Appendix A. PubMed Search Criteria
Common Search Criteria for Cost
|
Common Search Criteria for Cost ("Costs and Cost Analysis"[mh] OR "Cost of Illness"[mh] OR "Economics"[mh] OR "Health Care Costs"[mh] OR "Direct Service Costs"[mh] OR "Hospital Costs"[mh] OR "Health Expenditures"[mh] OR cost[tiab] OR costs[tiab] OR expenditure*[tiab] OR expense[tiab] OR spend*[tiab] OR "financial outcome"[tiab] OR "financial outcomes"[tiab] OR "financial impact"[tiab] OR "financial impacts"[tiab] OR "economic impact"[tiab] OR "economic impacts"[tiab] OR "economic outcome"[tiab] OR "economic outcomes"[tiab]) AND (incremental[tiab] OR additional[tiab] OR extra[tiab] OR attribut*[tiab] OR excess[tiab] OR "compared to"[tiab] OR "compared with"[tiab] OR "associated with"[tiab] OR "because of"[tiab] OR "due to"[tiab] OR "caused by"[tiab]) AND (hospital*[tiab] OR inpatient[tiab] OR "Hospital Costs"[mh] OR "intensive care unit"[tiab]) NOT "cost effectiveness"[ti] |
|
Common Search Criteria for Mortality "Mortality"[mh] OR "Hospital mortality"[mh] OR mortalit*[tiab] OR death*[tiab] OR fatalit*[tiab]) AND (additional[tiab] OR extra[tiab] OR attribut*[tiab] OR excess[tiab] OR "compared to"[tiab] OR "compared with"[tiab] OR "associated with"[tiab] OR "because of"[tiab] OR "due to"[tiab] OR "caused by"[tiab] |
|
Common Exclusions English[lang] AND United States[pl] AND (2000:2017[dp] |
|
Adverse Drug Events (("Drug therapy/adverse effects"[mh] OR "drug interactions"[mh] OR "anaphylaxis"[mh] OR "drug overdose"[mh] OR "Drug-related side effects and adverse reactions"[mh] OR "adverse drug event"[tiab] OR "adverse drug events"[tiab] OR "adverse drug reaction"[tiab] OR "adverse drug reactions"[tiab] OR "medication errors"[mh] OR "medication error"[tiab] OR "medication errors"[tiab] OR adverse [tiab] OR "allergic reaction"[tiab] OR "allergic reactions"[tiab] OR "anaphylaxis"[tiab] OR overdose[tiab] OR ((drug[tiab] OR medication[tiab]) AND (harm[tiab] OR injury[tiab]))) AND (("anticoagulants"[mh] OR "anticoagulation"[tiab] OR "anticoagulant"[tiab] OR "4- Hydroxycoumarins"[mh] OR "Acenocoumarol"[mh] OR "Ancrod"[mh] OR "Antithrombin III"[mh] OR "Antithrombin Proteins"[mh] OR "Beta 2-Glycoprotein I"[mh] OR "Blood Coagulation Factor Inhibitors"[mh] OR "Citric Acid"[mh] OR "Dabigatran"[mh] OR "Dalteparin"[mh] OR "Dermatan Sulfate"[mh] OR "Dextrans"[mh] OR "Dicumarol"[mh] OR "Edetic Acid"[mh] OR "Enoxaparin"[mh] OR "Ethyl Biscoumacetate"[mh] OR "Fibrin Fibrinogen Degradation Products"[mh] OR "Gabexate"[mh] OR "Heparin"[mh] OR "Heparin Cofactor II"[mh] OR "Heparin, Low-Molecular-Weight"[mh] OR "Heparinoids"[mh] OR "Hirudins"[mh] OR "Nadroparin"[mh] OR "Pentosan Sulfuric Polyester"[mh] OR "Phenindione"[mh] OR "Phenprocoumon"[mh] OR "Protein C"[mh] OR "Protein S"[mh] OR "Rivaroxaban"[mh] OR "Warfarin"[mh] OR "Hirudin Therapy"[mh]) OR ("analgesics, opioid"[mh] OR opioid*[tiab] OR "Alfentanil"[mh] OR "Alphaprodine"[mh] OR "Buprenorphine"[mh] OR "Buprenorphine, Naloxone Drug Combination"[mh] OR "Butorphanol"[mh] OR "Codeine"[mh] OR "Dextromoramide"[mh] OR "Dextropropoxyphene"[mh] OR "Dihydromorphine"[mh] OR "Diphenoxylate"[mh] OR "Enkephalin, Ala(2)-MePhe(4)-Gly(5)- "[mh] OR "Enkephalin, D- Penicillamine (2,5)- "[mh] OR "Ethylketocyclazocine"[mh] OR "Ethylmorphine"[mh] OR "Etorphine"[mh] OR "Fentanyl"[mh] OR "Heroin"[mh] OR "Hydrocodone"[mh] OR "Hydromorphone"[mh] OR "Levorphanol"[mh] OR "Meperidine"[mh] OR "Meptazinol"[mh] OR "Methadone"[mh] OR "Methadyl Acetate"[mh] OR "Morphine"[mh] OR "Nalbuphine"[mh] OR "Opiate Alkaloids"[mh] OR "Opium"[mh] OR "Oxycodone"[mh] OR "Oxymorphone"[mh] OR "Pentazocine"[mh] OR "Phenazocine"[mh] OR "Phenoperidine"[mh] OR "Pirinitramide"[mh] OR "Promedol"[mh] OR "Sufentanil"[mh] OR "Tilidine"[mh] OR "Tramadol"[mh])) AND ("iatrogenic disease"[mh] OR "nosocomial"[tiab] OR "healthcare associated"[tiab] OR "health care associated"[tiab] OR "hospital acquired"[tiab] OR "inpatient"[tiab] OR "hospitalized"[tiab] OR "hospital related"[tiab] OR "in hospital"[tiab] OR "in hospitals"[tiab] OR "within hospitals"[tiab])) |
|
CAUTI ((("urinary tract infections"[mh] OR "urinary tract infection*"[tiab]) AND (Urinary catheterization[mh] OR urinary catheter*[tiab] OR "catheter associated"[tiab])) OR ("catheter-related infections"[mh] AND "urinary"[tiab]) OR (Urinary Catheterization/adverse effects*[mh) OR "CAUTI"[tiab] OR (("cross infection"[mh] OR "iatrogenic disease"[mh] OR "nosocomial"[tiab] OR "hospital infection"[tiab] OR "hospital infections"[tiab] OR "healthcare associated"[tiab] OR "health care associated"[tiab] OR "hospital acquired"[tiab] OR "hospital related"[tiab]) AND "urinary"[tiab])) |
|
CLABSI ((("catheter-related"[tiab] OR "catheter-associated"[tiab] OR "Catheterization, Central Venous/adverse effects"[Mesh] OR "Central Venous Catheters/adverse effects"[mh] OR "Catheters, Indwelling/adverse effects"[mh] OR "umbilical catheter"[tiab] OR central line*[tiab] OR central venous catheter*[tiab]) AND ("bloodstream infection"[tiab] OR "bloodstream infections"[tiab] OR "blood stream infection"[tiab] OR "blood stream infections"[tiab] OR "bacteremia"[tiab] OR "bacteremia"[mh] OR ((Cross infection[mh] OR "cross infection"[tiab] OR "cross infections"[tiab] OR nosocomial[tiab] OR "hospital-acquired infection"[tiab] OR "hospital-acquired infections"[tiab] OR "healthcare-associated infection"[tiab] OR "healthcare-associated infections"[tiab] OR "health care-associated infection"[tiab] OR "health care-associated infections"[tiab]) AND ("bloodstream"[tiab] OR "blood stream"[tiab])))) OR CLABSI[tiab] OR CRBSI[tiab] OR CABSI[tiab] OR CLAB[tiab] OR ("catheter-related infections"[mh] AND ("blood stream"[tiab] OR "bloodstream"[tiab]))) |
|
