
- Immunizations reduce mortality and morbidity by:
- Protecting recipients from illness.
- Protecting others in the community who are not vaccinated.
- Beginning in 2007, seven vaccines were recommended to be completed by ages 19-35 months. The recommended vaccines are:
- Diphtheria-tetanus-pertussis vaccine.
- Polio vaccine.
- Measles-mumps-rubella vaccine.
- Haemophilus influenzae type B vaccine.
- Hepatitis B vaccine.
- Varicella vaccine.
- Pneumococcal conjugate vaccine.
- The Healthy People 2020 target is 80% coverage in the population ages 19-35 months.
Note:
- These vaccines constitute the 4:3:1:3:3:1:4 vaccine series tracked in Healthy People 2020.
Slide 27
Prevention: Receipt of Recommended Vaccinations by Young Children
The U.S. Surgeon General, Dr. Vivek H. Murthy, and Elmo want everyone to stay healthy and get vaccinated! https://youtu.be/viS1ps0r4K0
Slide 28
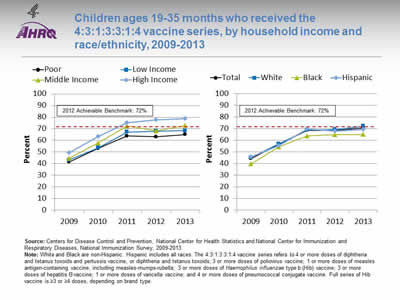
Children ages 19-35 months who received the 4:3:1:3:3:1:4 vaccine series, by household income and race/ethnicity, 2009-2013
Image: Charts show children ages 19-35 months who received the 4:3:1:3:3:1:4 vaccine series, by household income and race/ethnicity:
Left Chart:
| Income | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Poor | 41.6 | 53.1 | 63.9 | 63.1 | 65.0 |
| Low Income | 43.1 | 53.7 | 67.2 | 68.0 | 68.5 |
| Middle Income | 44.6 | 57.8 | 72.4 | 68.1 | 72.7 |
| High Income | 49.3 | 63.5 | 75.2 | 77.7 | 78.9 |
Right Chart:
| Race / Ethnicity | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|
| Total | 44.3 | 56.6 | 68.5 | 68.4 | 70.4 |
| Hispanic | 45.9 | 55.5 | 69.5 | 67.8 | 69.3 |
| Black | 39.6 | 54.5 | 63.7 | 64.8 | 65.0 |
| White | 45.2 | 56.9 | 68.8 | 69.3 | 72.1 |
2012 Achievable Benchmark: 72%.
Source: Centers for Disease Control and Prevention, National Center for Health Statistics and National Center for Immunization and Respiratory Diseases, National Immunization Survey, 2009-2013.
Notes: White and Black are non-Hispanic. Hispanic includes all races. The 4:3:1:3:3:1:4 vaccine series refers to 4 or more doses of diphtheria and tetanus toxoids and pertussis vaccine, or diphtheria and tetanus toxoids; 3 or more doses of poliovirus vaccine; 1 or more doses of measles antigen-containing vaccine, including measles-mumps-rubella; 3 or more doses of Haemophilus influenzae type b (Hib) vaccine; 3 or more doses of hepatitis B vaccine; 1 or more doses of varicella vaccine; and 4 or more doses of pneumococcal conjugate vaccine. Full series of Hib vaccine is ≥3 or ≥4 doses, depending on brand type.
- Overall: in 2013, the percentage of children ages 19-35 months who received the 4:3:1:3:3:1:4 vaccination series was 70.4%.
- Trends: From 2009 to 2013, the percentage of children ages 19-35 months who received the 4:3:1:3:3:1:4 vaccination series improved overall and for all income and racial/ethnic groups.
- Groups With Disparities:
- In 2013, the percentage of children ages 19-35 months who received all the recommended vaccines was lower for children from poor, low and middle income families compared to those from high income families.
- In 2013, the percentage of Black children (65.0%) ages 19-35 who received all the recommended vaccines was lower compared to White children (72.1%).
- Achievable Benchmark:
- The 2012 top 5 State achievable benchmark was 72%. The top 5 States that contributed to the achievable benchmark are Louisiana, Maryland, Massachusetts, New Hampshire, and Ohio.
- Children from high-income households and middle-income households have achieved the benchmark. White children also have achieved the benchmark.
- Children overall and children from poor and low-income households could achieve the benchmark in approximately a year. Black and Hispanic children also could achieve the benchmark within a year.
Slide 29
Prevention: Children's Vision Screening
- Vision checks for children may detect problems of which children and their parents were previously unaware.6
- Early detection also improves the chances that corrective treatments will be effective.6
Slide 30
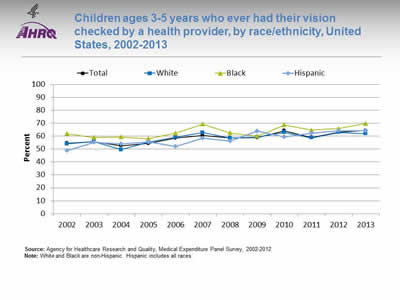
Children ages 3-5 years who ever had their vision checked by a health provider, by race/ethnicity, United States, 2002-2013
Image: Chart shows children ages 3-5 years who ever had their vision checked by a health provider, by race/ethnicity:
| Year | Total | White | Black | Hispanic |
|---|---|---|---|---|
| 2002 | 54.5 | 54.0 | 61.9 | 48.9 |
| 2003 | 55.8 | 55.6 | 59.0 | 55.4 |
| 2004 | 52.6 | 49.6 | 59.3 | 54.0 |
| 2005 | 54.4 | 55.4 | 58.1 | 55.7 |
| 2006 | 58.5 | 59.2 | 62.4 | 52.2 |
| 2007 | 60.5 | 62.8 | 69.3 | 58.5 |
| 2008 | 58.8 | 58.6 | 62.6 | 56.1 |
| 2009 | 58.9 | 59.2 | 60.1 | 64.1 |
| 2010 | 64.2 | 62.9 | 68.7 | 59.6 |
| 2011 | 59.1 | 58.8 | 64.7 | 62.3 |
| 2012 | 63.0 | 62.9 | 66.0 | 64.2 |
| 2013 | 64.4 | 61.9 | 69.8 | 64.2 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2012.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Trends:
- From 2002 to 2013, the percentage of children ages 3-5 years who had ever received a vision check by a health provider increased from 54.5% to 64.4%.
- Among White children ages 3-5 years, the percentage who had ever received a vision check by a health provider increased from 54% in 2002 to 61.9% in 2013. The percentage also increased for Hispanic children from 48.9% in 2002 to 64.2% in 2013. However, there was no statistically significant increase for Black children (61.9% in 2002 and 69.8% in 2013).
- Groups With Disparities:
- In 2013, there were no statistically significant differences between White, Black, and Hispanic children in the percentage who had ever received a vision check (61.9%, 69.8%, and 64.2%, respectively).
Slide 31
Prevention: Well-Child Visits in the Last Year
- The American Academy of Pediatrics recommends annual preventive health care visits for all children.7 Current (2014) recommendations for visits:
- 7 well-child visits before 12 months of age.
- 6 well-child visits between 12 and 36 months of age.
- 1 well-child visit per year from ages 3 to 21 years.
- The Affordable Care Act requires insurance plans to cover well-child visits with no copayments or deductibles.8
- A Healthy People 2020 objective is to improve the rate of adolescent well visits.9
Slide 32
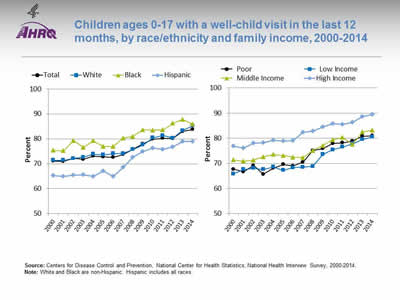
Children ages 0-17 with a well-child visit in the last 12 months, by race/ethnicity and family income, 2000-2014
Image: Charts show children ages 0-17 with a well-child visit in the last 12 months, by race/ethnicity and family income:
Left Chart:
| Year | Total | White | Black | Hispanic |
|---|---|---|---|---|
| 2000 | 71.0 | 71.3 | 75.4 | 65.3 |
| 2001 | 71.0 | 71.4 | 75.2 | 64.9 |
| 2002 | 72.1 | 72.1 | 79.4 | 65.4 |
| 2003 | 71.8 | 72.7 | 76.5 | 65.6 |
| 2004 | 73.0 | 73.9 | 79.2 | 64.9 |
| 2005 | 72.8 | 73.6 | 77.0 | 67.1 |
| 2006 | 72.5 | 74.0 | 76.9 | 64.9 |
| 2007 | 73.7 | 74.1 | 80.3 | 68.5 |
| 2008 | 75.8 | 75.7 | 81.0 | 72.6 |
| 2009 | 78.0 | 77.6 | 83.6 | 74.9 |
| 2010 | 79.9 | 80.4 | 83.5 | 76.3 |
| 2011 | 80.3 | 81.3 | 83.6 | 75.8 |
| 2012 | 80.2 | 80.3 | 86.3 | 76.8 |
| 2013 | 83.0 | 83.3 | 87.8 | 79.0 |
| 2014 | 83.8 | 85.3 | 85.9 | 78.9 |
Right Chart:
| Year | Poor | Low Income | Middle Income | High Income |
|---|---|---|---|---|
| 2000 | 67.7 | 65.8 | 71.3 | 76.8 |
| 2001 | 66.6 | 67.5 | 70.9 | 76.1 |
| 2002 | 69.1 | 68.1 | 71.3 | 78.0 |
| 2003 | 65.7 | 67.5 | 72.6 | 78.2 |
| 2004 | 68.1 | 68.5 | 73.5 | 79.1 |
| 2005 | 69.5 | 67.3 | 73.1 | 78.8 |
| 2006 | 69.0 | 68.3 | 72.4 | 79.1 |
| 2007 | 70.5 | 68.5 | 72.2 | 82.4 |
| 2008 | 75.1 | 68.8 | 75.1 | 82.8 |
| 2009 | 75.8 | 73.5 | 77.1 | 84.5 |
| 2010 | 77.9 | 75.4 | 79.4 | 85.8 |
| 2011 | 78.2 | 76.5 | 80.3 | 85.5 |
| 2012 | 78.9 | 77.9 | 77.6 | 86.3 |
| 2013 | 80.8 | 79.5 | 82.5 | 88.6 |
| 2014 | 81 | 80.5 | 83.2 | 89.5 |
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey, 2000-2014.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Trends:
- Overall, the percentage of children ages 0-17 years who had a well-child visit (as distinct from a symptom-driven visit) in the last 12 months increased from 71% in 2000 to 83.8% in 2014.
- From 2000 to 2014, the percentage of children who had a well-child visit increased significantly for Whites (71.3% to 85.3%), Blacks (75.4% to 85.9%), and Hispanics (65.3% to 78.9%).
- The percentage of children who had a well-child visit also increased for all income groups. From 2000 to 2014, the percentage of children with a well-child visit increased from 67.7% to 81.0% for poor families; from 65.8% to 80.5% for low-income families; rom 71.3% to 83.2% for middle-income families; and from 76.8% to 89.5% for high-income families.
- Groups With Disparities:
- In 2014, White children were more likely than Hispanic children to have had at least one well-child visit during the year (85.3% vs. 78.9%).
- In 2014, children in high-income families were more likely than children in poor, low-income, and middle-income families to have had at least one well-child visit during the year (89.5% vs. 81.0%, 80.5%, and 83.2%, respectively).
Slide 33
Prevention: Adolescent Meningitis Vaccine
- In 2010, children ages 10-14 years made up 6.7% of the U.S. population, and teens ages 15-19 made up 7.1%.10
- Youth ages 10-19 years are at risk of contracting meningitis, a possibly fatal11 infection.
- Meningococcal diseases are infections caused by the bacteria Neisseria meningitidis.12 Neisseria meningitides causes various infections but is most important as a potential cause of meningitis.12 It can also cause meningococcemia, a bloodstream infection.12
- The meningococcal vaccine can prevent most types of meningococcal disease.13 The meningococcal vaccine is recommended for all children ages 11-12 years. Effective January 2011, a second dose is recommended at age 16.13
Slide 34
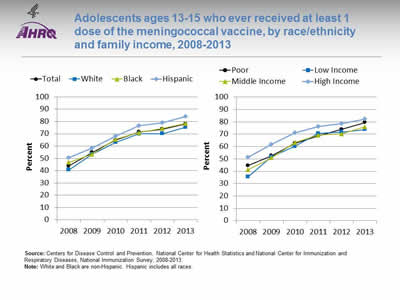
Adolescents ages 13-15 who ever received at least 1 dose of the meningococcal vaccine, by race/ethnicity and family income, 2008-2013
Image: Charts show adolescents ages 13-15 who ever received at least 1 dose of the meningococcal vaccine, by race/ethnicity and family income:
Left Chart:
| Race / Ethnicity | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|
| Total | 43.9 | 54.8 | 64.8 | 71.5 | 73.8 | 78.1 |
| Hispanic | 50.6 | 58.5 | 68.2 | 76.6 | 79.0 | 84.0 |
| Black | 46.7 | 53.4 | 65.5 | 71.0 | 74.3 | 78.4 |
| White | 40.7 | 53.4 | 63.0 | 69.9 | 70.1 | 75.3 |
Right Chart:
| Income | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|
| Poor | 44.7 | 52.6 | 62.6 | 68.5 | 74.0 | 79.5 |
| Low Income | 35.6 | 51.7 | 60.1 | 70.5 | 71.7 | 73.7 |
| Middle Income | 41.3 | 50.9 | 63.1 | 69.2 | 70.2 | 75.9 |
| High Income | 51.3 | 61.8 | 71.2 | 76.3 | 78.6 | 82.2 |
Source: Centers for Disease Control and Prevention, National Center for Health Statistics and National Center for Immunization and Respiratory Diseases, National Immunization Survey, 2008-2013.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Overall: In 2013, the percentage of adolescents ages 13-15 who ever received at least 1 dose of the meningococcal vaccine was 78.1%.
