Webinar 5: Reach Out to Collaborate with Partners Across Settings: Slide Presentation
Designing & Delivering Whole-Person Transitional Care: The Hospital Guide to Reducing Medicaid Readmissions
Slide 1: Designing & Delivering Whole-Person Transitional Care
Designing & Delivering Whole-Person Transitional Care
The Hospital Guide to Reducing Medicaid Readmissions
Webinar 5: Reach Out to Collaborate with Partners Across Settings
Slide 2: Agenda
- Describe the important position that hospitals are in to lead delivery system transformation in their communities through aligning and leveraging resources to address whole-person needs.
- Describe why investing effort to identify Medicaid-relevant providers and agencies is core to effective efforts to reduce readmissions.
- Describe a step-wise approach to creating "effective referral pathways" to reduce barriers to linking patients to needed and available services.
Slide 3: Objectives
- Cast aside the assumption that "there are no resources in our community".
- Identify Medicaid-relevant providers, including community and health plan based care management services.
- Develop working relationships and processes for making it easier and more effective to ensure linkage to services.
Slide 4: Table of Contents
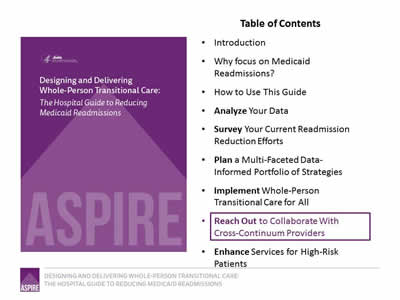
- Introduction.
- Why focus on Medicaid Readmissions?
- How to Use This Guide.
- Analyze Your Data.
- Survey Your Current Readmission Reduction Efforts.
- Plan a Multi-Faceted Data-Informed Portfolio of Strategies.
- Implement Whole-Person Transitional Care for All.
- Reach Out to Collaborate With Cross-Continuum Providers.
- Enhance Services for High-Risk Patients.
Image: Cover of the book, Designing & Delivering Whole-Person Transitional Care: The Hospital Guide to Reducing Medicaid Readmissions.
Slide 5: List of Tools
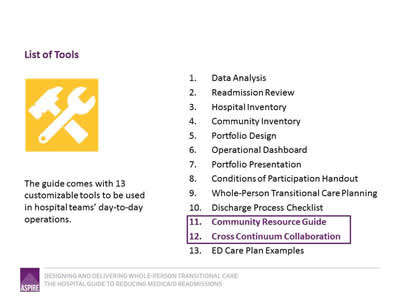
The guide comes with 13 customizable tools to be used in hospital teams’ day-to-day operations.
- Data Analysis.
- Readmission Review.
- Hospital Inventory.
- Community Inventory.
- Portfolio Design.
- Operational Dashboard.
- Portfolio Presentation.
- Conditions of Participation Handout.
- Whole-Person Transitional Care Planning.
- Discharge Process Checklist.
- Community Resource Guide.
- Cross Continuum Collaboration.
- ED Care Plan Examples.
Image: Tool icon (crossed hammer and wrench).
Slide 6: The ASPIRE Framework
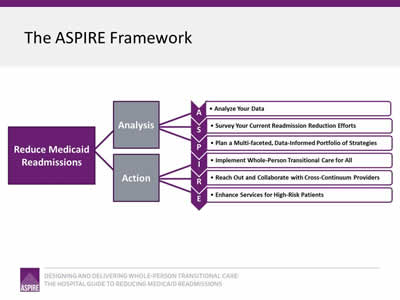
Image: The Framework is a flowchart reading from left to right. On the left is a box captioned "Reduce Medicaid Readmissions"; two lines connect this box to two boxes to its right captioned "Analysis" and "Action". Three lines each extend from "Analysis" and "Action" to connect to the elements that make up the ASPIRE acronym:
- Analyze Your Data.
- Survey Your Current Readmission Reduction Efforts.
- Plan a Multi-faceted, Data-Informed Portfolio of Strategies.
- Implement Whole-Person Transitional Care for All.
- Reach Out and Collaborate with Cross-Continuum Providers.
- Enhance Services for High-Risk Patients.
Slide 7: "We would be thrilled if someone from the hospital called us"
"We would be thrilled if someone from the hospital called us"
Slide 8: Cross-Continuum Collaboration: Whose Job is It?
- It’s the hospital’s job!
- CMS policies signal that hospitals are expected to lead delivery system transformation to more effectively deliver care across settings.
- Hospitals that do reach out to post-acute and community based providers and agencies find those partners are very receptive.