Falls ("Accidental Falls" [mh] OR Falls [tiab] OR Falling [tiab] OR Fall [tiab] OR "Accidental Falls" [tiab] OR "Accidental Fall" [tiab] OR Slip [tiab] OR Faller [tiab]) AND (hospital*[tiab] OR inpatient*[tiab] OR "Hospital Costs"[mh] OR "intensive care unit"[tiab] OR "acute care setting"[tiab] OR "hospitalization"[mh] OR "inpatients"[mh] OR "Intensive Care Units"[Mesh]) |
|
Obstetric Adverse Events ("Inferior Wall Myocardial Infarction"[Mesh] OR "Anterior Wall Myocardial Infarction"[Mesh] OR "Acute Kidney Injury"[Mesh] OR "Respiratory Distress Syndrome, Adult"[Mesh] OR "Embolism, Amniotic Fluid"[Mesh] OR "Aneurysm"[Mesh] OR "Heart Arrest"[Mesh] OR "Ventricular Fibrillation"[Mesh] OR "Disseminated Intravascular Coagulation"[Mesh] OR "Heart Failure"[Mesh] OR "Head Injuries, Closed"[Mesh] OR "Craniocerebral Trauma"[Mesh] OR "Cerebrovascular Trauma"[Mesh] OR "Cerebrovascular Disorders"[Mesh] OR "Pulmonary Edema"[Mesh] OR "Anesthesia, Obstetrical/adverse effects"[Mesh] OR "Anesthesia, Obstetrical/complications"[Mesh] OR "Sepsis"[Mesh] OR "Shock"[Mesh] OR "Anemia, Sickle Cell/complications"[Mesh] OR "Thrombosis/complications"[Mesh] OR "Blood Transfusion"[Mesh] OR "Defibrillators"[Mesh] OR "Interactive Ventilatory Support"[Mesh]) |
|
Pressure Ulcers (("Pressure Ulcer" [MeSH] OR "Pressure Ulcer" [tiab] OR "Bedsore" [tiab] OR "Bed Sores" [tiab] OR "Decubitus Ulcer" [tiab] OR "Pressure Sore" [MeSH] OR "Pressure Sore" [tiab] OR "Suspected Deep Tissue Injury" [tiab] OR "Pressure Ulcer" [MeSH] OR "Pressure Ulcer" [tiab] OR "osteomyelitis" [MeSH] OR "osteomyelitis" [tiab] OR "tunneling" [tiab] OR "fissure" [tiab]) AND ("hospital acquired" [tiab] OR "healthcare acquired" [tiab] OR "nosocomial" [tiab] OR "hospitalization" [MeSH] OR "hospitalized"[tiab] OR "healthcare associated"[tiab] OR "health care associated"[tiab] OR "health care acquired"[tiab] OR "hospital related"[tiab] OR "inpatient"[tiab] OR "in hospital"[tiab] OR "in hospitals"[tiab] OR "within hospitals"[tiab)) |
|
Venous Thromboembolism (("pulmonary embolism/economics"[MeSH Terms]) OR ("Upper Extremity Deep Vein Thrombosis"[MeSH Terms]) OR ("venous thromboembolism/economics"[MeSH Terms]) OR ("venous thrombosis/economics"[MeSH Terms]) OR ("Pulmonary Infarction"[Mesh]) OR (("deep venous"[tiab] OR "deep vein"[tiab] OR "pulmonary"[tiab]) AND (thrombos*[tiab] OR embolism*[tiab] OR thromboembolism*[tiab]))) AND ("iatrogenic disease"[mh] OR "nosocomial"[tiab] OR "healthcare associated"[tiab] OR "health care associated"[tiab] OR "hospital acquired"[tiab] OR "inpatient"[tiab] OR "hospitalized patients"[tiab] OR "hospital related"[tiab] OR "in hospital"[tiab] OR "in hospitals"[tiab] OR "within hospitals"[tiab]) |
|
Surgical Site Infections ("cross infection"[mh] OR "hospital acquired" [tiab] OR "healthcare acquired" [tiab] OR "nosocomial" [tiab] OR "hospitalized"[tiab] OR "healthcare associated"[tiab] OR "hospital associated"[tiab] OR "health care associated"[tiab] OR "health care acquired"[tiab] OR "hospital related"[tiab] OR "inpatient"[tiab] OR "in hospital"[tiab] OR "in hospitals"[tiab] OR "within hospitals"[tiab]) AND ("surgical wound infection/economics"[mh] OR "surgical procedures, operative/adverse effects"[mh] OR ("surgical wound infection"[mh] AND prognosis[mh]) OR (("surgical wound infection*"[tiab] OR "surgical site infection*"[tiab]) AND outcome*[tiab])) |
|
Ventilator Associated Pneumonia (("Pneumonia, Ventilator-Associated/economics"[mh]) OR ("Ventilator Associated Pneumonia"[tiab] OR "Ventilator-Associated Pneumonia"[tiab] OR "Ventilators, Mechanical/adverse effects"[mh]) OR (("Respiration, Artificial/economics"[mh] OR "Artifical respiration"[tiab]) AND (mechanically ventilat*[tiab] OR mechanical ventilat*[tiab] OR intubat*[tiab] OR ventilator associated*[tiab])) AND ("cross infection"[mh] OR "iatrogenic disease"[mh] OR "hospital acquired" [tiab] OR "healthcare acquired" [tiab] OR "nosocomial" [tiab] OR "healthcare associated"[tiab] OR "hospital associated"[tiab] OR "health care associated"[tiab] OR "health care acquired"[tiab] OR "hospital related"[tiab] OR "inpatient"[tiab] OR "in hospital"[tiab] OR "in hospitals"[tiab])) |
|
Clostridium difficile Infections (("Clostridium difficile" [Mesh] OR "Clostridium difficile*" [tiab] OR "C diff"[tiab] OR "Colitis" [Mesh] OR "Colitis" [tiab] OR CDAD[tiab]) AND("cross infection" [Mesh] OR "bacteremia" [Mesh] OR "iatrogenic disease"[MeSH] OR "nosocomial"[tiab] OR "healthcare associated"[tiab] OR "health care associated"[tiab] OR "hospital acquired"[tiab] OR "hospital infection*"[tiab] OR "inpatient"[tiab])) |
Appendix B. Excess Mortality Calculations
We define excess mortality as an estimate of additional deaths due to the hospital-acquired condition (HAC). These are expressed as the percentage of HAC cases who die as a result of the HAC.
Calculation: 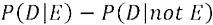
Where P(D|E) indicates the probability of death in those with HAC and P(D|not E) indicates the probability of death in those at risk for, but do not acquire, the HAC.
| Died | Alive | |
|---|---|---|
| HAC group | a | b |
| Non-HAC group | c | d |
Meta-analysis Method for Estimating Excess Mortality
We calculate the pooled relative risk using meta-analysis and then calculate excess mortality using the pooled RR and an estimate of the underlying mortality rate:
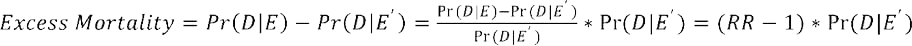
where RR =  represents the underlying mortality in patients at risk for the HAC.
represents the underlying mortality in patients at risk for the HAC.