- Trends: The percentage of adolescents ages 13-15 who ever received at least 1 dose of the meningococcal vaccine improved overall and for all racial/ethnic groups and income groups.
- Groups With Disparities:
- In 2013, the percentage of Hispanic adolescents (84%) ages 13-15 who ever received at least 1 dose of meningococcal vaccine was higher compared with White adolescents (75.3%).
- In all years, the percentage of adolescents ages 13-15 who ever received at least 1 dose of meningococcal vaccine was lower for those who live in poor, low-, and middle-income households compared with those from high-income households.
Slide 35
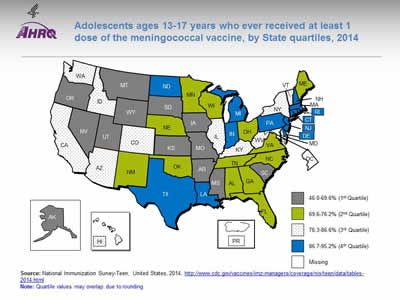
Adolescents ages 13-17 years who ever received at least 1 dose of the meningococcal vaccine, by State quartiles, 2014
Image: Map of the United States is color-coded by state to show estimated vaccination coverage with at least 1 dose of meningococcal vaccine among adolescents.
Source: National Immunization Survey-Teen, United States, 2014. http://www.cdc.gov/vaccines/imz-managers/coverage/nis/teen/data/tables-2014.html
Notes: Quartile values may overlap due to rounding.
- Overall: This map shows estimated vaccination coverage with at least 1 dose of meningococcal vaccine among adolescents ages 13-17 years, by State. State values ranged from 46.0% (Mississippi) to 95.2% (Pennsylvania).
- Differences by State: Interquartile ranges follow:
- First quartile (lowest): 46.0%-69.6% (AK, AR, IA, KS, MO, MS, MT, NV, OR, SC, SD, UT, WY).
- Second quartile (second lowest): 69.6%-76.2% (AL, FL, GA ME, MN, NC, NE, NM, OH, OK, TN, VA, WI).
- Third quartile (second highest): 76.3%-86.6% (AZ, CA, CO, HI, ID, IL, KY, MD, NY, VT, WA, WV).
- Fourth quartile (highest): 86.7%-95.2% (CT, DE, IN, LA, MA, MI, ND, NH, NJ, PA, RI, TX).
Slide 36
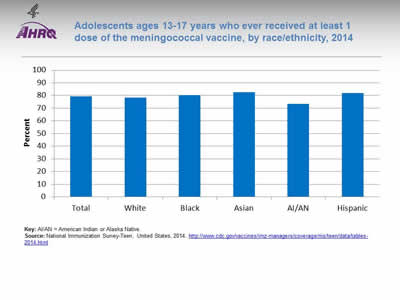
Adolescents ages 13-17 years who ever received at least 1 dose of the meningococcal vaccine, by race/ethnicity, 2014
Image: Chart shows adolescents ages 13-17 years who ever received at least 1 dose of the meningococcal vaccine, by race/ethnicity:
- Total - 79.3.
- White - 78.2.
- Black - 80.3.
- Asian - 82.5.
- AI/AN - 73.5.
- Hispanic - 82.1.
Key: AI/AN = American Indian or Alaska Native.
Source: National Immunization Survey-Teen, United States, 2014. http://www.cdc.gov/vaccines/imz-managers/coverage/nis/teen/data/tables-2014.html
Notes:
- Overall Rate: In 2014, the estimated vaccination coverage for the meningitis vaccine among all adolescents ages 13-17 was 79.3%.
- Groups With Disparities:
- Hispanics (82.1%) and Asians (82.5%) had the highest coverage.
- American Indians and Alaska Natives (73.5%) had the lowest coverage.
Slide 37
Human Papillomavirus Vaccination Coverage for Adolescents
- Licensed HPV vaccine available since 2006.
- Recommended by the Advisory Committee on Immunization Practices (ACIP) for routine vaccination of girls at age 11 or 12.14,15
- Quadrivalent HPV (HPV4) recommended by ACIP in 2011 for routine vaccination of boys at age 11 or 12.16
- Can be safely given with other routine vaccines; administration of all age-appropriate vaccines during a single visit recommended by ACIP.17
Slide 38
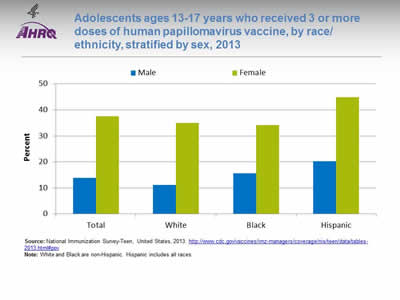
Adolescents ages 13-17 years who received 3 or more doses of human papillomavirus vaccine, by race/ethnicity, stratified by sex, 2013
Image: Chart shows adolescents ages 13-17 years who received 3 or more doses of human papillomavirus vaccine, by race/ethnicity, stratified by sex:
| Race / Ethnicity | Male | Female |
|---|---|---|
| Total | 13.9 | 37.6 |
| White | 11.1 | 34.9 |
| Black | 15.7 | 34.2 |
| Hispanic | 20.3 | 44.8 |
Source: National Immunization Survey-Teen, United States, 2013. http://www.cdc.gov/vaccines/imz-managers/coverage/nis/teen/data/tables-2013.html#pov.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Overall Rate: In 2013, 37.6% of adolescent females and 13.9% of adolescent males ages 13-17 years received 3 or more doses of the human papillomavirus (HPV) vaccine.
- Groups With Disparities:
- Hispanic females ages 13-17 (44.8%) were more likely than both White (34.9%) and Black (34.2%) females ages 13-17 to have received 3 or more doses of the HPV vaccine. There were no statistically significant differences between White females and Black females.
- Both Black (15.7%) and Hispanic (20.3%) males ages 13-17 were more likely than White (11.1%) males ages 13-17 to have received 3 or more doses of the HPV vaccine. There were no statistically significant differences between White males and Black males.
Slide 39
Person-Centered Care
- Person-centered care has taken an important place in quality measurement and improvement in the United States and elsewhere.18-21
- Good communication and demonstrations of respect are two critical aspects of person-centered care.22,23
Slide 40
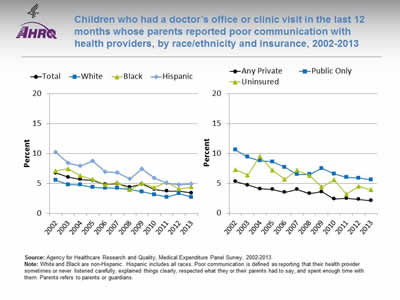
Children who had a doctor's office or clinic visit in the last 12 months whose parents reported poor communication with health providers, by race/ethnicity and insurance, 2002-2013
Image: Charts show children who had a doctor's office or clinic visit in the last 12 months whose parents reported poor communication with health providers, by race/ethnicity and insurance:
Left Chart:
| Race / Ethnicity | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 6.7 | 6.1 | 5.7 | 5.5 | 4.8 | 4.9 | 4.4 | 4.9 | 4.0 | 3.8 | 3.7 | 3.4 |
| White | 5.6 | 4.8 | 4.8 | 4.4 | 4.2 | 4.2 | 4.0 | 3.6 | 3.1 | 2.7 | 3.3 | 2.7 |
| Black | 7.1 | 7.5 | 6.3 | 5.7 | 4.8 | 5.1 | 4.0 | 5.1 | 4.3 | 5.2 | 4.1 | 4.4 |
| Hispanic | 10.2 | 8.4 | 7.9 | 8.8 | 7.0 | 6.8 | 5.8 | 7.4 | 5.9 | 5.1 | 4.8 | 4.9 |
Right Chart:
| Year | Any Private | Public Only | Uninsured |
|---|---|---|---|
| 2002 | 5.3 | 10.6 | 7.3 |
| 2003 | 4.7 | 9.4 | 6.4 |
| 2004 | 4.1 | 8.8 | 9.5 |
| 2005 | 4 | 8.6 | 7.2 |
| 2006 | 3.5 | 7.7 | 5.7 |
| 2007 | 4 | 6.5 | 7.2 |
| 2008 | 3.3 | 6.5 | 6.3 |
| 2009 | 3.6 | 7.5 | 4.4 |
| 2010 | 2.4 | 6.6 | 5.6 |
| 2011 | 2.5 | 6 | 3.2 |
| 2012 | 2.3 | 5.9 | 4.5 |
| 2013 | 2.1 | 5.6 | 3.9 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
Notes: White and Black are non-Hispanic. Hispanic includes all races. Poor communication is defined as reporting that their health provider sometimes or never listened carefully, explained things clearly, respected what they or their parents had to say, and spent enough time with them. Parents refers to parents or guardians.
- Overall Rate: In 2013, 3.4% of parents reported poor communication with their children's health provider.
- Trends:
- From 2002 to 2013, the percentage of children whose parents reported poor communication with their health providers decreased from 6.7% to 3.4%.
- Between 2002 and 2013, the percentage of children whose parents reported poor communication decreased for all racial/ethnic and insurance groups.
- Groups With Disparities:
- In 2013, the percentage reporting poor communication with health providers was higher for Hispanic children (4.9%) and Black (4.4%) children compared with White children (2.7%).
- In 2013, 2.1% of parents of privately insured children reported poor communication compared with 5.6% of parents of publicly insured children.
Slide 41
Patient Safety: Birth Trauma
- Cases included in birth trauma measure:
- Hemorrhage below the scalp.
- Cerebral hemorrhage at birth.
- Spinal cord injury at birth.
- Facial nerve injury at birth.
- Bone injury not elsewhere classified at birth.
- Nerve injury not elsewhere classified at birth.
- Birth trauma not elsewhere classified.24
- Many of these injuries to neonates may be preventable.25
Slide 42
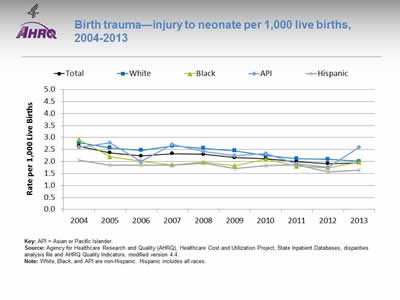
Birth trauma—injury to neonate per 1,000 live births, 2004-2013
Image: Chart shows birth trauma—injury to neonate per 1,000 live births:
| Year | Total | White | Black | API | Hispanic |
|---|---|---|---|---|---|
| 2004 | 2.64 | 2.79 | 2.92 | 2.59 | 2.05 |
| 2005 | 2.36 | 2.57 | 2.20 | 2.79 | 1.85 |
| 2006 | 2.23 | 2.47 | 2.01 | 2.01 | 1.85 |
| 2007 | 2.33 | 2.65 | 1.86 | 2.71 | 1.84 |
| 2008 | 2.30 | 2.55 | 1.97 | 2.41 | 1.94 |
| 2009 | 2.16 | 2.45 | 1.82 | 2.24 | 1.70 |
| 2010 | 2.12 | 2.25 | 2.09 | 2.34 | 1.82 |
| 2011 | 2.00 | 2.12 | 1.80 | 1.89 | 1.87 |
| 2012 | 1.91 | 2.09 | 1.74 | 1.76 | 1.56 |
| 2013 | 1.93 | 2.00 | 1.97 | 2.60 | 1.64 |
Key: API = Asian or Pacific Islander.
Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project, State Inpatient Databases, disparities analysis file and AHRQ Quality Indicators, modified version 4.4.
Notes: White, Black, and API are non-Hispanic. Hispanic includes all races.
- Overall Rate: In 2013, the birth trauma-neonatal injury rate was 1.9 per 1,000 live births.
- Trends:
- Birth trauma-neonatal injury rates fell from 2.6 per 1,000 live births in 2004 to 1.9 per 1,000 live births in 2013.
- Between 2004 and 2013, birth trauma-neonatal injury rates fell for all racial/ethnic groups, except for Asians and Pacific Islanders (APIs).
- Groups With Disparities:
- In 2013, Hispanic neonates (1.6 per 1,000 live births) were less likely to experience birth trauma compared with White neonates (2.0 per 1,000 live births).
Slide 43
Care Coordination Measures
- Children and adolescents whose health provider usually asks about prescription medications and treatments from other doctors.
- Emergency department (ED) visits with a principal diagnosis related to mental health, alcohol, or substance abuse.
- ED visits for asthma.
Slide 44
Communication About Prescription Medications and Treatments From Other Doctors
- Children are at risk for medication errors, including those due to polypharmacy, for various reasons26:
- Their size and physiologic variability.
- Limited communication ability and other factors.26
- Good medical practice includes asking patients about all their medications which can prevent adverse events.27
- The Food and Drug Administration and others urge patients to tell health care providers about all their medications.28
- Health care systems are trying strategies to better communicate with patients about medications other health care professionals give them.29
Slide 45
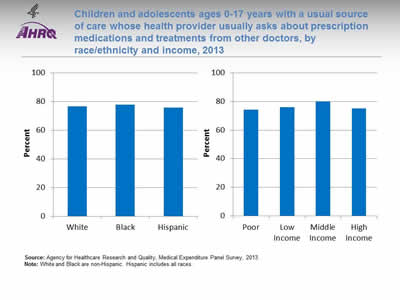
Children and adolescents ages 0-17 years with a usual source of care whose health provider usually asks about prescription medications and treatments from other doctors, by race/ethnicity and income, 2013
Image: Charts show children and adolescents with a usual source of care whose health provider usually asks about prescription medications and treatments from other doctors, by race/ethnicity and income:
Left Chart:
- White - 76.6.
- Black - 77.8.
- Hispanic - 75.9.
Right Chart:
- Poor - 74.3.
- Low Income - 76.1.
- Middle Income - 80.
- High Income - 75.2.
