1. Enhancing Specialty Care and Surgical Service Lines
Strengthening subspecialized care and surgical service lines in rural hospitals is crucial for improving prompt diagnostic accuracy and reducing the need for patient transfers. By enhancing local subspecialist and surgical capabilities, rural hospitals can provide more comprehensive care and facilitate quicker diagnoses and treatments for conditions that require surgical intervention or specialized treatment plans. This goal can be achieved by addressing the following areas.
Accessing Care (Preventive, Acute, Specialty). Rural residents often face barriers to care such as transportation, financial limitations, and inability to connect with healthcare providers for early diagnosis and treatment, which begins with a primary care provider (PCP). However, as of 2024, 65 percent of all primary care health professional shortage areas (HPSAs) were in rural communities.37-39
Figure 1. U.S. primary care health professional shortage areas38
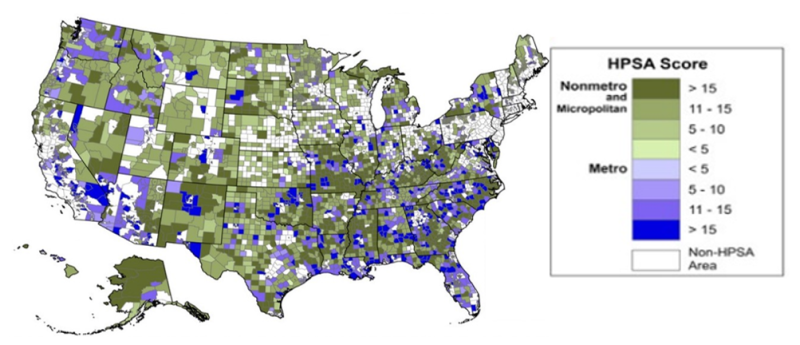
Source: data.HRSA.gov, Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services, July 2024.
Note: Alaska and Hawaii not to scale. HRSA scores HPSAs on a scale of a whole number (0-26 for primary care), with higher scores indicating greater need.
Given this shortage of primary caregivers, it is imperative to streamline care and maximize the value from each patient encounter. Rural organizations can ensure their physicians and advanced practice providers effectively use Healthcare Effectiveness Data and Information Set measures40 to attain high screening rates within patient care panels. Key performance metrics should be established and monitored to track the timely initiation of screenings, appropriate screening intervals, and timely follow-up on abnormal results.
When improving access to care, providers and organizations can move toward regionalization whenever possible.41 Deploying mobile care units for diagnostic testing (e.g., pulmonary testing, 3D mammography, mobile magnetic resonance imaging) can expand access to technology not immediately available in the rural community and improve diagnostic capabilities. Further, a community-based diagnostic hub-and-spoke model in partnership with other health organizations is another approach to help avoid significant financial outlay and provide easy access to diagnostic testing for rural residents.42,43
Integrating artificial intelligence (AI) is also becoming increasingly helpful in enhancing patient care in rural areas. AI algorithms can quickly analyze extensive data, including medical and family histories, demographics, and real-time health indicators. By leveraging these data, clinicians can quickly identify high-risk patients who need immediate attention, ensuring those with urgent needs are seen by specialist physicians without unnecessary delays. AI-driven prioritization optimizes resource allocation and improves overall patient outcomes by facilitating timely interventions.44 As regional healthcare systems continue to grapple with increasing patient volumes and complexity of care delivery, AI’s role in streamlining the referral process for patients in a rural setting becomes advantageous. Use of AI can foster a more efficient, equitable, and responsive healthcare environment.
Combining AI with telehealth models has been shown to improve outcomes for both patients and healthcare professionals in rural settings.45 This finding suggests that integrating these two approaches could significantly benefit rural communities by improving the timeliness and accuracy of diagnosis for high-risk patient screening.45 However, it is important to be mindful of AI’s potential to exacerbate existing disparities in healthcare, which necessitates careful implementation and monitoring to ensure equitable outcomes for all patients.