When the underlying mortality was not available from other literature, we used an estimate of the general inpatient mortality rate. This rate, 2 percent, can be thought of as the overall mortality rate among all hospitalized patients, HAC and non-HAC patients. This rate was used for falls and VTE. For all other HACs, the underlying mortality rate was drawn from the published literature. Exhibit B1 shows the underlying mortality rates and a description of the underlying population alongside the meta-analysis-based estimates of excess mortality.
Exhibit B1. Underlying Mortality Rates
| HAC | Underlying Population Description | Underlying Mortality Rate | RR (range) | Pooled RR (95% CI) | Excess Mortality Estimate (95% CI) |
|---|---|---|---|---|---|
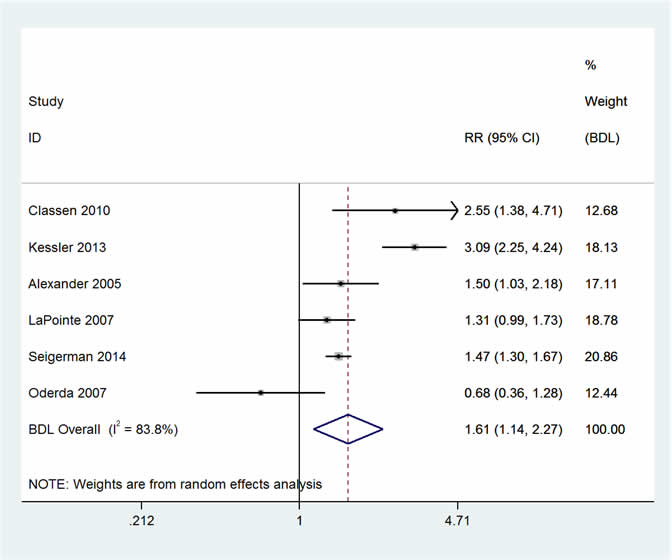
| ADE | Hospitalized patients who are given anticoagulants, hypoglycemic agents, and opioids during hospitalization | 0.02a | 0.68–3.09 | 1.61 (1.14, 2.27) | 0.012 (0.003–0.025) |
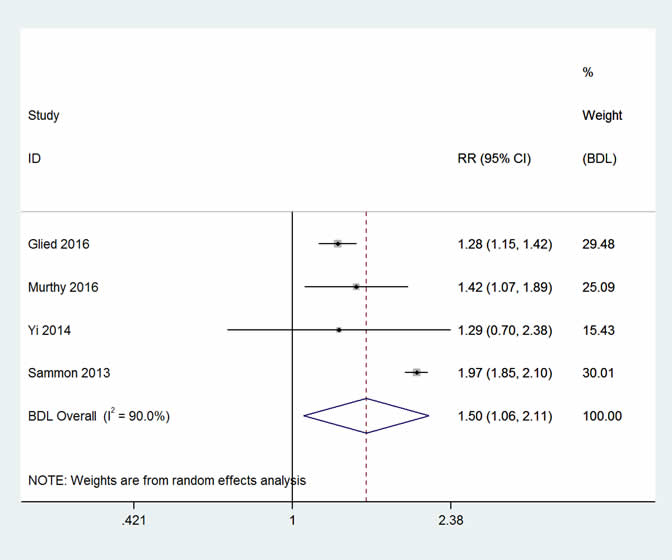
| CAUTI | Hospitalized patients with urinary catheters | 0.071b | 1.28–1.97 | 1.50 (1.06, 2.11) | 0.036 (0.004–0.079) |
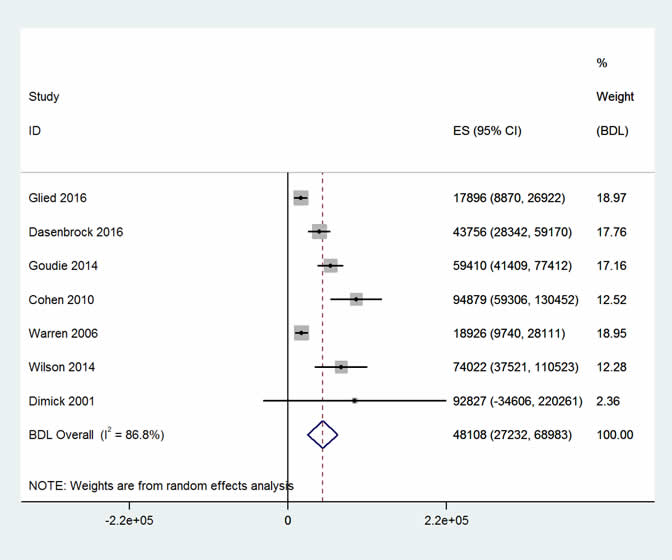
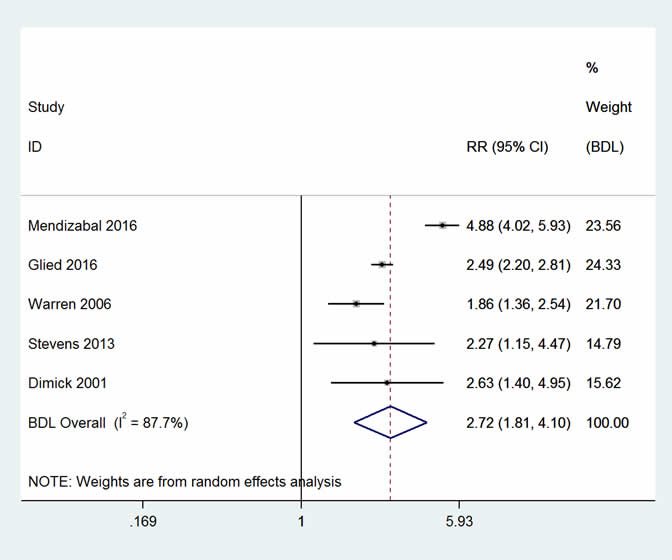
| CLABSI | Hospitalized patients with central lines | 0.086b | 1.86–4.88 | 2.72 (1.81, 4.10) | 0.15 (0.070–0.27) |
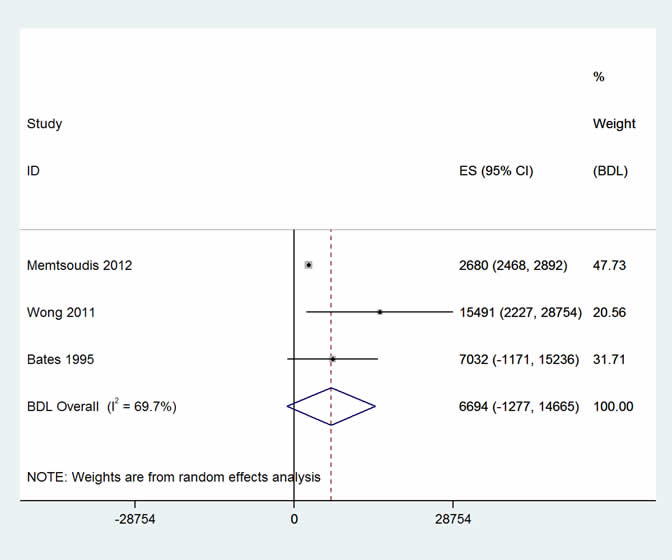
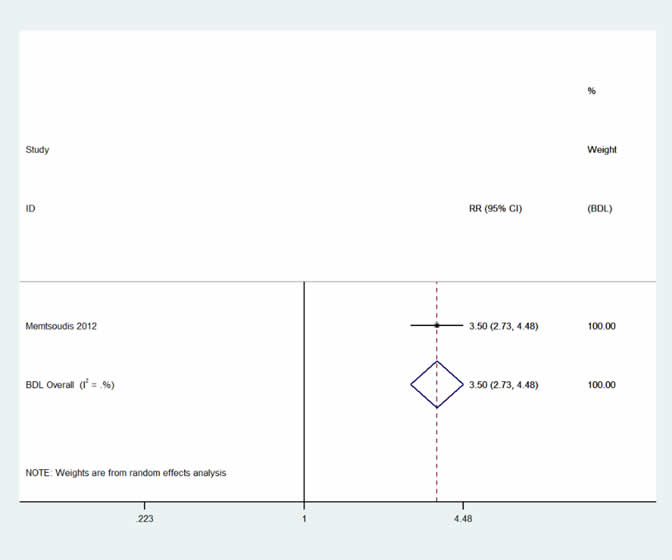
| Falls | All hospitalized patients who are at risk to fall in the hospital | 0.02a | 3.50 | 3.50 (2.73, 4.48) | 0.050 (0.035–0.070) |
| OBAE | Estimate was not based on RR and underlying mortality; please see report for details | 0.0049 (0.0030–0.013) | |||
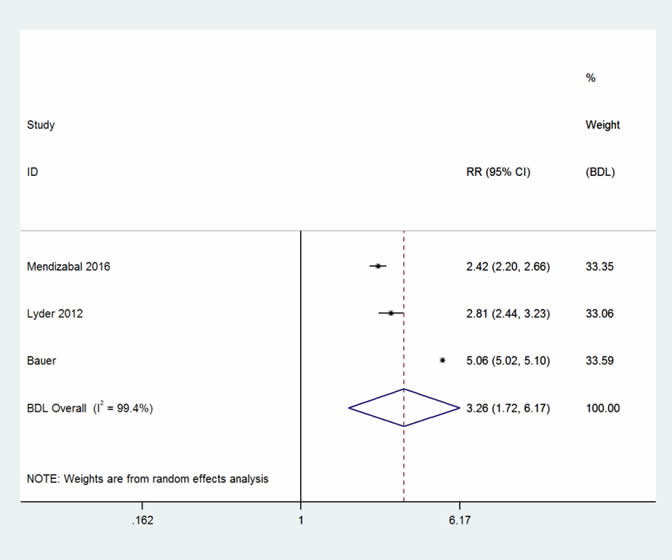
| Pressure Ulcer | All hospitalized patients who are at risk to have pressure ulcer | 0.018c | 2.42–5.06 | 3.26 (1.71, 6.17) | 0.041 (0.013–0.093) |
| SSI | All hospitalized postsurgical patients | 0.0114d | 1.75–5.70 | 3.32 (1.79, 6.18) | 0.026 (0.009–0.059) |
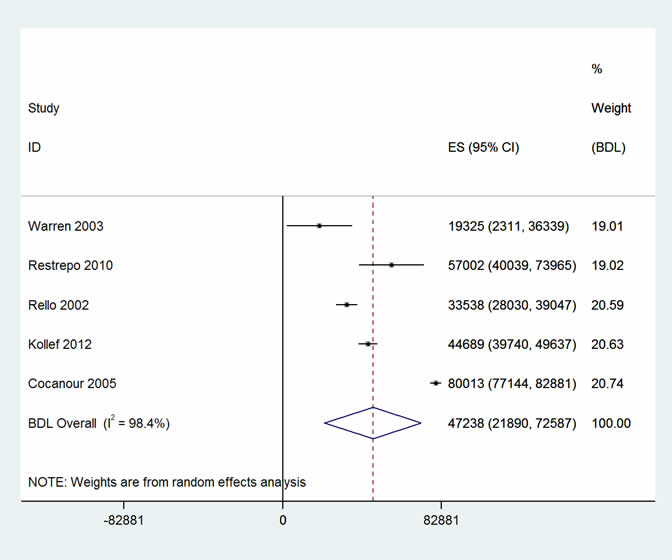
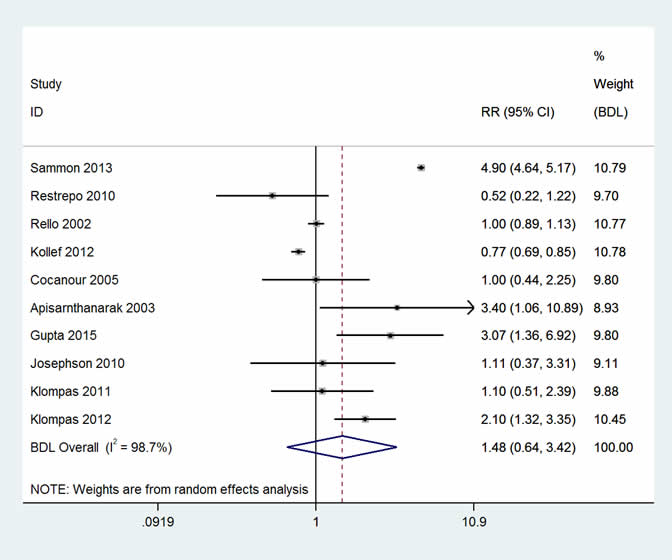
| VAP | Hospitalized patients with ventilator | 0.3e | 0.52–4.90 | 1.48 (0.64, 3.42) | 0.14 (-0.11–0.73) |
| VTE | All hospitalized patients who are at risk to get VTE | 0.02a | 1.01–13.63 | 3.15 (2.02, 4.91) | 0.043 (0.040–0.078) |
| CDI | All hospitalized patients who are at risk to get CDI | 0.073f | 1.17–9.60 | 1.60 (1.38, 1.87) | 0.044 (0.028–0.064) |
a Hall MJ, Levant S, DeFrances CJ. Trends in Inpatient Hospital Deaths: National Hospital Discharge Survey, 2000–2010 NCHS Data Brief, No. 118. Hyattsville, MD: National Center for Health Statistics; 2013.
b Glied S, Cohen B, Liu J, et al. Trends in mortality, length of stay, and hospital charges associated with health care–associated infections, 2006-2012. Amer J Inf Cont. 2016 Sep 1;44(9):983-9.
c Bauer K, Rock K, Nazzal M, et al. Pressure ulcers in the United States' inpatient population from 2008 to 2012: results of a retrospective nationwide study. Ostomy/wound Mgmt. 2016 Nov;62(11):30.
d Weiser TG, Semel ME, Simon AE, et al. In-hospital death following inpatient surgical procedures in the United States, 1996–2006. Wrld J of Surg. 2011 Sep 1;35(9):1950-6.
e Kahn JM, Goss CH, Heagerty PJ, et al. Hospital volume and the outcomes of mechanical ventilation. New Eng J of Med. 2006 Jul 6;355(1):41-50.
f Pakyz A, Carroll NV, Harpe SE, et al. Economic impact of Clostridium difficile infection in a multihospital cohort of academic health centers. Pharmacotherapy. 2011 Jun 1;31(6):546-51.
Appendix C. Meta-Analysis Citation List
Alexander KP. Excess dosing of antiplatelet and antithrombin agents in the treatment of non–ST-segment elevation acute coronary syndromes. JAMA. 2005 Dec;294(24):1-9.
Ali M, Ananthakrishnan AN, McGinley EL, et al. Deep vein thrombosis and pulmonary embolism in hospitalized patients with cirrhosis: a nationwide analysis. Dig Dis Sci. 2011 Jul;56(7):2152-9.
Apisarnthanarak A, Holzmann-Pazgal G, Hamvas A, et al. Ventilator-associated pneumonia in extremely preterm neonates in a neonatal intensive care unit: characteristics, risk factors, and outcomes. Pediatrics. 2003 Dec;112(6 Pt 1):1283-9.
Bates DW, Pruess K, Souney P, et al. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med. 1995 Aug 1;99(2):137-43.
Bauer K, Rock K, Nazzal M, et al. Pressure ulcers in the United States’ inpatient population from 2008 to 2012: results of a retrospective nationwide study. Ostomy Wound Manage. 2016 Nov;62(11):30-8.
Boltz MM, Hollenbeak CS, Julian KG, et al. Hospital costs associated with surgical site infections in general and vascular surgery patients. Surgery. 2011 Nov;150(5):934-42.
Byrn JC, Brooks MK, Belding-Schmitt M, et al. Impact of urinary tract infection definitions on colorectal outcomes. J Surg Res. 2015 Dec;199(2):331-7.
Callaghan WM, MacKay AP, Berg CJ. Identification of severe maternal morbidity during delivery hospitalizations, United States, 1991-2003. Am J Obstet Gynecol. 2008 Aug 31;199(2):133-e1.
Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012 Nov;120(5):1029-36.
Classen DC, Jaser L, Budnitz DS. Adverse drug events among hospitalized Medicare patients: epidemiology and national estimates from a new approach to surveillance. Jt Comm J Qual Patient Saf. 2010 Jan;36(1):12-21.
Cocanour CS, Ostrosky-Zeichner L, Peninger M, et al. Cost of a ventilator-associated pneumonia in a shock trauma intensive care unit. Surg Infect (Larchmt). 2005;6(1):65-72.
Cohen ER, Feinglass J, Barsuk JH, et al. Cost savings from reduced catheter-related bloodstream infection after simulation-based education for residents in a medical intensive care unit. Simul Healthc. 2010 Apr 1;5(2):98-102.
Creanga AA, Bateman BT, Mhyre JM, et al. Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol. 2014 Dec;211(6):647.e1-16.
Damle RN, Cherng NB, Flahive JM, et al. Clostridium difficile infection after colorectal surgery: a rare but costly complication. J Gastrointest Surg. 2014 Oct;18(10):1804-11.