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2013.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Trends: From 2002 to 2013, the percentage of children and adolescents whose health provider usually asked about medications and treatments from other doctors increased significantly, from 71.1% to 76.6% (data not shown).
- Groups With Disparities:
- In 2013, there were no statistically significant differences between Whites (76.6%), Blacks (77.8%), and Hispanics (75.9%) in the percentage of children whose health provider asked about medications and treatments from other doctors.
- In 2013, there were no statistically significant differences by income:
- Poor, 74.3%.
- Low income, 76.1%.
- Middle income, 80.0%.
- High income, 75.2%.
Slide 46
Emergency Department Visits Related to Mental Health and Substance Abuse
- EDs are a common source of care for mental illness when high-quality mental health care is not available in the community.30
- Some ED use for mental health and substance abuse problems among young people is seen as preventable with appropriate ambulatory care.
- Mental, emotional, and behavioral health services are lacking for as many as 50% of children and adolescents with high needs.31
Slide 47
Emergency Department Visits Related to Mental Health and Substance Abuse
- EDs are often not staffed or equipped to provide optimal psychiatric care, leading to long wait times for appropriate care.32
- ED staff observing patients waiting for psychiatric care find it difficult to efficiently care for patients with other medical emergencies.33
- Efforts are underway to prevent avoidable ED use through strategies such as case management.34,35
Slide 48
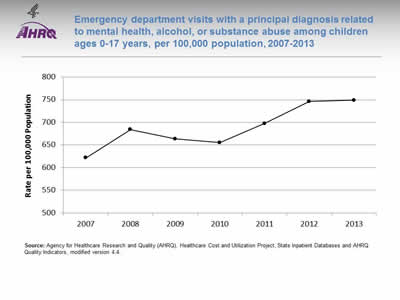
Emergency department visits with a principal diagnosis related to mental health, alcohol, or substance abuse among children ages 0-17 years, per 100,000 population, 2007-2013
Image: Chart shows emergency department visits with a principal diagnosis related to mental health, alcohol, or substance abuse among children ages 0-17 years:
| Year | Rate per 100,000 Population |
|---|---|
| 2007 | 621.8 |
| 2008 | 684 |
| 2009 | 663.3 |
| 2010 | 655.3 |
| 2011 | 697.5 |
| 2012 | 746 |
| 2013 | 749 |
Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project, State Inpatient Databases and AHRQ Quality Indicators, modified version 4.4.
Notes:
- Overall Rate: In 2013, among children ages 0-17 years, there were 749 ED visits related to mental health, alcohol, or substance use per 100,000 population.
- Trends: ED visit rates for children related to mental health, alcohol, or substance use worsened between 2007 (621.8 per 100,000 population) and 2013 (749 per 100,000 population).
Slide 49
Emergency Department Visits for Asthma
- Asthma is a common chronic disease among children.36
- ED visits for asthma are often preventable if a child receives high-quality ambulatory care.
- Three strategies are most likely to improve provider adherence to guidelines for asthma care:
- Decision support tools.
- Feedback and audit.
- Clinical pharmacy support.37
Slide 50
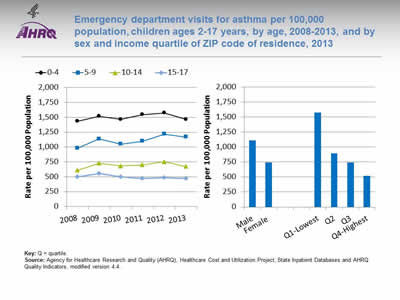
Emergency department visits for asthma per 100,000 population, children ages 2-17 years, by age, 2008-2013, and by sex and income quartile of ZIP code of residence, 2013
Image: Charts show emergency department visits for asthma per 100,000 population, children ages 2-17 years, by age, and by sex and income quartile of ZIP code of residence:
Left Chart:
| Year | 0-4 | 5-9 | 10-14 | 15-17 |
|---|---|---|---|---|
| 2008 | 1432.9 | 978.4 | 609.7 | 496.8 |
| 2009 | 1517 | 1135.6 | 726.2 | 555.9 |
| 2010 | 1465.2 | 1050.1 | 681.4 | 497.7 |
| 2011 | 1545 | 1096.9 | 698.7 | 472.9 |
| 2012 | 1574.3 | 1218.3 | 752.9 | 483.6 |
| 2013 | 1464.4 | 1169.3 | 670 | 471 |
Right Chart:
- Male - 1110.7.
- Female 741.9.
- Q1-Lowest - 1568.7.
- Q2 - 889.8.
- Q3 - 743.8.
- Q4-Highest - 516.4.
Key: Q = quartile.
Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project, State Inpatient Databases and AHRQ Quality Indicators, modified version 4.4.
Notes:
- Overall Rate: In 2013, the overall rate of ED visits for asthma was 930 per 100,000 (data not shown).
- Trend: From 2008 to 2013, the rate of ED visits for asthma worsened for children ages 5-9 (from 978 per 100,000 population to 1,169 per 100,000).
- Groups With Disparities:
- In 2013, male children ages 2-17 were 1.5 times as likely as female children to experience an ED visit for asthma (1,111 per 100,000 population vs. 742 per 100,000).
- In 2013, the rate of asthma ED visits was lower for children in the highest income quartile (516 per 100,000 population) compared with children in the first (1,569 per 100,000 population), second (890 per 100,000 population), and third quartiles (744 per 100,000 population).
Slide 51
References
- Cassedy A, Fairbrother G, Newacheck P. The impact of insurance instability on children's access, utilization, and satisfaction with health care. Ambul Pediatr 2008 Sep-Oct;8(5):321-8. PMID: 18922506. http://www.sciencedirect.com/science/article/pii/S1530156708001172. Accessed March 22, 2016.
- Guevara J, Moon J, Hines E, et al. Continuity of public insurance coverage: a systematic review of the literature. Med Care Res Rev 2014;71(2):115-37. PMID: 24227811. http://mcr.sagepub.com/content/71/2/115.long. Accessed March 22, 2016.
- Kenney G, Pelletier J. Monitoring duration of coverage in Medicaid and CHIP to assess program performance and quality. Acad Pediatr 2011;May-Jun;11(3 Suppl):S34-41. http://www.sciencedirect.com/science/article/pii/S1876285910001257. Accessed March 22, 2016.
- Children's Health Insurance Program Reauthorization Act of 2009. Public Law 111-3. http://www.gpo.gov/fdsys/pkg/PLAW-111publ3/html/PLAW-111publ3.htm. Accessed May 15, 2015.
- Harrington M, Kenney GM, et al. 2014. CHIPRA mandated evaluation of the Children's Health Insurance Program: final findings. Report submitted to the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Ann Arbor, MI: Mathematica Policy Research; August 2014. http://www.medicaid.gov/chip/downloads/chip_report_congress-2014.pdf (1.032 MB). Accessed March 22, 2016.
- U.S. Preventive Services Task Force. Visual Impairment in Children Ages 1-5: Screening. January 2011. http://www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/visual-impairment-in-children-ages-1-5-screening. Accessed March 22, 2016.
- American Academy of Pediatrics. Recommendations for Preventive Pediatric Health Care. http://pediatriccare.solutions.aap.org/DocumentLibrary/Periodicity%20Schedule_FINAL.pdf (394.89 KB) Last updated 2014. Accessed March 22, 2016.
- U.S. Department of Health and Human Services. Preventive Care for Children. 26 Covered Preventive Services for Children.
- Adolescent Health. AH-1. Increase the proportion of adolescents who have had a wellness checkup in the past 12 months. http://www.healthypeople.gov/2020/topics-objectives/topic/Adolescent-Health. Accessed March 22, 2016.
Slide 52
References
- U.S. Census Bureau. Community facts: 2010 profile of general population and housing characteristics: 2010 demographic profile data. http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_DP_DPDP1. Accessed March 22, 2016.
- Centers for Disease Control and Prevention. Meningitis. http://www.cdc.gov/meningitis/index.html. Accessed March 22, 2016.
- Centers for Disease Control and Prevention. Meningococcal Disease. http://www.cdc.gov/meningococcal/index.html. Accessed March 22, 2016.
- Centers for Disease Control and Prevention. Meningococcal VIS. http://www.cdc.gov/vaccines/hcp/vis/vis-statements/mening.html. Accessed 05/18/2015.
- Markowitz LE, Dunne EF, Saraiya M, et al. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2007;56(RR02). http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5602a1.htm. Accessed March 22, 2016.
- FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). MMWR 2010 May 28;59(20):626-9. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5920a4.htm. Accessed March 22, 2016.
- Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR 2011 Dec 23;60(50):1705-8. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6050a3.htm?s_cid=mm6050a3_w. Accessed March 22, 2016.
- Kroger AT, Sumaya CV, Pickering LK, et al. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices. MMWR 2011;60(RR02). http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6002a1.htm?s_cid=rr6002a1_w. Accessed March 22, 2016.
- Iedema R, Angell B. What are patients' care experience priorities? BMJ Qual Saf 2015 Jun;24 (6):356-9. PMID: 25972222. http://qualitysafety.bmj.com/content/24/6/356.long. Accessed March 22, 2016.
- Basch E. New frontiers in patient-reported outcomes: adverse event reporting, comparative effectiveness, and quality assessment. Annu Rev Med 2014;65:307-17. PMID: 24274179. http://www.annualreviews.org/doi/abs/10.1146/annurev-med-010713-141500?url_ver=Z39.88-2003&rfr_dat=cr_pub%3Dpubmed&rfr_id=ori:rid:crossref.org&journalCode=med. Accessed March 22, 2016.
Slide 53
References
- American Academy of Pediatrics Committee on Hospital Care and Institute for Patient- and Family-Centered Care. Patient- and family-centered care and the pediatrician's role. Pediatrics 2012 Feb;129(2):394-404. Epub 2012 Jan 30. PMID: 22291118. http://pediatrics.aappublications.org/content/129/2/394.long. Accessed March 22, 2016.
- Bethell C. Engaging families (and ourselves) in quality improvement: an optimistic and developmental perspective. Acad Pediatr 2013 Nov-Dec;13(6 Suppl):S9-11. PMID: 24268092. http://www.sciencedirect.com/science/article/pii/S187628591300212X. Accessed March 22, 2016.
- Dudley N. Ackerman A, Brown KM, et al. American Academy of Pediatrics Committee on Pediatric Emergency Medicine; American College of Emergency Physicians Pediatric Emergency Medicine Committee; Emergency Nurses Association Pediatric Committee. Patient- and family-centered care of children in the emergency department. Pediatrics 2015 Jan;135(1):e255-72. PMID: 25548335. http://pediatrics.aappublications.org/content/135/1/e255.long. Accessed March 22, 2016.
- Phillips-Salimi C, Haase J, Kooken W. Connectedness in the context of patient-provider relationships: a concept analysis. J Adv Nurs 2012 Jan;68(1):230-45. Epub 2011 Jul 20. PMID: 21771040. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601779/. Accessed March 22, 2016.
- Agency for Healthcare Research and Quality. Birth Trauma Rate—Injury to Neonate: Technical Specifications. AHRQ Quality Indicators™, Version 5.0. Patient Safety Indicators 17. http://www.qualityindicators.ahrq.gov/Downloads/Modules/PSI/V50/TechSpecs/PSI_17_Birth%20Trauma%20RateInjury%20to%20Neonate.pdf (61.38 KB) Last update November 2014. Accessed March 22, 2016.
- Ramphul M, Kennelly MM, Burke G, et al. Risk factors and morbidity associated with suboptimal instrument placement at instrumental delivery: observational study nested within the Instrumental Delivery & Ultrasound randomised controlled trial ISRCTN 72230496. BJOG 2015 Mar;122(4):558-63. Epub 2014 Nov 21. PMID: 25414081. http://onlinelibrary.wiley.com/doi/10.1111/1471-0528.13186/full. Accessed March 22, 2016.
- Neuspiel D, Taylor M. Reducing the risk of harm from medication errors in children. Health Serv Insights 2013 Jun 30;6:47-59. PMID: 25114560. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4089677/. Accessed March 22, 2016.
- General Medical Council. Prescribing guidance: sharing information with colleagues. 2015. http://www.gmc-uk.org/guidance/ethical_guidance/14320.asp. Accessed March 22, 2016.
Slide 54
References
- Food and Drug Administration. Strategies to Reduce Medication Errors: Working to Improve Medication Safety. 2013. http://www.fda.gov/Drugs/ResourcesForYou/Consumers/ucm143553.htm. Accessed March 22, 2016.
- Sarzynski EM, Luz CC, Rios-Bedoya CF, et al. Considerations for using the "brown bag" strategy to reconcile medications during routine outpatient office visits. Qual Prim Care 2014;22(4):177-87. PMID: 25695529.
- Alakeson V, Frank T. Health care reform and mental health care delivery. Psychiatr Serv 2010 Nov;61(11):1063. PMID: 21041340. http://ps.psychiatryonline.org/doi/full/10.1176/ps.2010.61.11.1063. Accessed March 22, 2016.
- Simon AE, Pastor PN, Reuben CA, et al. Use of mental health services by children ages six to 11 with emotional or behavioral difficulties. Psychiatr Serv 2015 May 15:appips201400342. [Epub ahead of print]. PMID: 25975889.
- Institute of Medicine. Committee on the Future of Emergency Care in the United States Health System. Hospital-based emergency care: at the breaking point. Washington, DC: National Academies Press; 2007.
- Alakeson V, Pande N, Ludwig M. A plan to reduce emergency room "boarding" of psychiatric patients. Health Aff (Millwood) 2010 Sep;29(9):1637-42. PMID: 20820019. http://content.healthaffairs.org/content/29/9/1637.long. Accessed March 22, 2016.
- Kirk T, Di Leo P, Rehmer P, et al. A case and care management program to reduce use of acute care by clients with substance use disorders. Psychiatr Serv 2013 May;64(5):491-3. PMID: 23632578. http://ps.psychiatryonline.org/doi/full/10.1176/appi.ps.201200258. Accessed March 22, 2016.
