Webinar 1: Introduction & Overview: Slide Presentation
Designing & Delivering Whole-Person Transitional Care: The Hospital Guide to Reducing Medicaid Readmissions
Slide 1: Designing & Delivering Whole-Person Transitional Care
The Hospital Guide to Reducing Medicaid Readmissions
Webinar 1: Introduction & Overview
Slide 2: Agenda
- Introduction to the AHRQ Reducing Medicaid Readmissions Project.
- Overview of The Hospital Guide to Reducing Medicaid Readmissions.
- Introduction to the framing concepts of the Guide & methods:
- Why Medicaid?
- Why "Whole-Person"?
- Why "Data-Informed"?
Slide 3: Objectives
- Understand the purpose of the AHRQ Hospital Guide to Reducing Readmissions.
- Understand the focus on Medicaid as the catalyst for promoting "whole-person" care for all high-risk patients.
- Understand the Guide’s ASPIRE framework is intended to support a data-informed, strategic redesign of readmission reduction efforts.
Slide 4: AHRQ Reducing Medicaid Readmissions Project
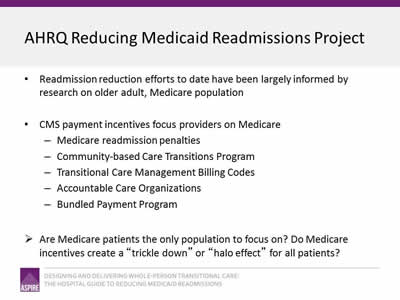
- Readmission reduction efforts to date have been largely informed by research on older adult, Medicare population.
- CMS payment incentives focus providers on Medicare:
- Medicare readmission penalties.
- Community-based Care Transitions Program.
- Transitional Care Management Billing Codes.
- Accountable Care Organizations.
- Bundled Payment Program.
- Are Medicare patients the only population to focus on? Do Medicare incentives create a "trickle down" or "halo effect" for all patients?
Slide 5: AHRQ Reducing Medicaid Readmissions Project
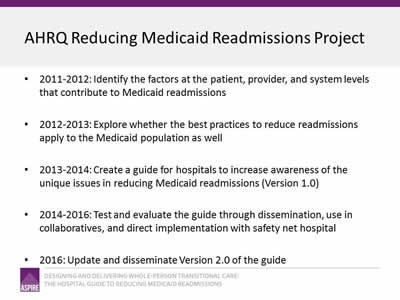
- 2011-2012: Identify the factors at the patient, provider, and system levels that contribute to Medicaid readmissions.
- 2012-2013: Explore whether the best practices to reduce readmissions apply to the Medicaid population as well.
- 2013-2014: Create a guide for hospitals to increase awareness of the unique issues in reducing Medicaid readmissions (Version 1.0).
- 2014-2016: Test and evaluate the guide through dissemination, use in collaboratives, and direct implementation with safety net hospital.
- 2016: Update and disseminate Version 2.0 of the guide.
Slide 6: Reducing Medicaid Readmissions Project Team
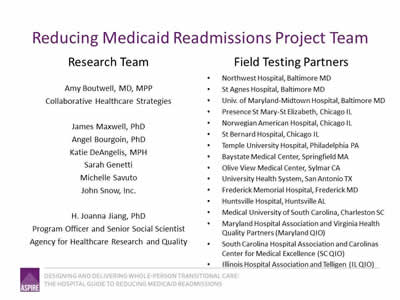
Research Team
Amy Boutwell, MD, MPP
Collaborative Healthcare Strategies
James Maxwell, PhD
Angel Bourgoin, PhD
Katie DeAngelis, MPH
Sarah Genetti
Michelle Savuto
John Snow, Inc.
H. Joanna Jiang, PhD
Program Officer and Senior Social Scientist
Agency for Healthcare Research and Quality
Field Testing Partners
- Northwest Hospital, Baltimore MD.
- St Agnes Hospital, Baltimore MD.
- Univ. of Maryland-Midtown Hospital, Baltimore MD.
- Presence St Mary-St Elizabeth, Chicago IL.
- Norwegian American Hospital, Chicago IL.
- St Bernard Hospital, Chicago IL.
- Temple University Hospital, Philadelphia PA.
- Baystate Medical Center, Springfield MA.
- Olive View Medical Center, Sylmar CA.
- University Health System, San Antonio TX.
- Frederick Memorial Hospital, Frederick MD.
- Huntsville Hospital, Huntsville AL.
- Medical University of South Carolina, Charleston SC.
- Maryland Hospital Association and Virginia Health Quality Partners (Maryland QIO).
- South Carolina Hospital Association and Carolinas Center for Medical Excellence (SC QIO).
- Illinois Hospital Association and Telligen (IL QIO).