Dasenbrock HH, Rudy RF, Smith TR, et al. Hospital-acquired infections after aneurysmal subarachnoid hemorrhage: a nationwide analysis. World Neurosurg. 2016 Apr;88:459-74.
de Lissovoy G, Fraeman K, Hutchins V, et al. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009 Jun;37(5):387-97.
Dimick JB, Pelz RK, Consunji R, et al. Increased resource use associated with catheter-related bloodstream infection in the surgical intensive care unit. Arch Surg. 2001 Feb;136(2):229-34.
Donnelly JP, Wang HE, Locke JE, et al. Hospital-onset Clostridium difficile infection among solid organ transplant recipients. Am J Transplant. 2015 Nov;15(11):2970-7.
Eagye KJ, Nicolau DP, Kuti JL. Impact of superinfection on hospital length of stay and costs in patients with ventilator-associated pneumonia. Semin Respir Crit Care Med. 2009 Feb;30(1):116-23.
Flagg A, Koch CG, Schiltz N, et al. Analysis of Clostridium difficile infections after cardiac surgery: epidemiologic and economic implications from national data. J Thorac Cardiovasc Surg. 2014 Nov;148(5):2404-9.
Gephart MGH, Zygourakis CC, Arrigo RT, et al. Venous thromboembolism after thoracic/thoracolumbar spinal fusion. World Neurosurg. 2012 Nov;78(5):545-52.
Glance LG, Stone PW, Mukamel DB, et al. Increases in mortality, length of stay, and cost associated with hospital-acquired infections in trauma patients. Arch Surg. 2011 Jul;146(7):794-801.
Glied S, Cohen B, Liu J, et al. Trends in mortality, length of stay, and hospital charges associated with health care-associated infections, 2006-2012. Am J Infect Control. 2016 Sep;44(9):983-9.
Goudie A, Dynan L, Brady PW, et al. Attributable cost and length of stay for central line-associated bloodstream infections. Pediatrics. 2014 Jun;133(6):e1525-32.
Goudie A, Dynan L, Brady PW, et al. Costs of venous thromboembolism, catheter-associated urinary tract infection, and pressure ulcer. Pediatrics. 2015 Sep 1;136(3):432-9.
Grobman WA, Bailit JL, Rice MM, et al. Frequency of and factors associated with severe maternal morbidity. Obstet Gynecol. 2014 Apr;123(4):804-10.
Gupta S, Boville BM, Blanton R, et al. A multicentered prospective analysis of diagnosis, risk factors, and outcomes associated with pediatric ventilator-associated pneumonia. Pediatr Crit Care Med. 2015 Mar;16(3):e65-73.
Hennessey P, Semenov YR, Gourin CG. The effect of deep venous thrombosis on short-term outcomes and cost of care after head and neck cancer surgery. Laryngoscope. 2012 Oct;122(10):2199-204.
Hunt TD, Guglielminotti J, Li G. Costs associated with anesthesia-related adverse events during labor and delivery in New York state, 2010. Anesth Analg. 2016 Jun;122(6):2007-16.
Josephson SA, Moheet AM, Gropper MA, et al. Ventilator-associated pneumonia in a neurologic intensive care unit does not lead to increased mortality. Neurocrit Care. 2010 Apr;12(2):155-8.
Keshavamurthy S, Koch CG, Fraser TG, et al. Clostridium difficile infection after cardiac surgery: prevalence, morbidity, mortality, and resource utilization. J Thorac Cardiovasc Surg. 2014 Dec;148(6):3155-7.
Kessler ER, Shah M, Gruschkus SK, et al. Cost and quality implications of opioid-based postsurgical pain control using administrative claims data from a large health system: opioid-related adverse events and their impact on clinical and economic outcomes. Pharmacotherapy. 2013 Apr;33(4):383-91.
Kilgore ML, Ghosh K, Beavers CM, et al. The costs of nosocomial infections. Med Care. 2008 Jan 1;46(1):101-4.
Kim SP, Shah ND, Karnes RJ, et al. The implications of hospital acquired adverse events on mortality, length of stay and costs for patients undergoing radical cystectomy for bladder cancer. J Urol. 2012 Jun;187(6):2011-7.
Klompas M, Khan Y, Kleinman K, et al. Multicenter evaluation of a novel surveillance paradigm for complications of mechanical ventilation. PLoS One. 2011 Mar;6(3):e18062.
Klompas M, Magill S, Robicsek A, et al. Objective surveillance definitions for ventilator-associated pneumonia. Crit Care Med. 2012 Dec;40(12):3154-61.
Kollef MH, Hamilton CW, Ernst FR. Economic impact of ventilator-associated pneumonia in a large matched cohort. Infect Control Hosp Epidemiol. 2012 Mar;33(3):250-6.
Lagu T, Stefan MS, Haessler S, et al. The impact of hospital-onset Clostridium difficile infection on outcomes of hospitalized patients with sepsis. J Hosp Med. 2014 Jul;9(7):411-7.
LaPointe NMA, Chen AY, Alexander KP, et al. Enoxaparin dosing and associated risk of in-hospital bleeding and death in patients with non ST-segment elevation acute coronary syndromes. Arch Intern Med. 2007 Jul;167(14):1539-44.
Lemaire A, Dombrovskiy V, Batsides G, et al. The effect of Clostridium difficile infection on cardiac surgery outcomes. Surg Infect (Larchmt). 2015 Feb;16(1):24-8.
Lesperance K, Causey MW, Spencer M, et al. The morbidity of Clostridium difficile infection after elective colonic resection-results from a national population database. Am J Surg. 2011 Feb;201(2):141-8.
Luo R, Greenberg A, Stone CD. Outcomes of Clostridium difficile infection in hospitalized leukemia patients: a nationwide analysis. Infect Control Hosp Epidemiol. 2015 Jul;36(7):794-801.
Lyder CH, Wang Y, Metersky M, et al. Hospital-acquired pressure ulcers: results from the national Medicare Patient Safety Monitoring System study. J Am Geriatr Soc. 2012 Sep;60(9):1603-8.
Memtsoudis SG, Dy CJ, Ma Y, et al. In-hospital patient falls after total joint arthroplasty: incidence, demographics, and risk factors in the United States. J of Arthroplasty. 2012 Jun 30;27(6):823-8.
Mendizabal A, Thibault DP, Willis AW. Patient safety events in hospital care of individuals with epilepsy. Epilepsia. 2016 Aug;57(8):1301-9.
Murthy SB, Moradiya Y, Shah J, et al. Nosocomial infections and outcomes after intracerebral hemorrhage: a population-based study. Neurocrit Care. 2016 Oct;25(2):178-84.
Nguyen GC, Sam J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008 Sep;103(9):2272-80.
O’Brien JA, Lahue BJ, Caro JJ, et al. The emerging infectious challenge of clostridium difficile-associated disease in Massachusetts hospitals: clinical and economic consequences. Infect Control Hosp Epidemiol. 2007 Nov;28(11):1219-27.
Oderda GM, Said Q, Evans RS, et al. Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Annals of Pharmacotherapy. 2007 Mar 1;41(3):400-7.
Pakyz A, Carroll NV, Harpe SE, et al. Economic impact of Clostridium difficile infection in a multihospital cohort of academic health centers. Pharmacotherapy. 2011 Jun;31(6):546-51.
Rello J, Ollendorf DA, Oster G, et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large U.S. database. Chest. 2002 Dec;122(6):2115-21.
Restrepo MI, Anzueto A, Arroliga AC, et al. Economic burden of ventilator-associated pneumonia based on total resource utilization. Infect Control Hosp Epidemiol. 2010 May;31(5):509-15.
Sammon J, Trinh VQ, Ravi P, Sukumar S, et al. Health care-associated infections after major cancer surgery. Cancer. 2013 Jun 15;119(12):2317-24.
Satahoo SS, Parikh PP, Naranjo D, et al. Are burn patients really at risk for thrombotic events? J Burn Care Res. 2015;36(1):100-4.
Seigerman M, Cavallaro P, Itagaki S, et al. Incidence and outcomes of heparin-induced thrombocytopenia in patients undergoing cardiac surgery in North America: an analysis of the nationwide inpatient sample. J Cardiothorac Vasc Anesth. 2014 Feb;28(1):98-102.
Skovrlj B, Guzman JZ, Silvestre J, et al. Clostridium difficile colitis in patients undergoing lumbar spine surgery. Spine (Phila Pa 1976). 2014 Sep;39(19):E1167-73.
Spector WD, Limcangco R, Owens PL, et al. Marginal hospital cost of surgery-related hospital-acquired pressure ulcers. Med care. 2016 Sep 1;54(9):845-51.
Stevens V, Geiger K, Concannon C, et al. Inpatient costs, mortality and 30-day re-admission in patients with central-line-associated bloodstream infections. Clin Microbiol Infect. 2014 May 1;20(5):O318-24.
Suh DC, Woodall BS, Shin SK, et al. Clinical and economic impact of adverse drug reactions in hospitalized patients. Ann Pharmacother. 2000 Dec;34(12):1373-9.
Sundaram V, May FP, Manne V, et al. Effects of Clostridium difficile infection in patients with alcoholic hepatitis. Clin Gastroenterol Hepatol. 2014 Oct;12(10):1745–52.e2.
Tabak YP, Zilberberg MD, Johannes RS, et al. Attributable burden of hospital-onset Clostridium difficile infection: a propensity score matching study. Infect Control Hosp Epidemiol. 2013 Jun;34(6):588-96.
Trinh VQ, Karakiewicz PI, Sammon J, et al. Venous thromboembolism after major cancer surgery: temporal trends and patterns of care. JAMA Surg. 2014 Jan;149(1):43–9.
Warren DK, Shukla SJ, Olsen MA, et al. Outcome and attributable cost of ventilator-associated pneumonia among intensive care unit patients in a suburban medical center. Crit Care Med. 2003 May;31(5):1312-7.
Warren DK, Quadir WW, Hollenbeak CS, et al. Attributable cost of catheter-associated bloodstream infections among intensive care patients in a nonteaching hospital. Crit Care Med. 2006 Aug;34(8):2084-9.
Wilson MZ, Rafferty C, Deeter D, et al. Attributable costs of central line-associated bloodstream infections in a pediatric hematology/oncology population. Am J Infect Control. 2014 Nov;42(11):1157-60.
Wong CA, Recktenwald AJ, Jones ML, et al. The cost of serious fall-related injuries at three Midwestern hospitals. Joint Com J Qual Patiet Saf. 2011 Feb 28;37(2):81-7.
Wu H, Nguyen GC. Liver cirrhosis is associated with venous thromboembolism among hospitalized patients in a nationwide U.S. study. Clin Gastroenterol Hepatol. 2010 Sep;8(9):800-5.