Training and Recruiting Specialists, Surgeons, and Surgical Staff. To ensure access to surgeons and surgical staff in rural communities, a multifaceted and intentional approach is needed. A 2017 study found that only 3 percent of final-year medical residents expressed an interest in practicing in communities of 25,000 people or smaller.46,47 Support of residency programs and fellowships designed specifically to train physicians and advanced practice providers for rural practice is an imperative.37,46
Rural hospitals can participate in hosting medical residents through various training programs, or partnering with a medical school to offer rural training experiences—essentially investing in the future of rural healthcare delivery. Programs such as the Targeted Rural Underserved Track Program,48,49 Rural Residency Planning and Development Program,50 and Rural Opportunities in Medical Education49 are excellent options. Among rural track graduates, 44 percent enter practice in a rural community, and physicians who completed more than half of their residency in rural areas chose to practice in rural areas at a significantly higher rate.51 Providing firsthand experience in rural communities remains a key strategy for engaging residents and should be actively pursued.52
In the interim, the American College of Surgeons Advisory Council for Surgery noted that a regional locum tenens solution (a common practice in rural and underserved areas where it is challenging to recruit medical staff) is an option. This approach involves hiring surgeons to cover for staff on leave, during high patient demand, or where shortages exist. It can ensure continuity of care from a few days to several months, providing additional support for rural communities to provide diagnostic procedural and surgical coverage.53-57 Further, satellite clinics can bring specialty-level diagnosis to places where rural residents would otherwise not have care, improving access to specialty medicine.58
For surgical and specialty care physicians, a commitment to lifelong learning is essential, and rural organizations can support ongoing education to expand the specialists’ ability to succeed. While urban physicians might experience routinization due to a high volume of repetitive procedures, rural community physicians and teams could display gaps in expertise due to low patient volume. Ongoing education and simulation training are practical ways to address these gaps and bolster experiential learning.24 Methods of e-learning can expand access to new care techniques for rural providers, such as video conferences with specialists from other locations, virtual patient computer-based simulation scenarios, and web-based learning. When diagnosis is accurate and timely, more complex patients can be transferred to urban facilities specializing in complex care, while rural facilities retain procedures they are equipped to handle. Ensuring that minimum case standards are developed by location, and competency is ensured, will foster high-quality specialty and surgical care. Implementing these models with a focus on diagnostic improvements may yield patient care advances in multiple specialty areas. Competency-based training in all specialties can ensure consistent care for patients regardless of their location, ultimately improving diagnostic outcomes.
Ensuring access to skilled surgical technologists and perioperative nurses is vital for increasing surgical specialists’ confidence in providing care in operating rooms. Using tools to validate perioperative skill sets and ensure ongoing continuing education for surgical staff is necessary to create a patient safety culture of diagnostic and surgical excellence.59 Such tools include Periop 10160 from the Association of periOperative Registered Nurses and Competency Based Orientation Programs61 from the American Society of PeriAnesthesia Nurses. These standardized training programs can help reduce variability in surgical training methods and create reliability in programmatic processes needed for safe patient care.
Establishing Tele-Specialty and Surgical Consultation Networks. In rural communities, the scarcity of specialists often limits access to specialty surgical care. One promising solution is the use of telehealth consultation networks, which combine remote specialty physicians with onsite advanced practice providers. This hybrid model enhances patient care while addressing the typical challenges associated with telehealth consultations.62,63 Rural hospitals can improve care access by partnering with nearby urban medical centers to provide remote surgical consultations and support, particularly when patient volumes do not justify a full-time specialist. A rotation of specialists in areas such as general surgery, cardiology, or obstetrics and gynecology can be arranged through partnerships, with the possibility of embedding specialty services within rural clinics to improve access to care.
Innovative solutions to accessing much-needed specialty care should be considered, such as developing telehealth hubs in rural communities to leverage specialists who choose to reside in or near these areas. Establishing telehealth agreements that allow these physicians to provide virtual care to other rural communities can help maintain a healthy practice volume and ensure sustainable compensation benefiting both the hospital and the specialist. However, this work is not without barriers. According to the Federal Communications Commission 2020 Broadband Deployment Report, nearly 25 percent of residents in rural areas lack broadband coverage.64 Limited broadband access can impede comprehensive physical examinations, affecting diagnostic accuracy, and highlights drawbacks in the current telehealth model. In regions with poor broadband access, integrating onsite specialty advanced practice providers with virtual or telephonic consultations from specialty physicians can improve the delivery of care. This model allows occasional surgical or interventional visits, minimizing travel demands on specialty physicians.
Investing in Advanced Surgical and Diagnostic Equipment and Technologies. Acquiring advanced diagnostic equipment can be challenging for rural facilities with limited operating margins. However, establishing funding pathways for this technology is crucial to improving diagnostic screening and surgical procedures.65 Evaluating emerging technologies (e.g., AI-powered colonoscopy tools) can improve screening with minimal investment and enhance the early detection of diseases.