- Olmstead T, Cohen J, Petry N. Health-care service utilization in substance abusers receiving contingency management and standard care treatments. Addiction 2012;107(8):1462-70. Epub 2012 Apr 17. PMID: 22296262. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3634865/. Accessed March 22, 2016.
- Akinbami LJ, Moorman JE, Simon AE, et al. Trends in racial disparities for asthma outcomes among children 0-17 years, 2001-2010. J Allergy Clin Immunol 2014 Sep;134(3):547-53. Epub 2014 Aug 1. PMID: 25091437. http://www.sciencedirect.com/science/article/pii/S0091674914007982#. Accessed March 22, 2016.
- Okelo S, Butz AM, Sharma R, et al. Interventions to modify health care provider adherence to asthma guidelines: a systematic review. Pediatrics 2013 Sep;132(3):517-34. Epub 2013 Aug 26. PMID: 23979092. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4079294/. Accessed March 22, 2016.
Slide 55
Chartbook on Healthy Living
Lifestyle Modification
Slide 56
Lifestyle Modification and Health
- Unhealthy behaviors place many Americans at risk for a variety of diseases.
- Lifestyle practices account for more than 40% of the differences in health among individuals.1
Slide 57
Impact of Behaviors on Health
- A recent study2 examined the effects of three healthy lifestyles on the risks of all-cause mortality and developing chronic conditions among adults in the United States:
- Not smoking.
- Engaging in at least 150 minutes of moderate or vigorous physical activity per week.
- Eating a healthy diet (e.g., grains, fruits, vegetables).
Slide 58
Impact of Behaviors on Health
- Compared with adults who did not engage in healthy behaviors, the risk for all-cause mortality was reduced by:
- 56% among nonsmokers.
- 47% among adults who were physically active.
- 26% among adults who consumed a healthy diet.2
- The risk of death decreased as the number of healthy behaviors increased. For adults engaged in all three healthy behaviors, the risk of death was reduced by:
- 82% for all causes.
- 65% for cardiovascular disease.
- 83% for cancer.
- 90% for other causes.2
Slide 59
Lifestyle Modification Measures
- Adult current smokers with a checkup in the last 12 months who received advice to quit smoking.
- Adults with obesity who ever received advice from a health professional to exercise more.
- Adults with obesity who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week.
Slide 60
Lifestyle Modification Measures
- Children ages 2-17 for whom a health provider gave advice about exercise.
- Adults with obesity who ever received advice from a health professional about eating fewer high-fat or high-cholesterol foods.
- Children ages 2-17 for whom a health provider gave advice within the past 2 years about healthy eating.
Slide 61
Prevention: Counseling To Quit Smoking
- Smoking harms nearly every bodily organ and causes or worsens many diseases.
- In the past 50 years, more than 20 million premature deaths have been attributable to smoking and exposure to secondhand smoke.3
- Smoking causes more than 87% of deaths from lung cancer and more than 79% of deaths from chronic obstructive pulmonary disease.3
Slide 62
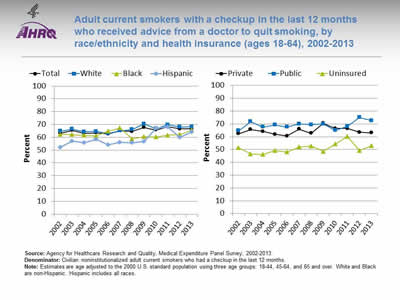
Adult current smokers with a checkup in the last 12 months who received advice from a doctor to quit smoking, by race/ethnicity and health insurance (ages 18-64), 2002-2013
Image: Charts show adult current smokers with a checkup in the last 12 months who received advice from a doctor to quit smoking, by race/ethnicity and health insurance:
Left Chart:
| Race / Ethnicity | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 63.1 | 65.3 | 63.1 | 63.4 | 62.7 | 65.1 | 64.5 | 67.6 | 65.7 | 68.2 | 66.5 | 66.5 |
| White | 64.8 | 66.4 | 64.2 | 64.6 | 63.0 | 65.0 | 66.1 | 70.5 | 66.7 | 69.8 | 67.9 | 68.1 |
| Black | 62.3 | 62.2 | 61.5 | 61.0 | 64.8 | 67.3 | 58.7 | 60.5 | 60.1 | 61.7 | 62.1 | 65.8 |
| Hispanic | 52.0 | 57.2 | 55.7 | 58.5 | 54.2 | 56.1 | 55.6 | 56.6 | 67.1 | 68.1 | 59.9 | 64.2 |
Right Chart:
| Insurance | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Private | 62.3 | 65.7 | 64.1 | 61.9 | 60.7 | 65.9 | 62.8 | 70.5 | 66.4 | 66.4 | 63.4 | 63.1 |
| Public | 64.7 | 71.7 | 67.6 | 69.1 | 67.6 | 70.1 | 69.3 | 69.9 | 65.0 | 68.1 | 75.0 | 72.6 |
| Uninsured | 51.3 | 46.6 | 46.2 | 49.2 | 48.1 | 52.0 | 52.8 | 48.5 | 54.2 | 60.3 | 49.2 | 52.9 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
Denominator: Civilian noninstitutionalized adult current smokers who had a checkup in the last 12 months.
Notes: Estimates are age adjusted to the 2000 U.S. standard population using three age groups: 18-44, 45-64, and 65 and over. White and Black are non-Hispanic. Hispanic includes all races.
- Importance: Smoking is a modifiable risk factor, and health care providers can help encourage patients to change their behavior and quit smoking. The 2008 update of the Public Health Service Clinical Practice Guideline Treating Tobacco Use and Dependence concludes that counseling and medication are both effective tools alone, but the combination of the two methods is more effective in increasing smoking cessation. For more information, visit http://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/tobacco/index.html.
- Overall Rate: In 2013, the percentage of adult current smokers with a checkup in the last 12 months who received advice from a doctor to quit smoking was 66.5%.
- Trends:
- From 2002 to 2013, the percentage of adult current smokers with a checkup in the last 12 months who received advice from a doctor to quit smoking increased overall (from 63.1% to 66.5%), for Hispanics (from 52.0% to 64.2%), and for Whites (from 64.8% to 68.1%).
- Groups With Disparities:
- In 2013, among adult current smokers ages 18-64 with a checkup, those with public health insurance (72.6%) were more likely than those with private health insurance (63.1%) to receive advice from a doctor to quit smoking.
- In 2013, among adult current smokers ages 18-64 with a checkup, those who were uninsured (52.9%) were less likely than those with private insurance (63.1%) to receive advice from a doctor to quit smoking.
- In all years except 2011, uninsured adult current smokers ages 18-64 with a checkup were less likely to receive advice to quit smoking compared with those with private insurance.
- From 2002 to 2013, there was no statistically significant change in the disparity between uninsured and privately insured adult current smokers with a checkup in the last 12 months who received advice from a doctor to quit smoking.
Slide 63
Prevention: Counseling for Adults About Exercise
- About one-third of adults (34.9%) are obese:
- Obesity-related conditions are among the leading causes of preventable death, such as heart disease, stroke, type 2 diabetes, and some cancers.4
- Physicians encounter many high-risk individuals, whom they can educate about personal risks and lifestyle changes that can help reduce weight and increase activity.5
Slide 64
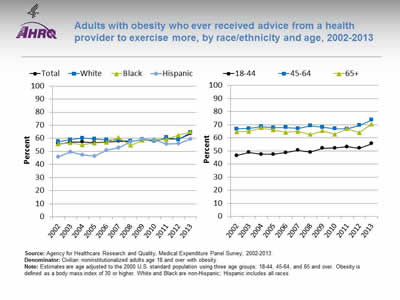
Adults with obesity who ever received advice from a health provider to exercise more, by race/ethnicity and age, 2002-2013
Image: Charts show adults with obesity who ever received advice from a health provider to exercise more, by race/ethnicity and age:
Left Chart:
| Race / Ethnicity | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 55.6 | 57.0 | 57.2 | 56.7 | 57.1 | 57.9 | 57.4 | 59.1 | 58.4 | 59.6 | 59.3 | 63.5 |
| White | 57.5 | 59.0 | 60.1 | 59.7 | 58.8 | 58.7 | 57.8 | 59.1 | 57.8 | 60.7 | 58.9 | 64.5 |
| Black | 55.8 | 56.6 | 55.1 | 56.3 | 56.8 | 60.8 | 54.7 | 58.5 | 59.1 | 59.2 | 62.4 | 64.8 |
| Hispanic | 45.9 | 49.7 | 47.4 | 46.5 | 50.8 | 52.8 | 57.2 | 59.4 | 58.8 | 55.7 | 55.9 | 59.5 |
Right Chart:
| Year | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 18-44 | 46.5 | 48.8 | 47.4 | 47.4 | 48.7 | 50.4 | 49.0 | 52.0 | 52.1 | 53.1 | 52 | 55.5 |
| 45-64 | 66.8 | 67.1 | 68.6 | 67.8 | 68.0 | 67.1 | 69.2 | 68.0 | 67.0 | 66.8 | 69.5 | 73.7 |
| 65+ | 64.6 | 64.9 | 67.6 | 66.0 | 64.3 | 64.9 | 62.6 | 65.5 | 62.7 | 66.9 | 64 | 70.6 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
Denominator: Civilian noninstitutionalized adults age 18 and over with obesity.
Notes: Estimates are age adjusted to the 2000 U.S. standard population using three age groups: 18-44, 45-64, and 65 and over. Obesity is defined as a body mass index of 30 or higher. White and Black are non-Hispanic; Hispanic includes all races.
- Importance: Physician-based exercise and diet counseling is an important component of effective weight loss interventions. Such interventions have been shown to increase levels of physical activity among sedentary patients, resulting in a sustained favorable body weight and body composition.5
- Overall Rate: In 2013, the overall percentage of adults with obesity who had ever received advice from a health provider to exercise more was 63.5%.
- Trends:
- From 2002 to 2013, the percentage of obese adults who ever received advice from a health provider to exercise more increased overall (from 55.6% to 63.5%), for Hispanics (from 45.9% to 59.5%), and for Blacks (from 55.8% to 64.8%).
- From 2002 to 2013, the percentage of obese adults who ever received advice from a health provider to exercise more increased for those ages 18-44 (from 46.5% to 55.5%).
- Groups With Disparities:
- In 2013, obese Hispanic adults (59.5%) were less likely than White obese adults (64.5%) to ever receive advice from a health provider to exercise more.
- In 8 of 12 years, obese Hispanic adults were less likely than White obese adults to ever receive advice from a health provider to exercise more.
- From 2002 to 2013, the disparity between Hispanic and White obese adults who ever received advice from a doctor to exercise more grew smaller but was still present.
- In 2013, obese adults ages 45-64 (73.7%) and age 65 and over (70.6%) were more likely than those ages 18-44 (55.5%) to ever receive advice from a doctor to exercise more.
- In all years, obese adults ages 45-64 and age 65 and over were more likely than those ages 18-44 to ever receive advice from a doctor to exercise more.
Slide 65
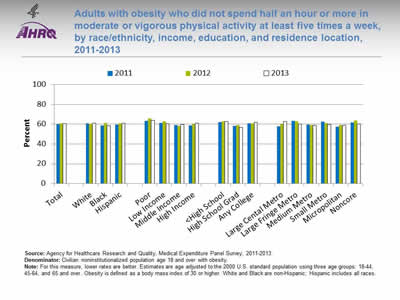
Adults with obesity who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week, by race/ethnicity, income, education, and residence location, 2011-2013
Image: Chart shows adults with obesity who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week, by race/ethnicity, income, education, and residence location:
| Characteristics | 2011 | 2012 | 2013 |
|---|---|---|---|
| Total | 60.1 | 60.7 | 60.5 |
| White | 60.6 | 60.4 | 61.1 |
| Black | 58.9 | 61.3 | 58.3 |
| Hispanic | 59.6 | 60.6 | 61.2 |
| Poor | 63.5 | 66.0 | 64.0 |
| Low Income | 61.4 | 62.8 | 60.5 |
| Middle Income | 59.3 | 58.5 | 59.7 |
| High Income | 58.5 | 59.7 | 60.9 |
| <High School | 62.0 | 62.9 | 62.5 |
| High School Grad | 58.1 | 59.0 | 56.9 |
| Any College | 60.6 | 60.8 | 61.7 |
| Large Cental Metro | 57.9 | 60.1 | 62.8 |
| Large Fringe Metro | 63.3 | 63.0 | 60.2 |
| Medium Metro | 59.5 | 59.1 | 58.9 |
| Small Metro | 62.4 | 61.1 | 59.9 |
| Micropolitan | 57.3 | 59.1 | 58.9 |
| Noncore | 61.5 | 63.7 | 60.1 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2011-2013.
Denominator: Civilian noninstitutionalized population age 18 and over with obesity.
Notes: For this measure, lower rates are better. Estimates are age adjusted to the 2000 U.S. standard population using three age groups: 18-44, 45-64, and 65 and over. Obesity is defined as a body mass index of 30 or higher. White and Black are non-Hispanic; Hispanic includes all races.
- Importance: The 2008 Physical Activity Guidelines for Americans recommend that adults engage in at least 2 hours and 30 minutes a week of moderate-intensity physical activity or 1 hour and 15 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. For more information, visit http://health.gov/paguidelines/guidelines/.
- Overall Rate: In 2013, the overall percentage of adults with obesity who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week was 60.5%.
- Groups With Disparities:
- In 2013, there were no statistically significant differences by race/ethnicity, income, education, or residence location in the percentage of adults with obesity who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week.
