"Sometimes it is not enough for the doctor to just say "lose weight"; sometimes you have to be shown how to do it."
Rural Community Focus Group Member
A Case Study: Ms. Smith
Ms. Smith, a middle aged mother of two that you've cared for over the past 15 years, is waiting in the exam room for a medication check-up. She's pre-diabetic, hypertensive, and about 45 pounds overweight, but otherwise healthy. You've helped Ms. Smith manage her hypertension with medication over the past 3 years and have warned her about the gradual increase in her laboratory blood sugar levels means. You've even tried a little motivational interviewing to see if you could help Ms. Smith think about improving her diet—but she says she's too busy right now working full time at the school, raising two kids, and caring for her mother who has mild dementia.
You think that many of Ms. Smith's health issues could be resolved if she were to focus on improving her diet, engaging in regular exercise, and returning to a healthier weight. However, you also realize the sensitive nature of the discussion about obesity. Before entering the exam room you quickly review her medical record. You note that only hypertension is present in the problem list so you add pre-diabetes. You see Ms. Smith was weighed today, but no height was taken and BMI was not calculated. However, your "eyeball test" tells you that Ms. Smith is obese. Just before you knock on the exam door your medical assistant reminds you that you are running behind schedule. You address the main reason for the visit with Ms. Smith (medication check-up) and move on to the next patient.
What didn't happen? There was no discussion of diet and nutrition as part of Ms. Smith's visit—despite the clinician's interest and the patient's need. National data indicates that conversations around diet and nutrition occur in only 12.2% of visits, and only 8.5% about exercise and 3.7% for weight reduction.3 This is a missed opportunity to help patients make lifestyles changes that may prevent development of chronic disease and improve management of multiple existing conditions.
Why didn't it happen? There are many reasons why primary care clinicians and staff may not address obesity, exercise, diet, or nutrition during the clinical encounter. Some may include:
- Not having enough time during the encounter.
- Inadequate reimbursement for health behavior change counseling.
- Thinking that you won't have an effect on patient behavior.
- Lacking ready solutions to help the patient.
- Fearing that the discussion may lead your patient to seek care from another clinician/clinic.
- Perhaps you, like 60% of American adults, are overweight or obese.
What Can Your Practice Do?
Primary care is well positioned to coordinate care by identifying patients who need to make health behavior changes (such as around weight management, dietary habits, or physical activity), offering brief counseling, and referring to more intensive counseling and support resources as needed. There is growing evidence that making a referral to community-based resources dedicated to the treatment and management of overweight and obesity may help. This toolkit is designed to help you bridge this gap between primary care and community-based resources.
Theoretical Framework for Building Clinic and Community Resource Bridges
Etz and colleagues (2009) created the model for bridging the gap between primary care clinics and community-based resources for health behavior change based on findings from the Robert Wood Johnson Foundation Prescription for Health Initiative.4 Effective linkages (i.e., bridging) requires foundational characteristics in the clinic as well as in the community-based resources—or what Etz and colleagues called "anchors." Once you've built the anchors, you can construct the "deck" of the bridge, which represents the connecting strategies. Figure 2 summarizes these critical bridging components.
Figure 2. Bridging Primary Care and Community Resources: Model Elements (Reproduced with permission from Etz et al., 2008)
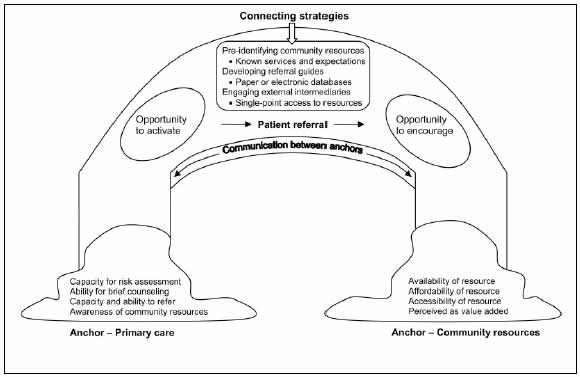
This toolkit elaborates on the Etz et al., (2008) model by describing the blueprint our team used to build bridges between rural primary care clinics and community-based resources for obesity management. Throughout this toolkit we present both simple designs and more complex approaches—but all are just sample blueprints. Many types of bridges can be built with different materials or designs, and you will need to determine the model that works best for your unique clinic and community context. For example the Brooklyn Bridge, Golden Gate Bridge, and a small bridge crossing a creek all achieve the same goal but have different external structures.
A community focus group member said: "Sometimes it's not enough to tell someone [to lose weight]; sometimes you have to be shown how to do it." The same is true with building clinic/community linkages. You have the inspiration—now let's allocate resources and put in the work!