Yi SH, Baggs J, Gould CV, et al. Medicare reimbursement attributable to catheter-associated urinary tract infection in the inpatient setting: a retrospective cohort analysis. Med Care. 2014 Jun;52(6):469-78.
Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003 Oct;290(14):1868-74.
Appendix D. Key Study Characteristics
Exhibit D1. Adverse Drug Events
| Kessler (2013) | Oderda (2007) | Suh (2000) | Classen (2010) | Alexander (2005) | LaPointe (2007) | Seigerman (2014) | ||
|---|---|---|---|---|---|---|---|---|
| Study | Study Year | 2009-2010 | 1990-1999 | 1998 | 2004 | 2004 | 2005 | 2009-2010 |
| Population | Patients with a primary surgical procedure | Adult surgical patients ( >17 y) in a single Utah hospital |
All patient (≥2 y) admissions to a single New York hospital | Medicare beneficiaries | Patients with NSTE ACS | Patients with NSTE ACS | Patients with cardiac surgery | |
| Study Design | Retrospective cohort | Matched cohort | Retrospective matched control | Retrospective cohort | Prospective observational | Prospective observational | Retrospective cohort | |
| Data Source(s) | Hospital administrative data | Hospital clinical and surveillance data | Hospital pharmacy and medical record reporting systems | MPSMS | CRUSADE National Quality Improvement Initiative Registry | CRUSADE National Quality Improvement Initiative Registry | HCUP-NIS | |
| Number of Cases | 4,537 | 1,586 | 131 | 172 | 22,480g | 13,803 | 560 | |
| Definition of HAC | ICD-9 | Hospital surveillance criteria and Noranjo criteria | WHO | Medication-specific algorithms | Recommended dosing categories | Recommended dosing categories | Non-specified diagnosis | |
| Cost | Cost or Charges Reported | Cost | Cost | Cost | ||||
| Attributable | Y | Y | Y | |||||
| Year of Cost Data | Not specified | Not specified | Not specified | |||||
| Mean Attributable Cost Calculated | $6,721.00 | $786.00 | $5,483.00 | |||||
| Standard Error | $347.54 | $151.79 | $1,959.00 | |||||
| Mortality | Matched Control Sample | Y | Y | N | N | N | N | |
| Adjusted RR/OR | 3.39 (2.42–4.74) | Not reported | Not used in analysis | 1.50 (1.03-2.17) | 1.31 (0.99-1.73) | 1.47 (1.30-1.67) | ||
| SE(logRR)/SE(logOR) | 0.161 | 0.321 | 0.314 | 0.190 | 0.142 | 0.064 |
g Represents the number of instances of a major bleed in the presence of drug therapy administration; some patients received more than one drug therapy.
Exhibit D2. Catheter-Associated Urinary Tract Infection
| Glied (2016) | Yi (2014) | Byrn (2015) | Dasenbrock (2016) | Goudie (2015) | Sammon (2013) | Murthy (2016) | ||
|---|---|---|---|---|---|---|---|---|
|
Study |
Study Year | 2006-2012 | 2009 | 2006-2012 | 2008-2011 | 2009-2011 | 1999-2009 | 2002-2011 |
| Population | All patients, New York City hospital network | Medicare beneficiaries with ESRD | Patients with colorectal resection | Patients with aneurysmal subarachnoid hemorrhage | Patients 1-17 years of age | Patients with any of 8 surgical oncology procedures | Patients with nontraumatic intracerebral hemorrhage | |
| Study Design | Matched retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | Matched retrospective cohort | Retrospective | Retrospective cohort | |
| Data Source(s) | Hospital clinical and administrative data | MedPAR, Beneficiary Annual Summary File | University hospital database | HCUP-NIS | HCUP-NIS | HCUP-NIS | HCUP-NIS | |
| Number of Cases | 8,048 | 884 | 18 | 1,793 | 1,513 | 105,113 | 40,018 | |
| Definition of HAC | Lab results and ICD-9 | CDC-NHSN | NHSN; NSQIP; ICD-9 | ICD-9 | ICD-9 | ICD-9 | ICD-9 | |
| Cost | Cost or Charges Reported | Charges | Payment | Cost | Charges | Cost | ||
| Attributable | Y | Y | N | N | Y | |||
| Year of Cost Data | 2012 | 2009 | 2012 | 2011h | 2011 | |||
| Mean Attributable Cost Calculated | $20,857.50 | $5,877.13 | $11,587.10 | $27,858.50 | $7,200.00 | |||
| Standard Error | $2,365.07 | $1,644.05 | $5,531.84 | $2,164.43 | $2,538.82 | |||
| Mortality | Matched Control Sample | Y | Y | N | N | |||
| Adjusted RR/OR | 1.28 | 1.37 (1.04-1.80) ICU; 1.17 (0.62-2.23) non-ICU |
1.97 (1.85-2.10) | 1.42 (1.10-1.94) | ||||
| SE(logRR)/SE(logOR) | 0.054 | 0.311 | 0.032 | 0.145 |
h The year of cost data is not specified; the last year of the study period was used for the purpose of this analysis.
Exhibit D2. Catheter-Associated Urinary Tract Infection continued
| Kilgore (2008) | ||
|---|---|---|
| Study | Study Year | 2001-2006 |
| Population | All hospitalized patients | |
| Study Design | Retrospective cohort | |
| Data Source(s) | Cardinal Health MedMined database | |
| Number of Cases | 18,930 | |
| Definition of HAC | Lab results | |
|
Cost |
Cost or Charges Reported | Cost |
| Attributable | Y | |
| Year of Cost Data | 2007 | |
| Mean Attributable Cost Calculated | $3,936.00 | |
| Standard Error | $1,961.26 | |
|
Mortality |
Matched Control Sample | |
| Adjusted RR/OR | ||
| SE(logRR)/SE(logOR) |
Exhibit D3. Central-Line Associated Bloodstream Infections
|
|
Dimick (2001) | Glied (2016) | Warren (2006) | Cohen (2010) | Dasenbrock (2016) | Goudie (2014) | Wilson (2014) | |
|---|---|---|---|---|---|---|---|---|
| Study | Study Year | 1998-1999 | 2006-2012 | 1998-2000 | 2006-2007 | 2008-2011 | 2008-2011 | 2008-2011 |
| Population | Surgical ICU patients in single Maryland hospital | All patients, New York City hospital network | All ICU patients, suburban St. Louis Missouri hospital | All ICU patients,single Chicago-area hospital | Patients with aneurysmal subarachnoid hemorrhage | Patients under 18 years of age | Pediatric hematology and oncology patients in Mid-Atlantic hospital | |
| Study Design | Prospective cohort | Matched retrospective cohort | Prospective cohort | Case-control | Retrospective cohort | Matched case-control | Matched prospective cohort | |
| Data Source(s) | Hospital administrative data | Patients’ electronic medical record and other digital sources | Hospital clinical and administrative data | Hospital administrative data | HCUP-NIS | HCUP-NIS | Hospital clinical and administrative data | |
| Number of Cases | 9 | 3,603 | 41 | 12 | 77 | 1,339 | 60 | |
| Definition of HAC | Catheter colonization | Lab results and ICD-9 | CDC-NHSN | ICD-9 | ICD-9 | AHRQ PQI | Lab results | |
|
Cost |
Cost or Charges Reported | Cost | Charges | Cost | Cost | Charges | Cost | Cost |
| Attributable | Y | Y | Y | Y | N | Y | Y | |
| Year of Cost Data | 1998 | 2012 | 2000 | 2008 | 2011i | 2011 | 2011j | |
| Mean Attributable Cost Calculated | $56,167.00 | $17,197.00 | $11,971.00 | $82,005.00 | $40,983.42 | $55,646.00 | $69,332.00 | |
| Standard Error | $39,340.52 | $4,425.38 | $2,964.34 | $15,687.02 | $7,366.13 | $8,602.71 | $17,443.43 | |
| Mortality | Matched Control Sample | N | Y | N |
|
|||
| Adjusted RR/OR | 4.3 (0.9-19.9) | 2.49 | Not reported |
|
||||
| SE(logRR)/SE(logOR) | 0.322 | 0.063 | 0.160 |
i The year of cost data is not specified; the last year of the study period was used for the purpose of this analysis.
j The year of cost data is not specified; the last year of the study period was used for the purpose of this analysis.
Exhibit D3. Central-Line Associated Bloodstream Infections continued
| Mendizabal (2016) | Sammon (2013) | Stevens (2014) | ||
|---|---|---|---|---|
| Study | Study Year | 2000-2010 | 1999-2009 | 2008-2010 |
| Population | Adult patients with epilepsy | Patients with any of 8 surgical oncology procedures | All patients, single tertiary-care hospital | |
| Study Design | Retrospective cohort | Retrospective | Retrospective cohort | |
| Data Source(s) | HCUP-NIS | HCUP-NIS | Hospital clinical and administrative data | |
| Number of Cases | Not reported | 47,551 | 197 | |
| Definition of HAC | AHRQ PSI | ICD-9 | CDC-NHSN | |
|
Cost |
Cost or Charges Reported | |||
| Attributable | ||||
| Year of Cost Data | ||||
| Mean Attributable Cost Calculated | ||||
| Standard Error | ||||
|
Mortality |
Matched Control Sample | N | N | N |
| Adjusted RR/OR | 4.88 (4.02-5.93) | 17.29 (16.33-18.31) | 2.27 (1.15-4.46) | |
| SE(logRR)/SE(logOR) | 0.099 | 0.015 | 0.346 |
Exhibit D4. Falls
| Memtsoudis (2012) | Bates (1995) | Wong (2011) | ||
|---|---|---|---|---|
| Study | Study Year | 1998-2007 | 1987-1991 | 2004-2006 |
| Population | Postoperative hip and knee surgery patients | All patients in a single Massachusetts hospital | Adult inpatients in 3 Midwest hospitals | |
| Study Design | Retrospective cohort | Retrospective case-control | Retrospective case-control | |
| Data Source(s) | HCUP-NIS | Hospital clinical data | Hospital incident reporting system | |
| Number of Cases | 9,198 | 62 | 57 | |
| Definition of HAC | ICD-9 | Patient reported as having fallen | Serious fall-related injury | |
|
Cost |
Cost or Charges Reported | Cost | Charges | Cost |
| Attributable | N | Y | Y | |
| Year of Cost Data | 2007k | 1991l | 2009 | |
| Mean Attributable Cost Calculated | $2,247 | $3,802 | $13,806 | |
| Standard Error | $90.57 | $2,262.97 | $6,031.23 | |
|
Mortality |
Matched Control Sample | N | ||
| Adjusted RR/OR | Not reported | |||
| SE(logRR)/SE(logOR) | 0.126 |
k The year of cost data is not specified; the last year of the study period was used for the purpose of this analysis.
l The year of cost data is not specified; the last year of the study period was used for the purpose of this analysis.