Slide 7: Table of Contents
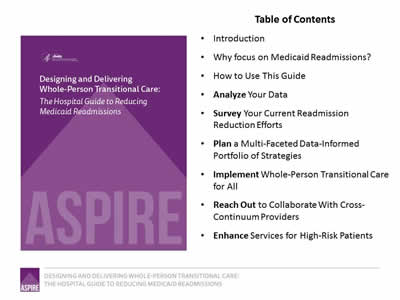
- Introduction.
- Why focus on Medicaid Readmissions?
- How to Use This Guide.
- Analyze Your Data.
- Survey Your Current Readmission Reduction Efforts.
- Plan a Multi-Faceted Data-Informed Portfolio of Strategies.
- Implement Whole-Person Transitional Care for All.
- Reach Out to Collaborate With Cross-Continuum Providers.
- Enhance Services for High-Risk Patients.
Image: Cover of the book, Designing & Delivering Whole-Person Transitional Care: The Hospital Guide to Reducing Medicaid Readmissions.
Slide 8: List of Tools
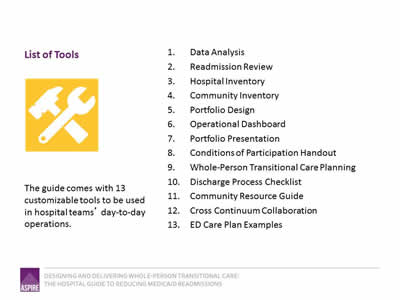
The guide comes with 13 customizable tools to be used in hospital teams’ day-to-day operations.
- Data Analysis.
- Readmission Review.
- Hospital Inventory.
- Community Inventory.
- Portfolio Design.
- Operational Dashboard.
- Portfolio Presentation.
- Conditions of Participation Handout.
- Whole-Person Transitional Care Planning.
- Discharge Process Checklist.
- Community Resource Guide.
- Cross Continuum Collaboration.
- ED Care Plan Examples.
Image: Tool icon (crossed hammer and wrench).
Slide 9: The ASPIRE Framework
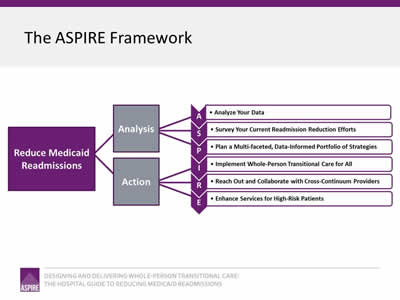
Image: The Framework is a flowchart reading from left to right. On the left is a box captioned "Reduce Medicaid Readmissions"; two lines connect this box to two boxes to its right captioned "Analysis" and "Action". Three lines each extend from "Analysis" and "Action" to connect to the elements that make up the ASPIRE acronym:
- Analyze Your Data.
- Survey Your Current Readmission Reduction Efforts.
- Plan a Multi-faceted, Data-Informed Portfolio of Strategies.
- Implement Whole-Person Transitional Care for All.
- Reach Out and Collaborate with Cross-Continuum Providers.
- Enhance Services for High-Risk Patients.
Slide 10: Why Focus on Medicaid Readmissions?
Why Focus on Medicaid Readmissions?
Slide 11: 6 Foundational Message from CMS
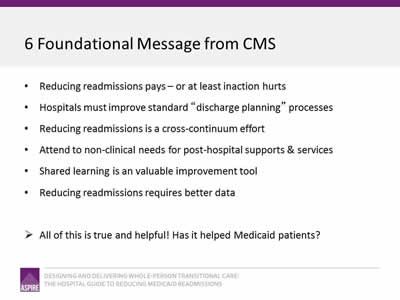
- Reducing readmissions pays—or at least inaction hurts.
- Hospitals must improve standard "discharge planning" processes.
- Reducing readmissions is a cross-continuum effort.
- Attend to non-clinical needs for post-hospital supports & services.
- Shared learning is an valuable improvement tool.
- Reducing readmissions requires better data.
- All of this is true and helpful! Has it helped Medicaid patients?
Slide 12: Medicare Penalty Focus Has Created Blinders
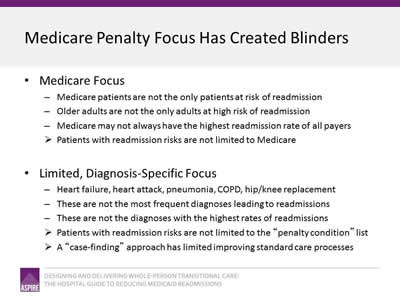
- Medicare Focus:
- Medicare patients are not the only patients at risk of readmission.
- Older adults are not the only adults at high risk of readmission.
- Medicare may not always have the highest readmission rate of all payers.
- Patients with readmission risks are not limited to Medicare.
- Limited, Diagnosis-Specific Focus:
- Heart failure, heart attack, pneumonia, COPD, hip/knee replacement.