Slide 66
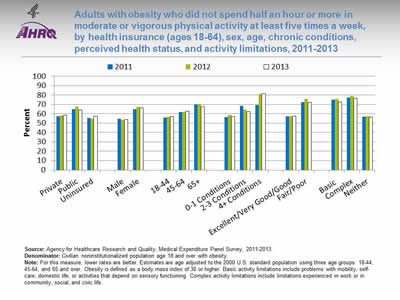
Adults with obesity who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week, by health insurance (ages 18-64), sex, age, chronic conditions, perceived health status, and activity limitations, 2011-2013
Image: Chart shows adults with obesity who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week, by health insurance, sex, age, chronic conditions, perceived health status, and activity limitations:
| Characteristics | 2011 | 2012 | 2013 |
|---|---|---|---|
| Private | 57.3 | 58.1 | 58.4 |
| Public | 65.0 | 67.3 | 64.2 |
| Uninsured | 55.4 | 54.9 | 57.6 |
| Male | 54.8 | 53.5 | 54.0 |
| Female | 65.1 | 67.5 | 66.5 |
| 18-44 | 56.0 | 56.9 | 56.9 |
| 45-64 | 61.7 | 62.3 | 62.7 |
| 65+ | 69.8 | 69.7 | 67.6 |
| 0-1 Conditions | 56.5 | 58.5 | 57.0 |
| 2-3 Conditions | 68.5 | 64.5 | 62.5 |
| 4+ Conditions | 69.1 | 81.5 | 81.5 |
| Excellent / Very Good / Good | 57.1 | 57.1 | 57.6 |
| Fair / Poor | 72.6 | 75.9 | 72.1 |
| Basic | 75.1 | 75.9 | 72.6 |
| Complex | 77.3 | 78.9 | 76.8 |
| Neither | 56.9 | 57.1 | 56.6 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2011-2013.
Denominator: Civilian noninstitutionalized population age 18 and over with obesity.
Notes: For this measure, lower rates are better. Estimates are age adjusted to the 2000 U.S. standard population using three age groups: 18-44, 45-64, and 65 and over. Obesity is defined as a body mass index of 30 or higher. Basic activity limitations include problems with mobility, self-care, domestic life, or activities that depend on sensory functioning. Complex activity limitations include limitations experienced in work or in community, social, and civic life.
- Groups With Disparities:
- In 2013, there were no statistically significant differences by health insurance in the percentage of obese adults ages 18-64 who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week.
- In 2011 and 2012, adults ages 18-64 with obesity with only public insurance were less likely to spend half an hour or more in vigorous physical activity at least five times a week compared with those with private insurance.
- In 2013, the percentage of adults with obesity who did not spend half an hour or more in moderate or vigorous physical activity at least five times a week was higher for:
- Females (66.5%) compared with males (54.0%).
- Those ages 45-64 (62.7%) and age 65 and over (67.6%) compared with those ages 18-44 (56.9%).
- Those with 4 or more chronic conditions (81.5%) compared with those with 0-1 chronic conditions (57.0%).
- Those who perceived their health status to be fair or poor (72.1%) compared with those who perceived their health status to be excellent, very good, or good (57.6%).
- Those with basic (72.6%) or complex activity limitations (76.8%) compared with those with neither limitation (56.6%).
Slide 67
Prevention: Counseling About Exercise for Children and Adolescents
- About 17% of children and adolescents ages 2-19 are overweight or obese.6
- Childhood is when people can establish healthy lifelong habits, and physicians can play an important role in encouraging healthy behaviors.
- The 2008 Physical Activity Guidelines for Americans recommend that children and adolescents engage in 1 hour or more of physical activity everyday.
Note:
- For more information, visit www.health.gov/paguidelines/guidelines/default.aspx.
Slide 68
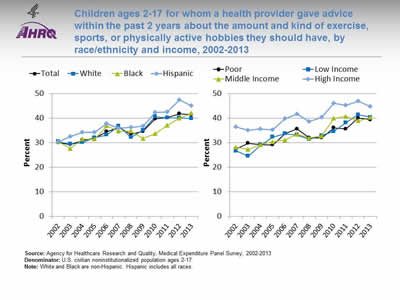
Children ages 2-17 for whom a health provider gave advice within the past 2 years about the amount and kind of exercise, sports, or physically active hobbies they should have, by race/ethnicity and income, 2002-2013
Image: Charts show children ages 2-17 for whom a health provider gave advice within the past 2 years about the amount and kind of exercise, sports, or physically active hobbies they should have, by race/ethnicity and income:
Left Chart:
| Race / Ethnicity | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 30.0 | 29.3 | 31.0 | 31.9 | 34.6 | 36.2 | 33.5 | 34.7 | 39.7 | 40.2 | 41.8 | 41.4 |
| White | 30.5 | 29.5 | 30.1 | 32.1 | 33.2 | 36.8 | 32.2 | 35.2 | 40.6 | 40.1 | 40.1 | 39.9 |
| Black | 30.5 | 27.7 | 31.5 | 31.5 | 36.9 | 34.7 | 34.7 | 31.7 | 33.7 | 37.0 | 40.1 | 42.0 |
| Hispanic | 30.4 | 32.5 | 34.2 | 34.3 | 37.8 | 36.0 | 36.3 | 36.8 | 42.3 | 42.6 | 47.5 | 45.1 |
Right Chart:
| Income | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Poor | 27.5 | 29.8 | 29.3 | 29.1 | 33.7 | 35.6 | 32.0 | 32.0 | 36.0 | 35.6 | 40.0 | 39.4 |
| Low Income | 26.7 | 24.5 | 28.9 | 32.4 | 33.6 | 33.2 | 31.4 | 32.9 | 34.6 | 38.2 | 41.4 | 40.4 |
| Middle Income | 28.2 | 27.2 | 29.2 | 30.4 | 31.0 | 33.4 | 31.9 | 32.8 | 39.9 | 40.7 | 38.9 | 40.3 |
| High Income | 36.4 | 35.0 | 35.6 | 35.2 | 39.9 | 41.6 | 38.6 | 40.3 | 46.1 | 45.2 | 46.9 | 44.8 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
Denominator: U.S. civilian noninstitutionalized population ages 2-17.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Importance: Physicians can educate children and parents about the importance of regular exercise and healthy eating.
- Overall Rate: In 2013, the overall percentage of children ages 2-17 for whom a health provider gave advice within the past 2 years about the amount and kind of exercise, sports, or physically active hobbies they should have was 41.4%.
- Trends:
- From 2002 to 2013, the percentage of children ages 2-17 for whom a health provider gave advice within the past 2 years about the amount and kind of exercise, sports, or physically active hobbies they should have increased overall (from 30.0% to 41.4%), for Hispanics (from 30.4% to 45.1%), for Blacks (from 30.5% to 42.0%), and for Whites (from 30.5% to 39.9%).
- From 2002 to 2013, the percentage of children ages 2-17 whose health providers gave advice about exercise increased for children in all income groups (poor, from 27.5% to 39.4%; low income, from 26.7% to 40.4%; middle income, from 28.2% to 40.3%; and high income, from 36.4% to 44.8%).
- Group With Disparities:
- In 2013, there were no statistically significant differences by race/ethnicity or income in the percentage of children ages 2-17 whose health providers gave advice about exercise.
Slide 69
Prevention: Counseling for Adults About Healthy Eating
- An important factor in maintaining a healthy body weight is changing eating habits to incorporate nutritious food and beverages.
- The U.S. Department of Agriculture created the Dietary Guidelines for Americans to help people understand the complexity of healthy eating for both children and adults.
Note:
- For more information, visit www.dietaryguidelines.gov.
Slide 70
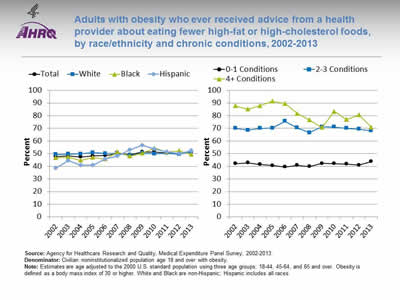
Adults with obesity who ever received advice from a health provider about eating fewer high-fat or high-cholesterol foods, by race/ethnicity and chronic conditions, 2002-2013
Image: Charts show adults with obesity who ever received advice from a health provider about eating fewer high-fat or high-cholesterol foods, by race/ethnicity and chronic conditions:
Left Chart:
| Race / Ethnicity | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 47.7 | 48.3 | 47.4 | 48.1 | 48.5 | 50.0 | 49.2 | 51.3 | 51.4 | 50.6 | 50.2 | 51.3 |
| White | 49.3 | 49.7 | 49.9 | 50.9 | 50.1 | 50.2 | 48.7 | 50.4 | 49.8 | 50.4 | 49.5 | 51.5 |
| Black | 46.7 | 47.4 | 44.7 | 47.1 | 45.8 | 51.3 | 48.0 | 50.3 | 54.5 | 51.3 | 52.3 | 49.3 |
| Hispanic | 38.6 | 44.3 | 41.0 | 40.9 | 45.7 | 48.1 | 53.0 | 56.7 | 53.7 | 51.2 | 50.2 | 52.3 |
Right Chart:
| No. of Conditions | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0-1 Conditions | 42.1 | 42.8 | 41.5 | 40.7 | 39.5 | 40.9 | 39.9 | 42.3 | 42.1 | 41.7 | 40.9 | 43.7 |
| 2-3 Conditions | 70.0 | 68.6 | 70.1 | 70.1 | 75.6 | 70.3 | 66.5 | 71.2 | 71.1 | 70.1 | 69.5 | 68.1 |
| 4+ Conditions | 87.8 | 85.2 | 87.9 | 91.4 | 89.5 | 81.8 | 76.6 | 70.7 | 83.4 | 77.0 | 80.5 | 70.9 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
Denominator: Civilian noninstitutionalized population age 18 and over with obesity.
Notes: Estimates are age adjusted to the 2000 U.S. standard population using three age groups: 18-44, 45-64, and 65 and over. Obesity is defined as a body mass index of 30 or higher. White and Black are non-Hispanic; Hispanic includes all races.
- Importance: Physicians need to emphasize the importance of eating foods from all food groups and balancing energy intake and energy expenditure. Foods from all food groups include whole grains and fibers, lean proteins, complex carbohydrates, fruits and vegetables, and low-fat or fat-free milk and dairy products.
- Overall Rate: In 2013, the overall percentage of adults with obesity who ever received advice from a health provider about eating fewer high-fat or high-cholesterol foods was 51.3%.
- Trends:
- From 2002 to 2013, the percentage of adults with obesity who ever received advice from a health provider about eating fewer high-fat or high-cholesterol foods increased for Hispanics (from 38.6% to 52.3% ).
- From 2002 to 2013, the percentage of obese adults who ever received advice from a health provider about eating fewer high-fat or high-cholesterol foods decreased for those with 4 or more chronic conditions (from 87.8% to 70.9%).
- Groups With Disparities:
- In 2013, obese adults with 2-3 chronic conditions (68.1%) and those with 4 or more chronic conditions (70.9%) were more likely to receive counseling about healthy eating than those with 0-1 chronic conditions (43.7%).
- In all years, obese adults with 2 or more chronic conditions were more likely to receive counseling about healthy eating than those with 0-1 chronic conditions.
Slide 71
Prevention: Counseling for Children About Healthy Eating
- Children and adolescents have become overweight from eating more calories than they burn.
- Children and adolescents consume 35% to 40% of their daily energy in school, so schools need to provide diverse, nutrient-based foods and drinks.7
- The Dietary Guidelines for Americans encourage children and adolescents to maintain a calorie-balanced diet to support normal growth and development without gaining excess weight.
Notes:
- About 30% to 40% of daily calories children and adolescents consume are energy-dense, nutrient-poor foods and drinks.7
- For more information, visit www.dietaryguidelines.gov.
Slide 72
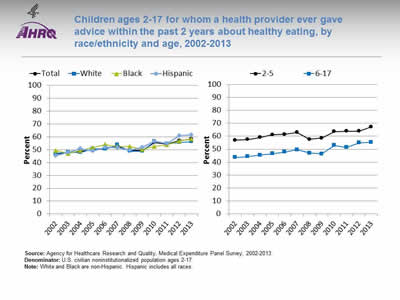
Children ages 2-17 for whom a health provider ever gave advice within the past 2 years about healthy eating, by race/ethnicity and age, 2002-2013
Image: Charts show children ages 2-17 for whom a health provider ever gave advice within the past 2 years about healthy eating, by race/ethnicity and age:
Left Chart:
| Race / Ethnicity | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 46.9 | 47.5 | 48.7 | 50.1 | 51.4 | 52.8 | 49.6 | 49.5 | 55.7 | 54.5 | 57.1 | 58.3 |
| White | 47.2 | 48.1 | 48.0 | 50.7 | 50.5 | 53.7 | 49.0 | 49.0 | 56.5 | 54.5 | 55.6 | 56.3 |
| Black | 49.3 | 47.1 | 49.4 | 51.7 | 54.1 | 52.5 | 52.6 | 50.3 | 52.6 | 53.7 | 56.9 | 58.5 |
| Hispanic | 45.5 | 48.0 | 51.0 | 48.9 | 52.0 | 51.4 | 49.7 | 51.8 | 56.7 | 54.8 | 61.1 | 61.6 |
Right Chart:
| Age | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2-5 | 57.0 | 57.4 | 59.1 | 61.1 | 61.6 | 62.9 | 57.6 | 58.5 | 63.6 | 63.9 | 63.8 | 67.2 |
| 6-17 | 43.7 | 44.3 | 45.4 | 46.5 | 47.9 | 49.6 | 47.0 | 46.4 | 53.0 | 51.4 | 54.9 | 55.4 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, 2002-2013.
Denominator: U.S. civilian noninstitutionalized population ages 2-17.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Importance: It is important to advise parents and guardians to provide balanced diets at home. Eating patterns that are established early in childhood are often adopted later in life, making early interventions important.
- Overall Rate: In 2013, the overall percentage of children ages 2-17 for whom a health provider gave advice within the past 2 years about healthy eating was 58.3%.