Exhibit D5. Obstetric Adverse Events
| Zhan (2003) | Hunt (2016) | Callaghan (2008) | Callaghan (2012) | Creanga (2014) | Grobman (2014) | ||
|---|---|---|---|---|---|---|---|
| Study | Study Year | 2000 | 2010 | 1991-2003 | 1998-2009 | 2008-2010 | 2008-2011 |
| Population | Women with delivery-related discharge | Women with delivery-related discharge in New York | Women with delivery-related discharges | Women with delivery-related discharges | Women with delivery-related discharges in 7-state sample | Women who delivered ≥23 weeks gestations in any of 25 cohort hospitals | |
| Study Design | Retrospective cohort | Retrospective cohort | Retrospective | Retrospective | Retrospective | Retrospective cohort | |
| Data Source(s) | HCUP-NIS | State-level inpatient database | National Hospital Discharge Survey | HCUP-NIS | HCUP-NIS | Eunice Kennedy Shriver National Institute of Child Health & Human Development Maternal-Fetal Medicine Units Network cohort | |
| Number of Cases | 64,879 | 1,053 | 257,000 | 597,920 | 74,720 | 332 | |
| Definition of HAC | AHRQ PSI | ICD-9 | ICD-9 | ICD-9 | ICD-9 | Geller et al. (2004) morbidity scoring system | |
| Cost | Cost or Charges Reported | Charges | Cost | ||||
| Attributable | Y | Y | |||||
| Year of Cost Data | 2000 | 2010 | |||||
| Mean Attributable Cost Calculated | $8.35 | $1,091.34 | |||||
| Standard Error | $28.344 | $30.20 | |||||
| Mortality | Matched Control Sample | N | N | N | N | ||
| Adjusted RR/OR | Alternative estimation method used | Alternative estimation method used | Alternative estimation method used | Alternative estimation method used | |||
| SE(logRR)/SE(logOR) | - | - | - | - |
Exhibit D6. Pressure Ulcers
| Bauer (2016) | Spector (2016) | Goudie (2015) | Zhan (2003) | Mendizabal (2016) | Lyder (2012) | ||
|---|---|---|---|---|---|---|---|
| Study |
Study Year |
2008-2012 | 2011–2012 | 2009-2011 | 2000 | 2000-2010 | 2006-2007 |
| Population | General hospitalized patients | Adult patients with surgery | Patients 1-17 years of age | General hospitalized patients | Adult patients with epilepsy | Medicare beneficiary FFS sample | |
| Study Design | Retrospective | Matched retrospective cohort | Matched retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective | |
| Data Source(s) | HCUP-NIS | HCUP-SID and MPSMS | HCUP-NIS | HCUP-NIS | HCUP-NIS | MPSMS | |
| Number of Cases | 676,435 | 534 | 120 | 843 | Not reported | 2,313 | |
| Definition of HAC | ICD-9 | MPSMS chart review | ICD-9 | ICD-9 | AHRQ PSI | ICD-9 | |
| Cost | Cost or Charges Reported | Charges | Cost | Cost | Charges | ||
| Attributable | N | Y | Y | Y | |||
| Year of Cost Data | Not specified | 2011 | 2011 | 2000 |
|
||
| Mean Attributable Cost Calculated | $19,900.00 | $8,251.00 | $19,740.00 |
$5,422.50 |
|
||
| Standard Error |
$149.72 |
$11,553.78 |
$11,553.78 |
$184.00 |
|
||
| Mortality | Matched Control Sample | N | N | N | |||
| Adjusted RR/OR | Not reported |
2.42 (2.20-2.66) |
2.81 (2.44-3.23) | ||||
| SE(logRR)/SE(logOR) | 0.004 |
0.048 |
0.072 |
Exhibit D7. Surgical Site Infections
| Glied (2016) | Kim (2012) | Boltz (2011) | de Lissovoy (2009) | Eagye (2009) | Sammon (2013) | ||
|---|---|---|---|---|---|---|---|
| Study | Study Year | 2006-2012 | 2001-2008 | 2007-2009 | 2005 | 2005-2007 | 1999-2009 |
| Population | All patients, New York City hospital network | Adults undergoing radical cystectomy for bladder cancer | Adult general and vascular surgical patients in single hospital | Surgical patients | Patients with ECS procedures in single Connecticut hospital | Patients with any of 8 surgical oncology procedures | |
| Study Design | Matched retrospective cohort | Retrospective cohort | Retrospective cohort | Matched retrospective cohort | Prospective cohort and case-control | Retrospective | |
| Data Source(s) | Patients’ electronic medical record and other digital sources | HCUP-NIS | Hospital clinical data | HCUP-NIS | Hospital administrative data | HCUP-NIS | |
| Number of Cases | 1,292 | 381 | 186 | 6,891 | 46 | 80,086 | |
| Definition of HAC | Lab results and ICD-9 | ICD-9 | NSQIP; CDC NNIS | ICD-9 | ICD-9 | ICD-9 | |
| Cost | Cost or Charges Reported | Charges | Cost | Cost | Cost | Cost | |
| Attributable | Y | N | Y | Y | N | ||
| Year of Cost Data | 2012 | 2008 | Not specified | 2005 | Not specified | ||
| Mean Attributable Cost Calculated | $34,813.00 | $36,454.00 | $10,497.00 | $20,842.00 | $21,228.07 | ||
| Standard Error | $7,274.19 | $2,530.06 | $3,532.46 | $971.19 | $3,844.11 | ||
| Mortality | Matched Control Sample | Y | N | N | |||
| Adjusted RR/OR | Not reported | 5.70 (3.94–8.24) | 3.78 (3.56-4.02) | ||||
| SE(logRR)/SE(logOR) | 0.129 | 0.188 | 0.031 |
Exhibit D8. Venous Thromboembolism
| Hennessey (2012) | Kim (2012) | Goudie (2015) | Ali (2011) | Gephart (2012) | Mendizabal (2016) | Nguyen (2008) | ||
|---|---|---|---|---|---|---|---|---|
|
Study |
Study Year | 2003-2008 | 2001-2008 | 2009-2011 | 2005 | 2002-2008 | 2000-2010 | 1998-2004 |
| Population | Patients with head or neck cancers | Adults undergoing radical cystectomy for bladder cancer | Patients 1-17 years of age | Patients with cirrhosis | Adult patients with thoracic/thoraco-lumbar spinal fusion | Adult patients with epilepsy | Patients with inflammatory bowel disease | |