- These are not the most frequent diagnoses leading to readmissions.
- These are not the diagnoses with the highest rates of readmissions.
- Patients with readmission risks are not limited to the "penalty condition" list.
- A "case-finding" approach has limited improving standard care processes.
Slide 13: Why Medicaid?
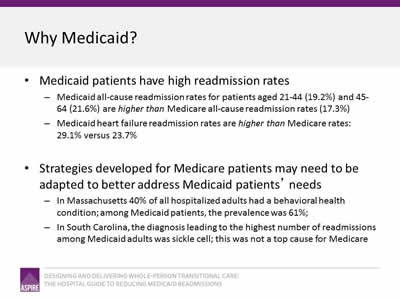
- Medicaid patients have high readmission rates:
- Medicaid all-cause readmission rates for patients aged 21-44 (19.2%) and 45-64 (21.6%) are higher than Medicare all-cause readmission rates (17.3%).
- Medicaid heart failure readmission rates are higher than Medicare rates: 29.1% versus 23.7%.
- Strategies developed for Medicare patients may need to be adapted to better address Medicaid patients’ needs:
- In Massachusetts 40% of all hospitalized adults had a behavioral health condition; among Medicaid patients, the prevalence was 61%.
- In South Carolina, the diagnosis leading to the highest number of readmissions among Medicaid adults was sickle cell; this was not a top cause for Medicare.
Slide 14: Why Take a "Whole-Person" Approach?
Why Take a "Whole-Person" Approach?
Slide 15: Whole-Person Approach
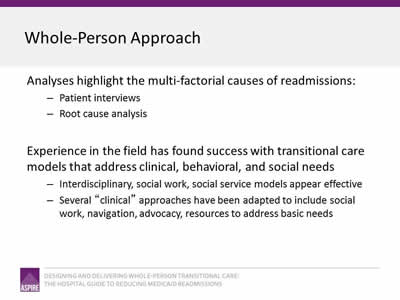
- Analyses highlight the multi-factorial causes of readmissions:
- Patient interviews.
- Root cause analysis.
- Experience in the field has found success with transitional care models that address clinical, behavioral, and social needs:
- Interdisciplinary, social work, social service models appear effective.
- Several "clinical" approaches have been adapted to include social work, navigation, advocacy, resources to address basic needs.
Slide 16: Whole-Person Approach
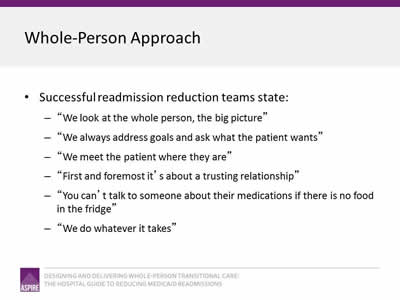
- Successful readmission reduction teams state:
- "We look at the whole person, the big picture."
- "We always address goals and ask what the patient wants."
- "We meet the patient where they are."
- "First and foremost it’s about a trusting relationship."
- "You can’t talk to someone about their medications if there is no food in the fridge."
- "We do whatever it takes."
Slide 17: What is a "Data-Informed" Approach?
What is a "Data-Informed" Approach?
Slide 18: Why Take A Data-Informed Approach?
- Many readmission reduction efforts have been launched in direct response to Medicare readmission penalties.
- The discharge diagnoses in the penalty program are not the top reasons for readmissions in the Medicare population.
- There are many high risk patients that go without improved transitional care when the focus is just on penalty conditions.
- Focusing on those diagnoses only will not reduce hospital-wide readmission rates.
Slide 19: Data-Informed Approach
- Articulate your hospital’s readmission reduction goal.
- Analyze your own hospital’s data to identify patients at high risk and unique readmission patterns.
- Understand root causes of readmissions among your patients.
- Implement an approach that is designed to effectively meet the transitional care needs of your patients.
- Track implementation and outcome data to continuously improve processes to reach your goal.
Slide 20: Summary
- The AHRQ Hospital Guide to Reducing Medicaid Readmissions encourages hospitals to:
- Expand readmission reduction efforts to all patients.
- Adapt strategies to better serve Medicaid patients.
- Employ a data-informed approach to designing efforts.
- Implement a whole-person approach to identifying and addressing patients’ transitional care needs.
- The ASPIRE Framework:
- Supports an updated strategic planning process.
- Recommends improving care in 3 domains: improve hospital-based care, collaborate across settings, deliver enhanced services.
Slide 21: Thank you
Thank you for your commitment to reducing readmissions
Amy E. Boutwell, MD, MPP
Collaborative Healthcare Strategies
amy@collaborativehealthcarestrategies.com
Angel Bourgoin, PhD & Jim Maxwell, PhD
John Snow, Inc.
Angel_Burgoin@jsi.com; Jim_Maxwell@jsi.com