- Trends:
- From 2002 to 2013, the percentage of children ages 2-17 for whom a health provider gave advice within the past 2 years about healthy eating improved overall (from 46.9% to 58.3%), for Hispanics (from 45.5% to 61.6%), for Blacks (from 49.3% to 58.5%), and for Whites (from 47.2% to 56.3%).
- From 2002 to 2013, the percentage of children for whom a health provider gave advice about health eating increased for those ages 2-5 (57% to 67.2%) and for those ages 6-17 (43.7% to 55.4%).
- Groups With Disparities:
- In 2013, Hispanic children (61.6%) were more likely than White children (56.3%) to receive advice from a health provider about healthy eating.
- In 2013, children ages 6-17 (55.4%) were less likely than children ages 2-5 (67.2%) to receive advice about healthy eating.
Slide 73
References
- Satcher D, Higginbotham EJ. The public health approach to eliminating disparities in health. Am J Public Health 2008;98(9 Suppl):S8-11. PMID: 18687626. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518593/. Accessed March 23, 2016.
- Ford E, Bergmann M, Boeing H, et al. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev Med 2012 Jul;55(1):23-7. Epub 2012 Apr 29. PMID: 22564893. http://www.sciencedirect.com/science/article/pii/S0091743512001582. Accessed March 23, 2016.
- Office on Smoking and Health. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 2014. http://www.surgeongeneral.gov/library/reports/50-years-of-progress/index.html. Accessed March 23, 2016.
- Adult Obesity Facts. Atlanta, GA: Centers for Disease Control and Prevention; 2014. http://www.cdc.gov/obesity/data/adult.html. Accessed March 23, 2016.
- Lin JS, O'Connor E, Whitlock EP, et al. Behavioral counseling to promote physical activity and a healthful diet to prevent cardiovascular disease in adults: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2010 Dec 7;153(11):736-50. PMID: 21135297. http://annals.org/article.aspx?articleid=746527. Accessed June 26, 2015.
- Childhood Obesity Facts. Atlanta, GA: Centers for Disease Control & Prevention; 2014. http://www.cdc.gov/obesity/data/childhood.html. Accessed March 23, 2016.
- American Academy of Pediatrics, Council on School Health; Committee on Nutrition. Policy Statement. Snacks, sweetened beverages, added sugars, and schools. Pediatrics 2015;135(3):575-83. http://pediatrics.aappublications.org/content/135/3/575.long. Accessed March 23, 2016.
Slide 74
Chartbook on Healthy Living
Clinical Preventive Services
Slide 75
Measures of Clinical Preventive Services: Screening
- Women ages 21-65 years who received a Pap smear in the last 3 years.
- Invasive cervical cancer incidence per 100,000 women age 20 and over.
- Adults who received a blood pressure measurement in the last 2 years and can state whether their blood pressure was normal or high.
Note: Clinical preventive services include screening for early detection of cancer and cardiovascular disease.
Slide 76

Women ages 21-65 years who received a Pap smear in the last 3 years, by education and race, 2000-2013
Image: Charts show women ages 21-65 years who received a Pap smear in the last 3 years, by education and race:
Left Chart:
| Education | 2000 | 2005 | 2008 | 2010 | 2013 |
|---|---|---|---|---|---|
| Total | 87.5 | 85.3 | 84.5 | 82.8 | 80.7 |
| <High School | 78.0 | 72.7 | 75.0 | 67.8 | 68.5 |
| High School Grad | 85.2 | 81.9 | 78.9 | 76.8 | 75.7 |
| Any College | 91.4 | 89.7 | 89.0 | 87.8 | 85.5 |
Right Chart:
| Race | 2000 | 2005 | 2008 | 2010 | 2013 |
|---|---|---|---|---|---|
| White | 88.1 | 86.1 | 85.1 | 83.2 | 81.4 |
| Black | 90.3 | 84.6 | 86.1 | 85.0 | 82.2 |
| Asian | 71.7 | 68.8 | 71.5 | 75.7 | 70.5 |
| AI/AN | 77.6 | 74.7 | 82.0 | 76.9 | 82.1 |
| >1 Race | 86.7 | 90.4 | 86.1 | 75.2 | 77.7 |
Key: AI/AN = American Indian or Alaska Native.
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey, 2000-2013.
Denominator: Women ages 21-65.
Notes: Measure is age adjusted. Data for this measure are not collected every year.
- Importance: Screening with Pap smears can detect high-grade precancerous cervical lesions that can be removed before they become cancerous.
- Overall: In 2013, 80.7% of women ages 21-65 had received a Pap smear in the last 3 years.
- Trends: From 2000 to 2013, the percentage of women ages 21-65 years who received a Pap smear in the last 3 years decreased overall, among all education groups, and among Black and White women.
- Groups With Disparities: In all years, the percentage of women who received a Pap smear was lower:
- Among Asian women compared with White women. From 2000 to 2013, the disparity grew smaller, but it was still present in 2013.
- Among women with less than a high school education and high school graduates compared with women with any college. From 2000 to 2013, there were no statistically significant differences in the disparities.
Slide 77
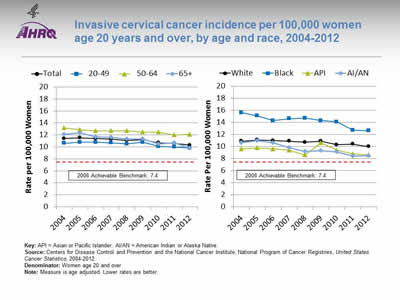
Invasive cervical cancer incidence per 100,000 women age 20 years and over, by age and race, 2004-2012
Image: Charts show invasive cervical cancer incidence per 100,000 women age 20 years and over, by age and race:
Left Chart:
| Age | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|---|---|
| Total | 11.4 | 11.5 | 11.4 | 11.3 | 11.1 | 11.2 | 10.7 | 10.6 | 10.3 |
| 20-49 | 10.6 | 10.8 | 10.8 | 10.7 | 10.5 | 10.8 | 10.1 | 10.0 | 9.8 |
| 50-64 | 13.2 | 12.9 | 12.7 | 12.7 | 12.7 | 12.5 | 12.5 | 12.0 | 12.1 |
| 65+ | 12.1 | 12.4 | 11.7 | 11.6 | 11.3 | 11.3 | 10.5 | 10.7 | 9.8 |
Right Chart:
| Race | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|---|---|
| White | 10.9 | 11.1 | 11.0 | 10.9 | 10.7 | 10.9 | 10.3 | 10.4 | 10.0 |
| Black | 15.6 | 15.1 | 14.3 | 14.6 | 14.7 | 14.3 | 14.1 | 12.7 | 12.6 |
| API | 9.6 | 9.8 | 9.6 | 9.4 | 8.6 | 10.6 | 9.4 | 8.8 | 8.6 |
| AI/AN | 10.6 | 11.0 | 10.6 | 9.8 | 9.2 | 9.3 | 9.1 | 8.4 | 8.5 |
2008 Achievable Benchmark: 7.4.
Key: API = Asian or Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: Centers for Disease Control and Prevention and the National Cancer Institute, National Program of Cancer Registries, United States Cancer Statistics, 2004-2012.
Denominator: Women age 20 and over.
Notes: Measure is age adjusted. Lower rates are better.
- Importance: Since the implementation of widespread screening with Pap smears, rates of invasive cervical cancer have fallen dramatically. Most cases now occur among women who have not been appropriately screened.
- Overall: In 2012, the overall rate of invasive cervical cancer per 100,000 women age 20 years and over was 10.3.
- Trends: From 2004 to 2012, rates of invasive cervical cancer fell overall and among all age groups and racial/ethnic groups.
- Groups With Disparities:
- In 2012, rates of invasive cervical cancer were higher:
- Among women ages 50-64 compared with women ages 20-49.
- Among Black women compared with White women. From 2004 to 2012, this disparity grew smaller, but it was still present in 2012.
- In 2012, rates of invasive cervical cancer were lower among Asian and Pacific Islander women compared with White women.
- In 2012, rates of invasive cervical cancer were higher:
- Achievable Benchmark:
- The 2008 top 5 State achievable benchmark was 7.4 per 100,000 women. The top 5 States that contributed to the achievable benchmark are Connecticut, Kansas, Massachusetts, Utah, and Wisconsin.
- At the current annual rates of decrease, this benchmark would not be attained for more than 14 years overall and approximately 18 years for people ages 20-49 and 50-64. Most racial groups could achieve it within 15 years. API women could achieve the benchmark in 3 years and women age 65 and over could achieve it in 6 years.
Slide 78
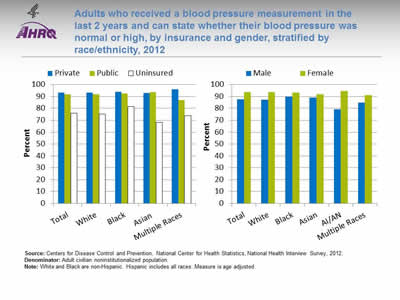
Adults who received a blood pressure measurement in the last 2 years and can state whether their blood pressure was normal or high, by insurance and gender, stratified by race/ethnicity, 2012
Image: Charts show adults who received a blood pressure measurement in the last 2 years and can state whether their blood pressure was normal or high, by insurance and gender, stratified by race/ethnicity:
Left Chart:
| Insurance | Total | White | Black | Asian | Multiple Races |
|---|---|---|---|---|---|
| Private | 93.4 | 93.3 | 93.9 | 92.9 | 95.9 |
| Public | 91.7 | 91.8 | 92.7 | 93.6 | 87 |
| Uninsured | 75.9 | 75.1 | 81.5 | 68.1 | 73.7 |
Right Chart:
| Sex | Total | White | Black | Asian | AI/AN | Multiple Races |
|---|---|---|---|---|---|---|
| Male | 87.5 | 87.3 | 89.6 | 89.2 | 79.2 | 84.7 |
| Female | 93.5 | 93.6 | 93.4 | 91.8 | 94.6 | 91.3 |
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey, 2012.
Denominator: Adult civilian noninstitutionalized population.
Notes: White and Black are non-Hispanic. Hispanic includes all races. Measure is age adjusted.
- Importance: Early detection and treatment of high blood pressure can prevent heart failure, kidney failure, and stroke. Because high blood pressure typically causes no symptoms, screening is essential.
- Overall: In 2012, the percentage of adults who received a blood pressure measurement in the last 2 years and can state whether their blood pressure was normal or high was 90.6% (data not shown).
- Groups With Disparities:
- In 2012, overall, the percentage of adults who received a blood pressure measurement was lower for people with public insurance and those who were uninsured compared with people with private insurance.
- In 2012, for all races, the percentage of adults who received a blood pressure measurement was lower for people who were uninsured compared with people with private insurance.
- In 2012, the percentage of adults who received a blood pressure measurement was higher for females compared with males overall and for Whites, Blacks, and American Indians and Alaska Natives.
Slide 79
Measures of Clinical Preventive Services: Immunization
- Adults age 65 years and over who ever received pneumococcal immunization.
- Hospital patients who received:
- Pneumococcal immunization.
- Influenza immunization.
- Long-stay nursing home residents who were assessed and appropriately given:
- Pneumococcal immunization.
- Influenza immunization.
Note: Important adult immunizations include pneumococcal and influenza immunization. Childhood and adolescent immunizations are presented in the section of this chartbook on Maternal and Child Health Care.
Slide 80
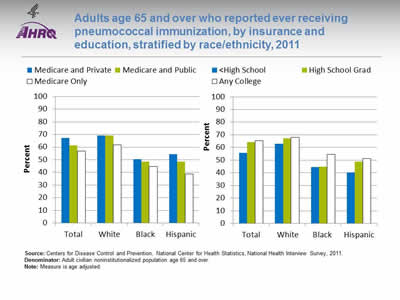
Adults age 65 and over who reported ever receiving pneumococcal immunization, by insurance and education, stratified by race/ethnicity, 2011
Image: Charts show adults age 65 and over who reported ever receiving pneumococcal immunization, by insurance and education, stratified by race/ethnicity:
Left Chart:
| Insurance | Total | White | Black | Hispanic |
|---|---|---|---|---|
| Medicare and Private | 67.3 | 69.3 | 50.5 | 54.3 |
| Medicare and Public | 61.4 | 69.2 | 48.4 | 48.5 |
| Medicare Only | 56.8 | 61.8 | 44.8 | 38.9 |
Right Chart:
| Education | Total | White | Black | Hispanic |
|---|---|---|---|---|
| <High School | 55.8 | 62.8 | 44.4 | 40.2 |
| High School Grad | 64.1 | 67.3 | 44.7 | 48.7 |
| Any College | 65.5 | 67.9 | 54.4 | 51.2 |
Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Health Interview Survey, 2011.
Denominator: Adult civilian noninstitutionalized population age 65 and over.
Notes: Measure is age adjusted.
- Importance: Immunization is a cost-effective strategy for reducing illness, death, and disparities associated with pneumococcal disease.
- Overall: In 2011, the percentage of adults age 65 years and over who reported ever receiving pneumococcal immunization was 62.7% (data not shown).
- Groups With Disparities:
- In 2011, overall, the percentage of adults who ever received pneumococcal immunization was lower for those with Medicare only and Medicare and public insurance compared with those with Medicare and private insurance.
- In 2011, the percentage of adults who ever received pneumococcal immunization was lower for Hispanic and White adults with Medicare only compared with those with Medicare and private insurance.
- In 2011, overall and for all racial/ethnic groups, the percentage of adults who ever received pneumococcal immunization was lower for adults with less than a high school education compared with those with any college.