| Study Design | Retrospective cohort | Retrospective case control | Matched retrospective cohort | Retrospective cross sectional | Retrospective cohort | Retrospective cohort | Retrospective cohort | |
| Data Source(s) | HCUP-NIS | HCUP-NIS | HCUP-NIS | HCUP-NIS | HCUP-NIS | HCUP-NIS | HCUP-NIS | |
| Number of Cases | 1,860 | 219 | 1,563 | 8,231 | 162 | Not reported | 1,934 | |
| Definition of HAC | ICD-9 | ICD-9 | ICD-9 | ICD-9 | ICD-9 | AHRQ PSI | ICD-9 | |
| Cost | Cost or Charges Reported | Cost | Cost | Cost | ||||
| Attributable | Y | N | Y | |||||
| Year of Cost Data | 2011 | 2008 | 2011 | |||||
| Mean Attributable Cost Calculated | $10,313.28 | $27,387 | $27,686.00 | |||||
| Standard Error | $1,159.73 | $3,024.31 | $8,443.52 | |||||
| Mortality | Matched Control Sample | N | N | N | N | N | N | |
| Adjusted RR/OR | 3.08 (1.56 – 6.12) | 5.85 (3.61 – 9.48) | 1.01 (0.83, 1.23) | 13.63 (6.37-29.16) | 3.09 (2.64-3.62) | 2.50 (1.83 – 3.43) | ||
| SE(logRR)/SE(logOR) | 0.349 | 0.246 | 0.100 | 0.388 | 0.081 | 0.160 |
Exhibit D8. Venous Thromboembolism continued
| Satahoo (2015) | Trinh (2014) | Wu (2010) | ||
|---|---|---|---|---|
| Study | Study Year | 2005-2009 | 1999-2009 | 1998-2006 |
| Population | Patients with burn injuries | Patients with major cancer surgery | Patients with liver cirrhosis | |
| Study Design | Retrospective cohort | Retrospective cohort | Retrospective cohort | |
| Data Source(s) | HCUP-NIS | HCUP-NIS | HCUP-NIS | |
| Number of Cases | 297 | 33,409 | Not reported | |
| Definition of HAC | ICD-9 | ICD-9 | ICD-9 | |
|
Cost |
Cost or Charges Reported | |||
| Attributable | ||||
| Year of Cost Data | ||||
| Mean Attributable Cost Calculated | ||||
| Standard Error | ||||
| Mortality | Matched Control Sample | N | N | N |
| Adjusted RR/OR | 1.88 (1.147 – 3.075) | 5.30 (4.88 – 5.76) | 2.30 (2.06 – 2.57) | |
| SE(logRR)/SE(logOR) | 0.252 | 0.042 | 0.056 |
Exhibit D9. Ventilator-Associated Pneumonia
| Cocanour (2005) | Kollef (2012) | Rello (2002) | Restrepo (2010) | Warren (2003) | Apisarnthanarak (2003) | Gupta (2015) | ||
|---|---|---|---|---|---|---|---|---|
| Study | Study Year | 2002-2003 | 2008-2009 | 1998-1999 | 2002-2006 | 1998-1999 | 2000-2001 | 2009 |
| Population | ICU patients with shock trauma in a single Texas tertiary-care hospital | Adults ICU patents, ≥1 day in ICU with mechanical ventilation ≥2 days | All patients admitted to ICU who received mechanical ventilation for >24h | Hospitalized patients in 54 medical centers, nationwide | All patients admitted to ICU in a single Missouri medical center | Extremely pre-term neonates in Missouri hospital | Mechanically ventilated patients <18 y across 16 geographically diverse PICUs | |
| Study Design | Matched retrospective cohort | Matched retrospective cohort | Matched retrospective cohort | Matched retrospective cohort | Prospective cohort | Prospective and nested cohort | Prospective cohort | |
| Data Source(s) | Hospital administrative data | Premier Healthcare Informatics Database | MediQual Profile database | NASCENT study | Hospital clinical and administrative data | Hospital clinical data | Hospital CXR | |
| Number of Cases | 93 | 2,144 | 816 | 30 | 127 | 19 | 108 | |
| Definition of HAC | NNIS guideline | ICD-9 | ICD-9 | ICD-9 and lab results | NNIS criteria | CDC-NNIS | CDC-NHSN | |
| Cost | Cost or Charges Reported | Cost | Cost | Charges | Cost | Cost | ||
| Attributable | Y | Y | N | N | Y | |||
| Year of Cost Data | 2003 | 2009 | 1999 | 2005 | 1999 | |||
| Mean Attributable Cost Calculated | $57,158.00 | $39,828.00 | $20,647.00 | $44,331.50 | $11,897.00 | |||
| Standard Error | $1,045.59 | $2,250.00 | $1,730.21 | $6,731.00 | $5,344.23 | |||
|
Mortality |
Matched Control Sample | Y | Y | Y | Y | Y | N | |
| Adjusted RR/OR | Not reported | Not reported | Not reported | Not reported | 3.4 (1.2, 12.3) | 3.07 (1.36 – 6.90) | ||
| SE(logRR)/SE(logOR) | 0.414 | 0.052 | 0.062 | 0.435 | 0.594 | 0.414 |
Exhibit D9. Ventilator-Associated Pneumonia continued
| Josephson (2010) | Klompas (2011) | Klompas (2012) | Sammon (2013) | ||
|---|---|---|---|---|---|
| Study | Study Year | 2006-2007 | 2006-2007 | Not specified | 1999-2009 |
| Population | Patients with neurovascular disease in a California hospital | Mechanically ventilated patients >18 y in 3 geographically diverse hospitals | 8 U.S. hospital ICUs | Patients with any of 8 surgical oncology procedures | |
| Study Design | Retrospective | Retrospective matched control | Retrospective | Retrospective cohort | |
| Data Source(s) | Hospital clinical and administrative | Hospital clinical data | Hospital clinical data | HCUP-NIS | |
| Number of Cases | 24 | 55 | Not reported | 87,594 | |
| Definition of HAC | CDC-NHSN | CDC-NHS | Candidate surveillance definitions | ICD-9 | |
| Cost | Cost or Charges Reported | ||||
| Attributable | |||||
| Year of Cost Data | |||||
| Mean Attributable Cost Calculated | |||||
| Standard Error | |||||
|
Mortality |
Matched Control Sample | N | Y | Y | N |
| Adjusted RR/OR | 1.11 (0.37 – 3.30) | 1.1 (0.5 – 2.4) | 2.1 (1.3 – 3.3) | 4.90 (4.64 – 5.17) | |
| SE(logRR)/SE(logOR) | 0.558 | 0.395 | 0.238 | 0.02 |