Hospital and clinic administrators must be well versed in federal, state, and private funding opportunities. Training staff in grant writing is recommended to ensure that rural hospitals remain competitive in procuring advanced diagnostic technology. Applying for grants to acquire capital equipment (e.g., computed tomography machines, stress lab equipment, surgical robotics) can considerably enhance diagnostic capabilities.
Providing Access to Care to Hub Populations on State Lines. Many rural communities are located near state lines, presenting opportunities to recruit healthcare providers from neighboring states and provide equitable access to healthcare for patients closer to a healthcare facility in an adjacent state. Removing barriers to recruiting providers across states by adopting multistate Compact Licensure for Physicians, which would eliminate the need for multiple state licenses, would be valuable.66 Enabling physicians and advanced practice providers to practice across state lines within the Compact would enhance access to care for rural patients and encourage providers residing near state borders to explore adjacent opportunities.67 A similar initiative has been introduced through the U.S. Department of Health and Human Services’ License Portability Grant Program for Social Workers, which maintains quality standards while improving access to care.68 This model could be adapted to advance specialty and surgical care in rural communities as well.
2. Enhanced Care Coordination
Better care coordination is critical for advancing diagnosis by streamlining patient care, minimizing redundancies, and ensuring accurate and timely diagnoses. The presence of increased rural population-level comorbidities for chronic conditions (e.g., hypertension, diabetes, chronic obstructive pulmonary disease, and kidney disease) further complicates diagnosis,18 making care coordination among rural care settings and providers essential.69
Patient insurance status (whether underinsured or uninsured), health literacy, and transportation, among other factors, can also hinder how patients access the healthcare system. Individuals often rely on emergency departments for both major illnesses and nonemergent needs. Nationally, this use results in 136.3 million emergency department visits annually, with 17 percent (23 million) of these visits attributable to frequent users.70
Effective care coordination improves diagnostic accuracy and decreases healthcare costs by reducing unnecessary tests and preventing hospital readmissions affecting patients, providers, and insurers.69 In rural areas where healthcare resources are limited, efficient care coordination is essential for optimizing diagnostic care, reducing redundancies, and improving care efficiency, particularly when patients can be connected to the most appropriate location at the most appropriate time. This goal can be achieved through several key strategies in the following areas that enhance care delivery by promoting greater integration and collaboration.
Training and Support for Care Coordinators. Providing comprehensive training and ongoing support for care coordinators is crucial for equipping them with the skills and resources needed to manage patient care effectively.71 Care coordinators in rural settings navigate substantial barriers that inhibit patients’ access to care, such as arranging transportation to out-of-county specialists, identifying providers who accept patients’ insurance plans, and managing long wait times for appointments, scheduling of surgical interventions, and specialty care.69
To enhance their efficacy, care coordinators can be trained in areas including health information technology, patient communication strategies, and care coordination techniques.71,72 Enhancing support for care coordinators through access to professional networks, ongoing education, and real-time decision support tools can help to better address the complex needs of rural populations. By strengthening training and support frameworks, rural healthcare systems can more adeptly manage chronic conditions, improve diagnostic accuracy, and reduce reliance on emergency services.70 This approach also improves patient outcomes and leads to more cost-effective healthcare delivery.72
Improved Efficiency. Enhancing the efficiency of patient care by optimizing processes and reducing delays is critical for timely diagnoses; however, most rural care delivery entities are siloed. Practical strategies can focus on standardizing protocols, using telecommunication platforms, conducting joint training exercises, and forming collaborative consortia that involve regional clinics, primary care practices, and hospitals to improve care delivery.
Integrated Care Models. A 2020 CDC study found a 40 percent higher prevalence of heart disease among rural residents compared with their urban counterparts.73 To address this disparity and many similar health disparities for other chronic illnesses, developing integrated care models is essential to connect patients to a wide range of healthcare services to ensure comprehensive care. Integrated care models link patients to primary care for medication management, promote healthy lifestyles, and address social determinants of health, which can substantively decrease the risks of diseases.42,43,74 Technologies such as telehealth consultations, mobile health applications, and remote patient monitoring also play a role by identifying at-risk patients before they visit a PCP or an emergency department.75 Integrating these technologies into healthcare care coordination activities can improve diagnostic accuracy and timeliness.