Slide 81
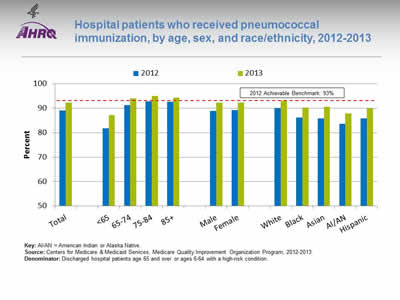
Hospital patients who received pneumococcal immunization, by age, sex, and race/ethnicity, 2012-2013
Image: Chart shows hospital patients who received pneumococcal immunization, by age, sex, and race/ethnicity:
| Characteristics | 2012 | 2013 |
|---|---|---|
| Total | 89 | 92.2 |
| <65 | 81.8 | 87.2 |
| 65-74 | 91.3 | 94.0 |
| 75-84 | 92.8 | 94.9 |
| 85+ | 92.5 | 94.3 |
| Male | 88.8 | 92.2 |
| Female | 89.1 | 92.3 |
| White | 90.0 | 92.8 |
| Black | 86.1 | 90.3 |
| Asian | 85.7 | 90.5 |
| AI/AN | 83.5 | 87.9 |
| Hispanic | 85.8 | 89.8 |
2012 Achievable Benchmark: 93%.
Key: AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Medicare Quality Improvement Organization Program, 2012-2013.
Denominator: Discharged hospital patients age 65 and over or ages 6-64 with a high-risk condition.
Notes:
- Importance: Hospitals are important sites for ensuring people receive needed immunizations, including pneumococcal immunization.
- Overall Rate: In 2013, 92.2% of hospital patients received pneumococcal immunization.
- Groups With Disparities:
- In 2012 and 2013, the percentage of hospital patients who received pneumococcal immunization was higher for people ages 65-74, 75-84, and 85+ compared with people less than 65.
- In both years, the percentage of hospital patients who received pneumococcal immunization was lower for Blacks, Asians, American Indians and Alaska Natives, and Hispanics compared with Whites.
- Achievable Benchmark:
- The 2012 top 5 State achievable benchmark was 93%. The top 5 States that contributed to the achievable benchmark are Delaware, Florida, Ohio, South Carolina, and West Virginia.
- In 2013, adults age 65 and over achieved the benchmark. All other groups were below the benchmark.
Slide 82
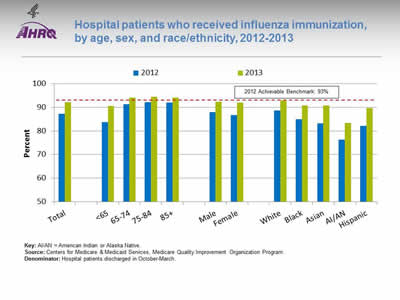
Hospital patients who received influenza immunization, by age, sex, and race/ethnicity, 2012-2013
Image: Chart shows hospital patients who received influenza immunization, by age, sex, and race/ethnicity:
| Characteristics | 2012 | 2013 |
|---|---|---|
| Total | 87.2 | 92.2 |
| <65 | 83.7 | 90.6 |
| 65-74 | 91.4 | 94.1 |
| 75-84 | 92.2 | 94.5 |
| 85+ | 92.0 | 94.1 |
| Male | 88.0 | 92.4 |
| Female | 86.7 | 92.1 |
| White | 88.6 | 92.8 |
| Black | 84.9 | 90.7 |
| Asian | 83.3 | 90.8 |
| AI/AN | 76.3 | 83.4 |
| Hispanic | 82.2 | 89.7 |
2012 Achievable Benchmark: 93%.
Key: AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Medicare Quality Improvement Organization Program.
Denominator: Hospital patients discharged in October-March.
Notes:
- Importance: Hospitals are important sites for ensuring people receive needed immunizations, including influenza immunization.
- Overall Rate: in 2013, 92.2% of hospital patients received influenza immunization.
- Groups With Disparities:
- In 2012 and 2013, the percentage of hospital patients who received influenza immunization was higher for people ages 65-74, 75-84, and 85 and over compared with people less than 65.
- In 2012, the percentage of hospital patients who received influenza immunization was lower for females compared with males.
- In both years, the percentage of hospital patients who received influenza immunization was lower for Blacks, Asians, American Indians and Alaska Natives, and Hispanics compared with Whites.
- Achievable Benchmark:
- The 2012 top 5 State achievable benchmark was 93%. The top 5 States that contributed to the achievable benchmark are Delaware, Maryland, New Hampshire, South Carolina, and West Virginia.
- In 2013, adults age 65 and over achieved the benchmark. All other groups were below the benchmark.
Slide 83
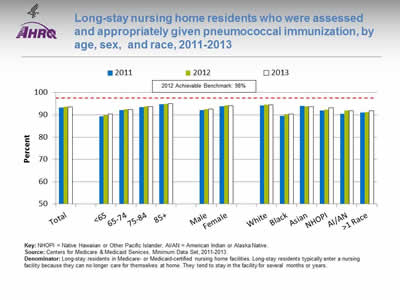
Long-stay nursing home residents who were assessed and appropriately given pneumococcal immunization, by age, sex, and race, 2011-2013
Image: Chart shows long-stay nursing home residents who were assessed and appropriately given pneumococcal immunization, by age, sex, and race:
| Characteristics | 2011 | 2012 | 2013 |
|---|---|---|---|
| Total | 93.3 | 93.6 | 93.6 |
| <65 | 89.4 | 89.9 | 90.3 |
| 65-74 | 92.2 | 92.5 | 92.4 |
| 75-84 | 93.5 | 93.8 | 93.7 |
| 85+ | 94.8 | 95.0 | 95.0 |
| Male | 92.1 | 92.5 | 92.6 |
| Female | 93.9 | 94.2 | 94.1 |
| White | 94.3 | 94.5 | 94.5 |
| Black | 89.6 | 90.2 | 90.4 |
| Asian | 93.9 | 93.9 | 93.7 |
| NHOPI | 91.9 | 92.4 | 93.2 |
| AI/AN | 90.5 | 91.9 | 91.8 |
| >1 Race | 91.0 | 91.2 | 91.9 |
2012 Achievable Benchmark: 98%.
Key: NHOPI = Native Hawaiian or Other Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Minimum Data Set, 2011-2013.
Denominator: Long-stay residents in Medicare- or Medicaid-certified nursing home facilities. Long-stay residents typically enter a nursing facility because they can no longer care for themselves at home. They tend to stay in the facility for several months or years.
Notes:
- Importance: Nursing homes are also important sites for ensuring people receive needed immunizations, including pneumococcal immunization.
- Overall Rate: In 2013, 93.6% of long-stay nursing home residents were assessed and appropriately given pneumococcal immunization.
- Groups With Disparities:
- From 2011 to 2013, the percentage of nursing home residents who were assessed and appropriately given pneumococcal immunization was higher:
- Among residents ages 65-74, 75-84, and 85 and over compared with residents less than 65.
- Among female residents compared with male residents.
- From 2011 to 2013, the percentage of nursing home residents who were assessed and appropriately given pneumococcal immunization was lower:
- Among Blacks, Native Hawaiians and Other Pacific Islanders, American Indians and Alaska Natives, and multiple-race residents compared with Whites.
- From 2012 to 2013, the percentage of nursing home residents who were assessed and appropriately given pneumococcal immunization was lower:
- Among Asians compared with Whites.
- From 2011 to 2013, the percentage of nursing home residents who were assessed and appropriately given pneumococcal immunization was higher:
- Achievable Benchmark:
- The 2012 top 5 State achievable benchmark was 98%. The top 5 States that contributed to the achievable benchmark are Alaska, Delaware, New Hampshire, North Dakota, and Wisconsin.
- All groups were below the benchmark.
Slide 84
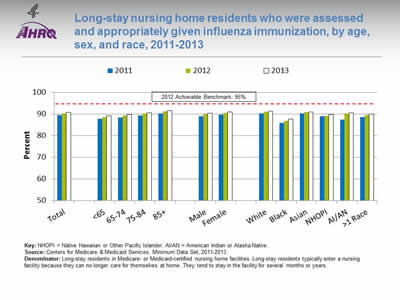
Long-stay nursing home residents who were assessed and appropriately given influenza immunization, by age, sex, and race, 2011-2013
Image: Chart shows long-stay nursing home residents who were assessed and appropriately given influenza immunization, by age, sex, and race:
| Characteristics | 2011 | 2012 | 2013 |
|---|---|---|---|
| Total | 89.5 | 90.4 | 90.8 |
| <65 | 87.8 | 88.6 | 89.3 |
| 65-74 | 88.5 | 89.3 | 89.8 |
| 75-84 | 89.4 | 90.3 | 90.7 |
| 85+ | 90.5 | 91.3 | 91.7 |
| Male | 89.1 | 89.9 | 90.5 |
| Female | 89.7 | 90.6 | 91.0 |
| White | 90.4 | 91.2 | 91.5 |
| Black | 86.0 | 86.8 | 87.7 |
| Asian | 90.4 | 91.0 | 91.1 |
| NHOPI | 89.1 | 89.2 | 89.9 |
| AI/AN | 87.5 | 90.4 | 90.7 |
| >1 Race | 88.6 | 89.6 | 90.1 |
2012 Achievable Benchmark: 95%.
Key: NHOPI = Native Hawaiian or Other Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Minimum Data Set, 2011-2013.
Denominator: Long-stay residents in Medicare- or Medicaid-certified nursing home facilities. Long-stay residents typically enter a nursing facility because they can no longer care for themselves at home. They tend to stay in the facility for several months or years.
Notes:
- Importance: Nursing home residents are at particularly high risk for contracting and developing serious complications of influenza.
- Overall Rate: In 2013, 90.8% of long-stay nursing home residents were assessed and appropriately given influenza immunization.
- Groups With Disparities:
- From 2011 to 2013, the percentage of nursing home residents who were assessed and appropriately given influenza immunization was higher:
- Among residents ages 75-84 and 85 and over compared with residents less than 65.
- From 2011 to 2013, the percentage of nursing home residents who were assessed and appropriately given influenza immunization was lower:
- Among Black and multiple-race residents compared with White residents.
- In 2012 and 2013, the percentage of nursing home residents who were assessed and appropriately given pneumococcal immunization was lower among Native Hawaiians and Other Pacific Islanders compared with Whites.
- From 2011 to 2013, the percentage of nursing home residents who were assessed and appropriately given influenza immunization was higher:
- Achievable Benchmark:
- The 2012 top 5 State achievable benchmark was 95%. The top 5 States that contributed to the achievable benchmark are Hawaii, Iowa, New Hampshire, North Dakota, and South Dakota.
- All groups were below the benchmark.
Slide 85
Chartbook on Healthy Living
Functional Status Preservation and Rehabilitation
Slide 86
Interventions To Maintain and Improve Functional Status
- Some interventions can help prevent diseases that commonly cause declines in functional status:
- Promoting physical activity.
- Promoting social interaction.
- Other interventions can help patients regain lost function or minimize the rate of decline in function:
- Physical therapy.
- Occupational therapy.
- Speech-language therapy.
Slide 87
Settings for Services
- Services are delivered in a variety of settings:
- Hospitals.
- Providers' offices.
- Patients' homes.
- Long-term care facilities.
- Other post-acute care or rehabilitation facilities.
Slide 88
Functional Status Preservation and Rehabilitation Measures
- Improvement in mobility among home health care patients.
- Nursing home residents needing more help with daily activities.
Slide 89
Improvement in Mobility Among Home Health Care Patients
- Home care services play an integral role in helping older adults preserve independence, remain in the community, and delay or avoid institutionalization.1
- Home-based physical therapy assists people in restoring strength, balance, and mobility after an illness or injury.2
Slide 90
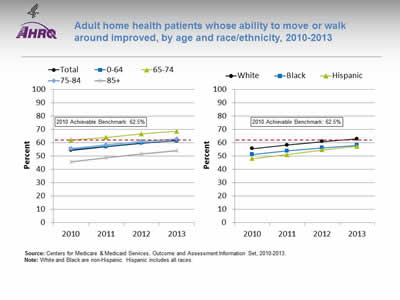
Adult home health patients whose ability to move or walk around improved, by age and race/ethnicity, 2010-2013
Image: Charts show adult home health patients whose ability to move or walk around improved, by age and race/ethnicity:
Left Chart:
| Age | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|
| Total | 54.4 | 57 | 59.7 | 61.8 |
| 0-64 | 55 | 57.3 | 59.8 | 61.5 |
| 65-74 | 62 | 64.1 | 66.7 | 68.6 |
| 75-84 | 55.7 | 58.5 | 60.9 | 63.0 |
| 85+ | 45.6 | 48.7 | 51.7 | 54.1 |
Right Chart:
| Year | White | Black | Hispanic |
|---|---|---|---|
| 2010 | 55.6 | 51.2 | 48.1 |
| 2011 | 58.2 | 53.8 | 51.1 |
| 2012 | 60.9 | 56.2 | 54.7 |
| 2013 | 62.9 | 58.1 | 57.2 |
2010 Achievable Benchmark: 62.5%.
Source: Centers for Medicare & Medicaid Services, Outcome and Assessment Information Set, 2010-2013.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Importance: Many patients who receive home health care are recovering from an injury or illness and may have difficulty walking or moving around safely. Maintaining and improving functional status, such as patients' ability to ambulate, improves quality of life and allows them to stay at home as long as possible. Getting better at walking or moving around may be a sign that their health status is improving.
- Overall Rate: In 2013, 61.8% of home health care patients showed improvement in walking or moving around.
- Trends: From 2010 to 2013, the percentage of home health care patients who showed improvement in walking or moving around increased overall and for all age and racial/ethnic groups.
- Groups With Disparities:
- From 2010 to 2013, home health patients ages 65-74 were more likely than those under age 65 to get better at walking or moving around.
- In all years, home health patients age 85 and over were less likely than those under age 65 to get better at walking or moving around.
- In all years, Hispanic home health patients were less likely than White home health patients to get better at walking or moving around. From 2010 to 2013, there was no statistically significant change in this disparity.
- From 2011 to 2013, Black home health care patients were less likely than White patients to get better at walking or moving around.
- Achievable Benchmark:
- The 2010 top 5 State achievable benchmark was 62.5%. The top 5 States that contributed to the achievable benchmark are Maine, Missouri, New Jersey, South Carolina, and Utah.
- Whites and adults ages 65-74 and 75-84 have achieved the benchmark.