Exhibit D10. Clostridium difficile Infections
| Donnelly (2015) | Glance (2011) | Kim (2012) | Lagu (2014) | Pakyz (2011) | Sundaram (2014) | Tabak (2013) | ||
|---|---|---|---|---|---|---|---|---|
| Study | Study Year | 2012-2014 | 2005-2006 | 2001-2008 | 2004-2010 | 2002-2007 | 2008-2011 | 2007-2008 |
| Population | Patients with solid organ transplant | Trauma patients LOS >3 days | Adults undergoing radical cystectomy for bladder cancer | Adult, non-surgical patients with sepsis | Adult patients | Adult patients with primary diagnosis of alcoholic hepatitis | Adult patients in six Pennsylvania hospitals | |
| Study Design | Retrospective cohort | Retrospective | Retrospective cohort | Retrospective cohort | Retrospective | Retrospective | Retrospective | |
| Data Source(s) | University Health System Consortium Clinical Database | HCUP-NIS | HCUP-NIS | Premier Healthcare Informatics Database | University Health System Consortium Clinical Database | HCUP-NIS | Clinical research database | |
| Number of Cases | 1,109 | 768 | 73 | 2,368 | 10,857 | 177 | 282 | |
| Definition of HAC | ICD-9 | ICD-9 | ICD-9 | ICD-9, lab results, and treatment codes | ICD-9 and treatment codes | ICD-9 | Toxin Assay | |
|
Cost |
Cost or Charges Reported | Cost | Cost | Cost | Cost | Cost | Charges | Cost |
| Attributable | Y | Y (ratio) | N | Y | N | N | Y | |
| Year of Cost Data | 2014 | 2011m | 2008 | 2010 | 2007 | 2011 | 2013n | |
| Mean Attributable Cost Calculated |
$27,890.65 |
$14,905.00 |
$22,634.00 |
$4,924.00 |
$27,160.00 |
$3,894.00 |
$6,117.00 |
|
| Standard Error |
$1,617.07 |
$1,147.00 |
$3,346.00 |
$1,244.00 |
$249.00 |
$1,382.00 |
$2,274.00 |
|
|
Mortality |
Matched Control Sample | N | N | N | Y | Y | N | Y |
| Adjusted RR/OR | 1.22 (0.9-1.65) | 1.87 (1.31-2.66) | 2.11 (1.04-4.28) | Not reported | Not reported | 1.75 (1.01-3.03) | 1.61 | |
| SE(logRR)/SE(logOR) |
0.155 |
0.181 |
0.361 |
0.060 |
0.037 |
0.280 |
0.214 |
m The year of cost data is not specified; the last year of the study period was used for the purpose of this analysis.
n The year of cost data is not specified; the last year of the study period was used for the purpose of this analysis.
Exhibit D10. Clostridium difficile Infections continued
| Damle (2014) | O’Brien (2007) | Flagg (2014) | Keshavamurthy (2014) | Lemaire (2015) | Lesperance (2011) | Luo (2015) | ||
|---|---|---|---|---|---|---|---|---|
| Study | Study Year | 2008-2012 | 1999-2003 | 2004-2008 | 2005-2011 | 2002-2009 | 2004-2006 | 2005-2011 |
| Population | Adult patients with colorectal resection and malignancy | All hospitalizations in a single Massachusetts hospital database with primary or secondary diagnosis of CDAD | Patients who underwent cardiac surgery | Patients who underwent cardiac surgery in a single Ohio hospital | Patients who underwent coronary artery bypass grafting and valvular surgery | Patients who underwent colonic resection during hospital admission | Adult patients with leukemia | |
| Study Design | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | |
| Data Source(s) | University Health System Consortium Database | Hospital database | HCUP-NIS | Hospital clinical data and REDCap database | HCUP-NIS | HCUP-NIS | HCUP-NIS | |
| Number of Cases | 1,266 | 3,692 | 2,581 | 145 | Not reported | 10,077 | 42,438 | |
| Definition of HAC | ICD-9 | ICD-9 | ICD-9 | Lab testing | ICD-9 | ICD-9 | ICD-9 | |
| Cost | Cost or Charges Reported | Cost | Cost | |||||
| Attributable | Y | Y | ||||||
| Year of Cost Data | 2008 | 2005 | ||||||
| Mean Attributable Cost Calculated | $14,130.00 | $13,675.00 | ||||||
| Standard Error | $465.00 | $583.00 | ||||||
| Mortality | Matched Control Sample | Y | Y | N | N | N | ||
| Adjusted RR/OR | Not reported | Not reported | 2.0 (1.65-2.35) (CABG) 1.9 (1.51-2.39) VS |
1.19 (1.11-1.29) | 1.17 (1.13-1.22) | |||
| SE(logRR)/SE(logOR) | 0.089 | 0.276 | 0.095 | 0.038 | 0.02 |
Exhibit D10. Clostridium difficile Infections Ccontinued
| Skovrlj (2014) | ||
|---|---|---|
| Study | Study Year | 2002-2011 |
| Population | Patients with lumbar spine surgery for degenerative diagnoses | |
| Study Design | Retrospective | |
| Data Source(s) | HCUP-NIS | |
| Number of Cases | 2,867 | |
| Definition of HAC | ICD-9 | |
| Cost | Cost or Charges Reported | |
| Attributable | ||
| Year of Cost Data | ||
| Mean Attributable Cost Calculated | ||
| Standard Error | ||
|
Mortality |
Matched Control Sample | N |
| Adjusted RR/OR | 9.6 (5.17-17.83) | |
| SE(logRR)/SE(logOR) | 0.316 |
Appendix E. Forest Plots
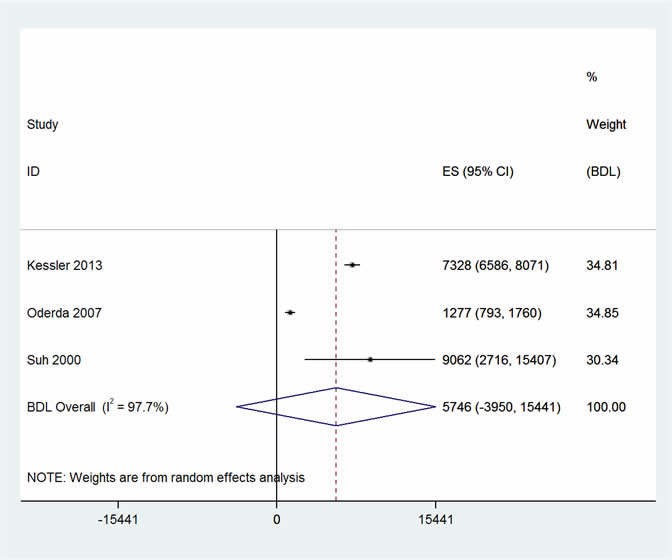
Adverse Drug Events
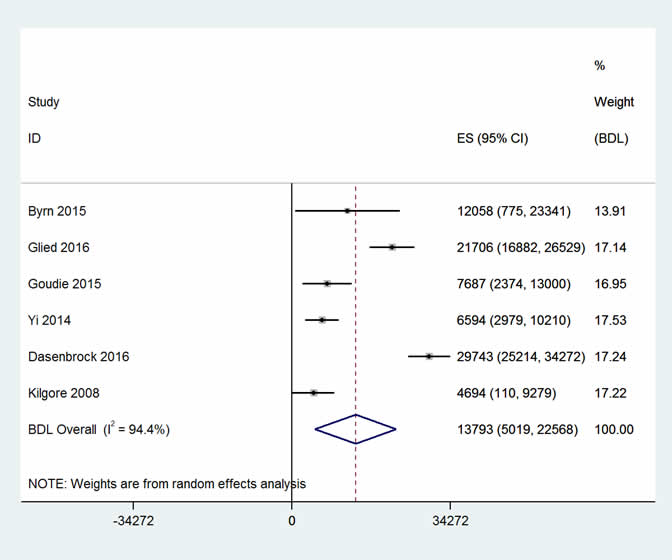
Catheter-Associated Urinary Tract Infection
Central-Line Associated Bloodstream Infections
Falls
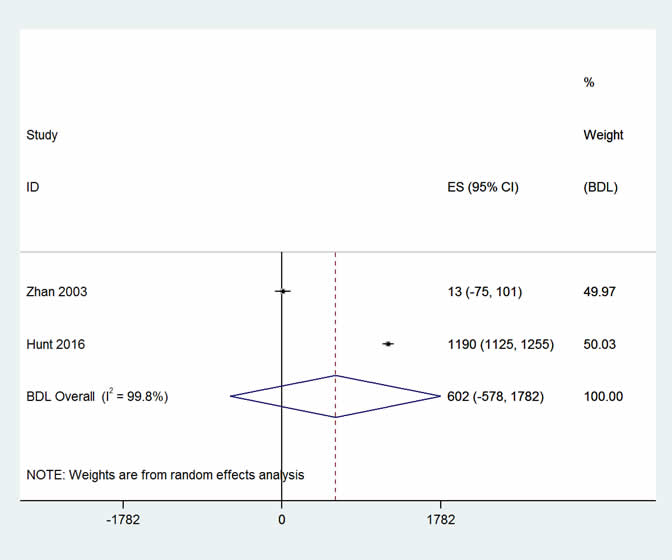
Obstetric Adverse Events
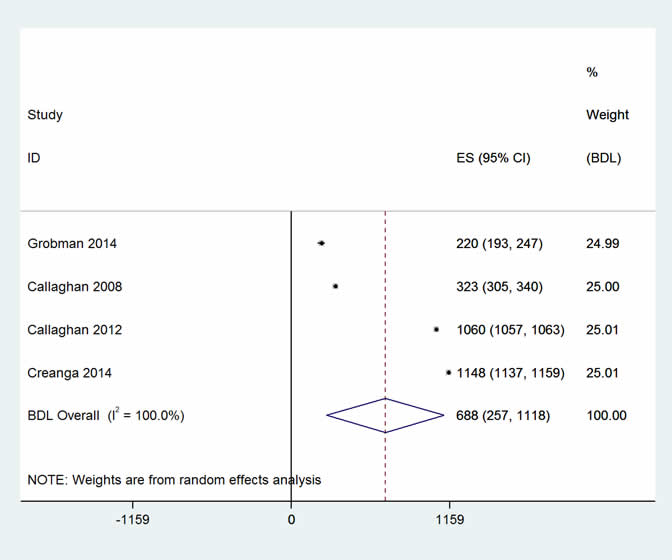
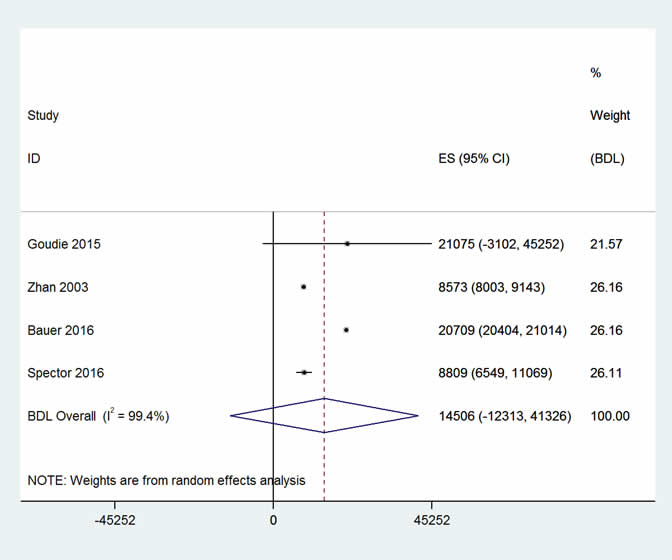
Pressure Ulcers
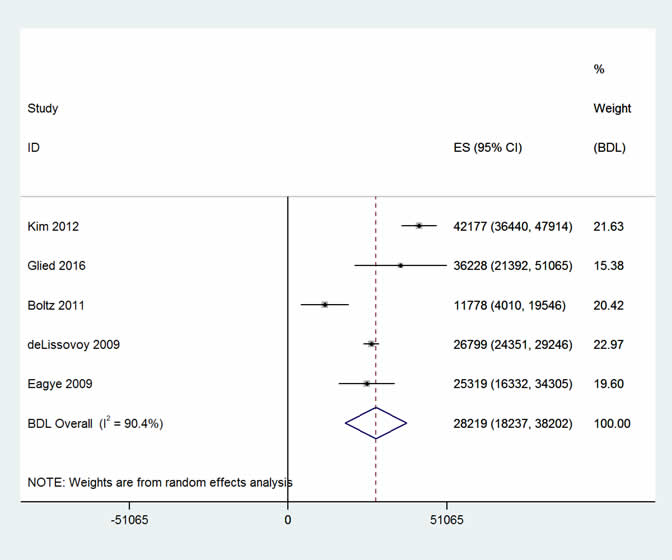
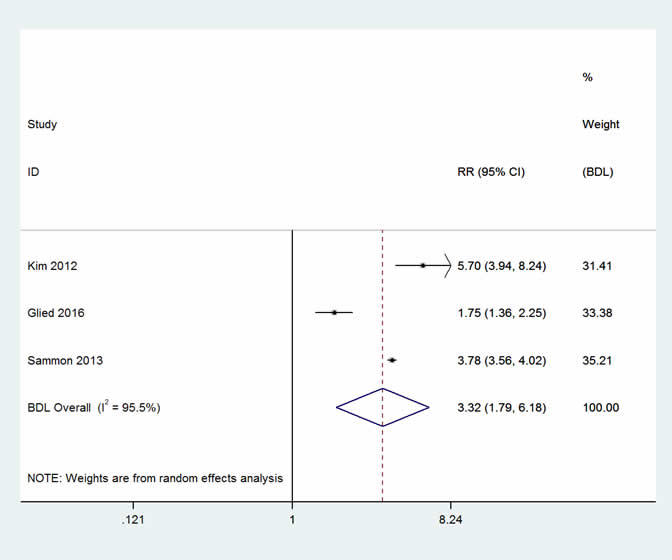
Surgical Site Infections
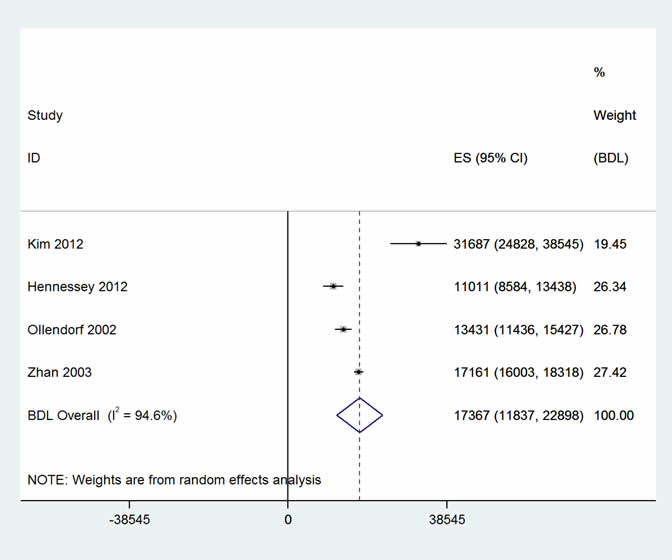
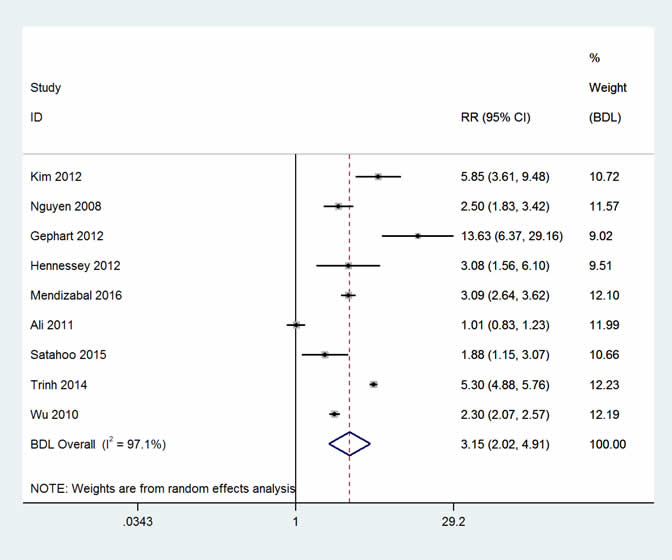
Venous Thromboembolism
Ventilator-Associated Pneumonia
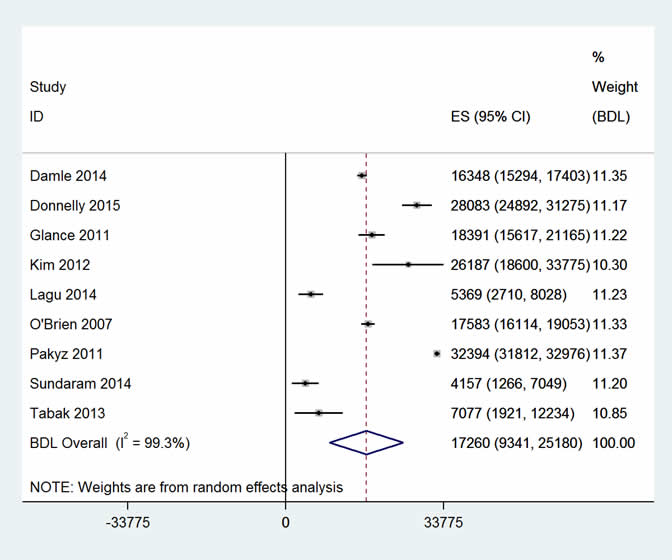
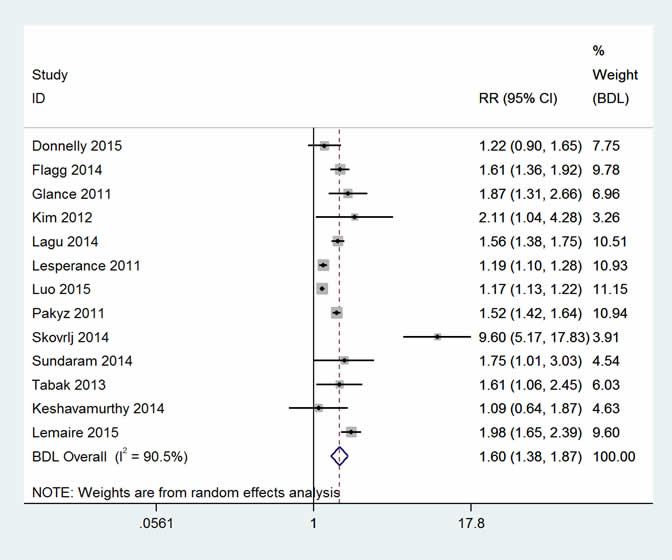
Clostridium difficile Infections