Telehealth Use. Care coordination across telemedicine and telehealth networks can considerably improve patient access to personalized care across multiple providers. For example, many rural hospitals lack access to specialized medical expertise, but telemedicine networks, such as telestroke programs, enable quicker and more accurate diagnoses of critical conditions.76-78 These networks facilitate collaboration between rural hospitals and specialists, improving their ability to deliver a timely diagnosis and critical treatments.
A 2018 study examining telestroke adoption in 107 community hospitals found that hospitals that lack financial resources and capacity can pool resources needed for acquiring essential technology.76 The use of telestroke networks allows rural hospitals to collaborate with neurologists, enhancing their ability to administer life-saving clot-dissolving drugs during strokes.78 This approach could be expanded to other high-priority diagnostic areas, such as cardiology and oncology, where specialist shortages also exist. Telehealth can improve patient outcomes through timely access to care, while local and regional resources are optimized, reducing the overall cost burden on both the healthcare system and patients.
3. Social Determinants of Health: Screenings and Referrals
The presence of unaddressed social determinants of health (i.e., food, employment, housing, education) that patients experience can lead to significant diagnostic challenges and increase health disparities.79,80 For example, cultural and language barriers or low health literacy can prevent patients from accurately describing their symptoms or medical history, leading to misdiagnosis.81 Similarly, poverty may prevent patients from accessing care, leading to delayed diagnoses, or adhering to medication regimes (e.g., filling/refilling prescriptions, managing polypharmacy).81,82
Healthcare plays a vital role in population health, and 10-20 percent of SDOH have modifiable contributors that healthcare delivery can assist in addressing.79,83 Once a patient’s social needs have been identified, a plan to address those needs should be in place. A provider (e.g., clinician, hospital) does not have to meet the social need; it could be as simple as providing patients with a list of organizations that can assist with identified social needs. Whether the protocol is providing a list, making personalized referrals, or providing the service themselves (e.g., providing public transportation vouchers, occasional late business hours, flexible billing), it should be streamlined and easy for both the clinicians, staff, and patients to act. Rural hospitals, clinics, and physicians can join existing community partnerships, or form new partnerships, to prioritize, develop, and implement SDOH interventions and define their roles in this endeavor.84
To achieve diagnostic excellence in rural healthcare, action to identify and address a wider spectrum of factors influencing patients’ health and access to care is imperative, and this need cannot be excised from healthcare delivery. Some actionable steps to help address patient SDOH in rural settings include the following areas.
Using Standardized SDOH Screening Tools. Screening for SDOH is critical in identifying and addressing the nonmedical factors that significantly impact health outcomes in rural communities.25,85 Integrating SDOH screening into routine patient care helps healthcare providers understand the broader context of a patient’s health, enabling more precise and personalized care and diagnoses. Effective screening protocols are crucial for identifying and reducing diagnostic errors by addressing factors contributing to misdiagnosis or delayed treatment. Implementing the consistent use of one of many tested SDOH screening protocols is an immediate step healthcare clinicians can take to improve diagnostic care in rural settings.25,26,29,74,85
Connecting Patients With Community Resources. Establishing strong referral networks with community resources that can address modifiable SDOH factors is another immediately actionable area. Once unmet social needs are identified, it is crucial to connect patients with local resources and services to address these needs.29 An essential first step is meeting with relevant community-based organizations so they are aware that patients may be referred. Community-based organizations can support patients with housing, nutrition, insurance eligibility, and employment support, which can ultimately improve their health outcomes and health-related quality of life.26,29
Training Healthcare Staff. Educating healthcare staff on the importance of SDOH and how to integrate this understanding into patient care is vital. Training programs for staff focused on using standardized protocols and developing the skills and sensitivity to identify barriers related to SDOH can contribute to a lower risk of systemic diagnostic errors.4,86,87
Enhancing Community Engagement. Strengthening community engagement is integral to addressing SDOH effectively. Implementing SDOH interventions, such as health education campaigns to raise awareness of health-related outcomes and prevention strategies, community health literacy programs, patient engagement in their healthcare, and fostering of patient-centeredness, are all powerful methods to reduce disparities in health and healthcare.4,86,87
By actively involving the community in preventive care initiatives and health management activities, healthcare providers can enhance awareness of prevalent health issues within the population and promote the adoption of proactive health behaviors.88 This engagement helps bridge the gap between healthcare services and the community by better equipping patients to manage their health, ultimately leading to more timely and accurate diagnosis. This endeavor also facilitates a closer alignment between healthcare services and the community, empowering patients to manage their health more effectively, which in turn contributes to timelier and more accurate diagnoses.