- At current rates, the overall population could reach the benchmark in less than a year. Adults under age 65 could reach the benchmark in less than a year and those age 85 and over would take 4 years.
- Blacks and Hispanics could achieve the benchmark in 3 years.
Slide 91
Nursing Home Residents Needing More Help With Daily Activities
- Independence in activities of daily living (ADLs) is positively associated with quality of life.
- ADL impairments are strongly associated with poorer physical health, hospital admission, increased cost, and death.
- A resident's ADL status and likely pattern of change over time are important considerations in determining care priorities.3
Note: ADLs are basic personal care activities such as dressing, eating, and moving about.
Slide 92
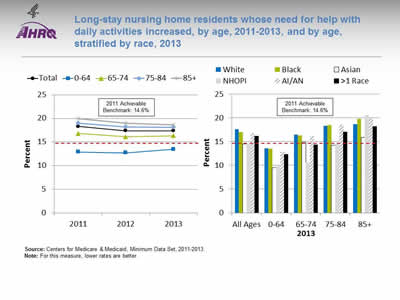
Long-stay nursing home residents whose need for help with daily activities increased, by age, 2011-2013, and by age, stratified by race, 2013
Image: Charts show long-stay nursing home residents whose need for help with daily activities increased, by age, and by age stratified by race:
Left Chart:
| Year | Total | 0-64 | 65-74 | 75-84 | 85+ |
|---|---|---|---|---|---|
| 2011 | 18.3 | 12.9 | 16.8 | 19 | 20 |
| 2012 | 17.4 | 12.7 | 16.1 | 18.2 | 19 |
| 2013 | 17.4 | 13.5 | 16.3 | 18.2 | 18.6 |
Right Chart:
| Age | White | Black | Asian | NHOPI | AI/AN | >1 Race |
|---|---|---|---|---|---|---|
| All Ages | 17.64 | 16.96 | 14.52 | 14.52 | 16.84 | 16.17 |
| 0-64 | 13.62 | 13.53 | 9.49 | 9.88 | 12.88 | 12.32 |
| 65-74 | 16.46 | 16.31 | 14.84 | 10.62 | 16.12 | 14.40 |
| 75-84 | 18.27 | 18.47 | 14.24 | 14.66 | 18.60 | 17.11 |
| 85+ | 18.62 | 19.79 | 15.94 | 20.55 | 19.88 | 18.20 |
2011 Achievable Benchmark: 14.6%.
Source: Centers for Medicare & Medicaid, Minimum Data Set, 2011-2013.
Notes: For this measure, lower rates are better.
- Importance: Long-stay residents typically enter a nursing facility because they can no longer care for themselves at home. They tend to remain in the facility for several months or years. Most residents want to care for themselves, and the ability to perform daily activities is important to their quality of life. While some functional decline among residents cannot be avoided, high-quality nursing home care should minimize the rate of decline and the number of patients experiencing decline.
- Overall Rate: In 2013, the percentage of long-stay nursing home residents who had increased need for help with daily activities was 17.4%.
- Groups With Disparities:
- From 2011 to 2013, nursing home residents ages 0-64 were less likely than residents in other age groups to need increased help with daily activities.
- In age groups 0-64, 75-84, and 85 and over, Asian residents were less likely than White residents to need increased help with daily activities.
- Achievable Benchmark:
- The 2011 top 5 State achievable benchmark was 14.6%. The top 5 States that contributed to the achievable benchmark are Alaska, California, Illinois, Oregon, and, Utah.
- Residents ages 0-64 had a rate below the benchmark. Residents of all races ages 0-64 had a rate below the benchmark.
- Data are insufficient to determine time to benchmark for other groups.
Slide 93
References
- Lo AT, Gruneir A, Bronskill SE, et al. Sex differences in home care performance: a population-based study. Womens Health Issues 2015 May-Jun;25(3):232-8. Epub 2015 Apr 15. PMID: 25890502. http://www.sciencedirect.com/science/article/pii/S1049386715000055. Accessed March 24, 2016.
- Russell D, Rosati RJ, Andreopoulos E. Continuity in the provider of home-based physical therapy services and its implications for outcomes of patients. Phys Ther 2012 Feb;92(2):227-35. Epub 2011 Nov 10. PMID: 22074941. https://doi.org/10.2522/ptj.20110171. Accessed March 24, 2016.
- Kruse RL, Petroski GF, Mehr DR, et al. Activities of daily living trajectories surrounding acute hospitalization of long-stay nursing home residents. J Am Geriatr Soc Nov;61(11):1909-18. Epub 2013 Oct 28. PMID: 24219192. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3831170/. Accessed March 24, 2016.
Slide 94
Chartbook on Healthy Living
Supportive and Palliative Care
Slide 95
Goals of Supportive and Palliative Care
- Disease cannot always be cured, and functional impairment cannot always be reversed.
- For patients with long-term health conditions, managing symptoms and preventing complications are important goals.
- Supportive and palliative care:
- Cuts across many medical conditions.
- Is delivered by many health care providers.
- Focuses on enhancing patient comfort and quality of life and preventing and relieving symptoms and complications.
Slide 96
Measures of Supportive and Palliative Care
- Improvement in shortness of breath among home health care patients.
- Nursing home residents with moderate to severe pain.
- Nursing home residents who lost too much weight.
Slide 97
Shortness of Breath Among Home Health Care Patients
- Shortness of breath is uncomfortable.
- Many patients with heart or lung problems experience difficulty breathing and may tire easily or be unable to perform daily activities.
- Doctors and home health staff should monitor shortness of breath and may give advice, therapy, medication, or oxygen to help lessen this symptom.
Slide 98
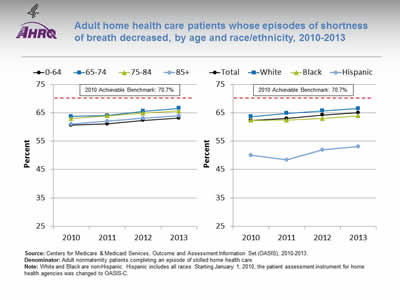
Adult home health care patients whose episodes of shortness of breath decreased, by age and race/ethnicity, 2010-2013
Image: Charts show adult home health care patients whose episodes of shortness of breath decreased, by age and race/ethnicity:
Left Chart:
| Year | 0-64 | 65-74 | 75-84 | 85+ |
|---|---|---|---|---|
| 2010 | 60.6 | 63.7 | 63 | 61 |
| 2011 | 61.1 | 64 | 63.9 | 62.1 |
| 2012 | 62.3 | 65.5 | 64.9 | 63.1 |
| 2013 | 63.2 | 66.6 | 65.6 | 63.9 |
Right Chart:
| Year | Total | White | Black | Hispanic |
|---|---|---|---|---|
| 2010 | 62.3 | 63.6 | 62.3 | 50.1 |
| 2011 | 63 | 64.8 | 62.4 | 48.4 |
| 2012 | 64.2 | 65.7 | 63 | 52 |
| 2013 | 65.0 | 66.5 | 63.9 | 53.1 |
2010 Achievable Benchmark: 70.7%.
Source: Centers for Medicare & Medicaid Services, Outcome and Assessment Information Set (OASIS), 2010-2013.
Denominator: Adult nonmaternity patients completing an episode of skilled home health care.
Notes: White and Black are non-Hispanic. Hispanic includes all races. Starting January 1, 2010, the patient assessment instrument for home health agencies was changed to OASIS-C.
- Importance: Shortness of breath interferes with activity and is an important health status indicator. It affects quality of life, ability to engage in a wide variety of activities, and patients' ability to care for themselves.
- Overall Rate: In 2013, 65% of home health care patients had less shortness of breath.
- Trend: From 2010 to 2013, the percentage of adult home health care patients whose episodes of shortness of breath decreased improved overall and for Blacks and Whites.
- Groups With Disparities:
- In all years, Hispanics were less likely than Whites to show improvement in shortness of breath. From 2010 to 2013, there was no statistically significant change in this disparity.
- Achievable Benchmark:
- The 2010 top 5 State achievable benchmark was 70.7%. The top 5 States that contributed to the achievable benchmark are District of Columbia, Hawaii, Maryland, New Jersey, and South Carolina.
- At the current rate, the overall rate could reach the benchmark in 6 years. All ages and racial/ethnic groups could reach the benchmark within 10 years except Hispanics, who show no progress toward the benchmark.
Slide 99
Moderate to Severe Pain Among Nursing Home Residents
- Pain management is a particularly important clinical concern for older adults residing in nursing homes.
- Poorly managed pain can decrease resident quality of life, reduce mobility and functional status, and increase loneliness and depression.1
Slide 100
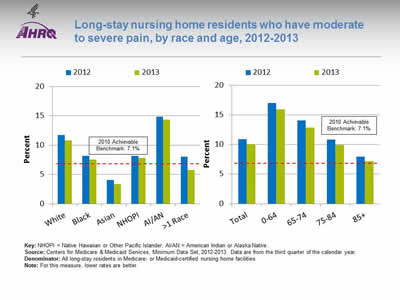
Long-stay nursing home residents who have moderate to severe pain, by race and age, 2012-2013
Image: Charts show long-stay nursing home residents who have moderate to severe pain, by race and age:
Left Chart:
| Race | 2012 | 2013 |
|---|---|---|
| White | 11.7 | 10.8 |
| Black | 8.2 | 7.5 |
| Asian | 4.1 | 3.4 |
| NHOPI | 8.2 | 7.8 |
| AI/AN | 14.9 | 14.3 |
| >1 Race | 8.0 | 5.7 |
Right Chart:
| Age | 2012 | 2013 |
|---|---|---|
| Total | 10.9 | 10.0 |
| 0-64 | 17.0 | 15.9 |
| 65-74 | 14.0 | 12.9 |
| 75-84 | 10.8 | 9.9 |
| 85+ | 8.0 | 7.2 |
2010 Achievable Benchmark: 7.1%.
Key: NHOPI = Native Hawaiian or Other Pacific Islander; AI/AN = American Indian or Alaska Native.
Source: Centers for Medicare & Medicaid Services, Minimum Data Set, 2012-2013. Data are from the third quarter of the calendar year.
Denominator: All long-stay residents in Medicare- or Medicaid-certified nursing home facilities.
Notes: For this measure, lower rates are better.
- Importance: Failure to identify the presence of pain or to assess its severity and functional impact can leave a potentially treatable symptom unrecognized and therefore unlikely to be addressed.
- Overall Rate: In 2013, 10.0% of nursing home residents had moderate to severe pain.
- Groups With Disparities:
- In 2012 and 2013, Blacks, Asians, Native Hawaiians and Other Pacific Islanders, and multiple-race residents were less likely than Whites to have moderate to severe pain.
- In both years, American Indians and Alaska Natives were more likely than Whites to have moderate to severe pain.
- In both years, residents ages 0-64, 65-74, and 75-84 were more likely than residents age 85 and over to have moderate to severe pain.
- Achievable Benchmark:
- The 2011 top 5 State achievable benchmark was 7.1%. The top 5 States that contributed to the achievable benchmark are District of Columbia, Hawaii, Maryland, New Jersey, and New York.
- Asians and multiple-race residents have achieved the benchmark.
Slide 101

Weight Loss Among Nursing Home Residents
- Unintentional weight loss is a common problem among nursing home residents.
- Weight loss is associated with adverse, costly clinical outcomes, including increased hospitalization, morbidity, and mortality.
- The Minimum Data Set defines clinically significant weight loss for nursing home residents:
- Weight loss ≥5% within a 30-day period or 10% within a 180-day period.
Slide 102
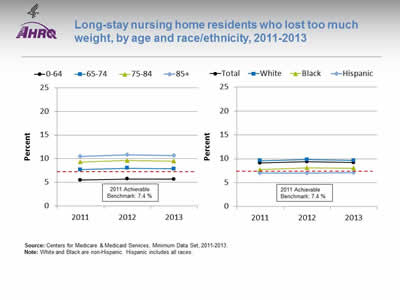
Long-stay nursing home residents who lost too much weight, by age and race/ethnicity, 2011-2013
Image: Charts show long-stay nursing home residents who lost too much weight, by age and race/ethnicity:
Left Chart:
| Year | 0-64 | 65-74 | 75-84 | 85+ |
|---|---|---|---|---|
| 2011 | 5.5 | 7.7 | 9.3 | 10.5 |
| 2012 | 5.7 | 8 | 9.6 | 10.8 |
| 2013 | 5.7 | 7.8 | 9.5 | 10.6 |
Right Chart:
| Year | Total | White | Black | Hispanic |
|---|---|---|---|---|
| 2011 | 9.1 | 9.6 | 7.7 | 7 |
| 2012 | 9.4 | 9.8 | 8.1 | 7 |
| 2013 | 9.2 | 9.6 | 8.0 | 7.1 |
2011 Achievable Benchmark: 7.4 %.
Source: Centers for Medicare & Medicaid Services, Minimum Data Set, 2011-2013.
Notes: White and Black are non-Hispanic. Hispanic includes all races.
- Importance: Nursing home residents with weight loss are at higher risk for functional decline, hip fracture, and death. Weight loss also may lead to muscle wasting, infections, and increased risk of pressure ulcers. Detecting and preventing weight loss is central to ensure appropriate nutritional intake.
- Overall Rate: The percentage of long-stay nursing home residents who lost too much weight was 9.2% in 2013.
- Groups With Disparities:
- From 2011 to 2013, the percentage of nursing home residents who lost too much weight was higher for people ages 65-74, 75-84, and 85 and over compared with those under age 64.
- In all years, the percentage of nursing home residents who lost too much weight was lower for Black and Hispanic residents compared with White residents.
- Achievable Benchmark:
- The 2011 top 6 State achievable benchmark was 7.4%. The top 6 States that contributed to the achievable benchmark are California, District of Columbia, Maryland, Massachusetts, New York, and Texas.
- Only nursing home residents ages 0-64 and Hispanics have achieved the benchmark.
Slide 103
References