Slide 9: "There are many resources in the city..."
"There are many resources in the city, but it can be hard to find them. We need to inventory them and collect this information in one place."
Slide 10: Identify Medicaid-Relevant Partners
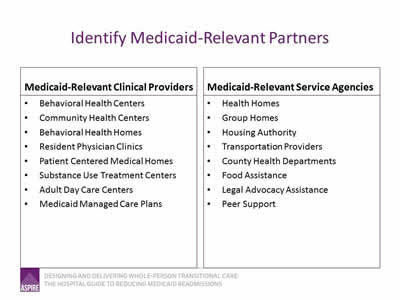
Medicaid-Relevant Clinical Providers
- Behavioral Health Centers.
- Community Health Centers.
- Behavioral Health Homes.
- Resident Physician Clinics.
- Patient Centered Medical Homes.
- Substance Use Treatment Centers.
- Adult Day Care Centers.
- Medicaid Managed Care Plans.
Medicaid-Relevant Service Agencies
- Health Homes.
- Group Homes.
- Housing Authority.
- Transportation Providers.
- County Health Departments.
- Food Assistance.
- Legal Advocacy Assistance.
- Peer Support.
Slide 11: Look for Care Management Resources
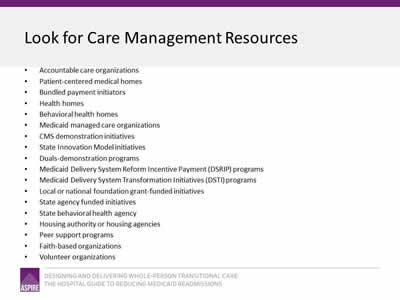
- Accountable care organizations.
- Patient-centered medical homes.
- Bundled payment initiators.
- Health homes.
- Behavioral health homes.
- Medicaid managed care organizations.
- CMS demonstration initiatives.
- State Innovation Model initiatives.
- Duals-demonstration programs.
- Medicaid Delivery System Reform Incentive Payment (DSRIP) programs.
- Medicaid Delivery System Transformation Initiatives (DSTI) programs.
- Local or national foundation grant-funded initiatives.
- State agency funded initiatives.
- State behavioral health agency.
- Housing authority or housing agencies.
- Peer support programs.
- Faith-based organizations.
- Volunteer organizations.
Slide 12: Community Resource Guide (Tool 11)
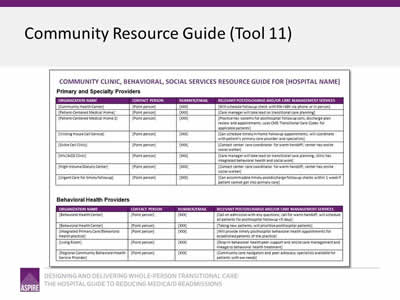
Image: The first page of the Community Resource Guide Tool.
Slide 13: Develop "Referral Pathways" to Ensure Effective Linkage to Services
Make doing the right thing the easy thing for staff.
Slide 14: Cross Continuum Coordination—Getting Started
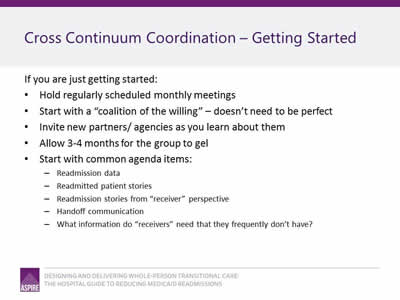
If you are just getting started:
- Hold regularly scheduled monthly meetings.
- Start with a "coalition of the willing"—doesn’t need to be perfect.
- Invite new partners/ agencies as you learn about them.
- Allow 3-4 months for the group to gel.
- Start with common agenda items:
- Readmission data.
- Readmitted patient stories.
- Readmission stories from "receiver" perspective.
- Handoff communication.
- What information do "receivers" need that they frequently don’t have?
Slide 15: Cross Continuum Coordination—Getting Specific
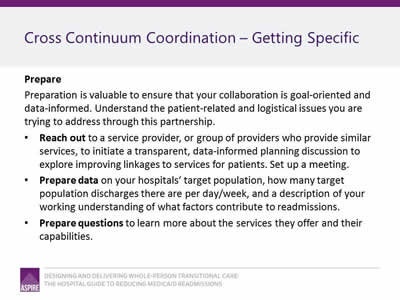
Prepare
Preparation is valuable to ensure that your collaboration is goal-oriented and data-informed. Understand the patient-related and logistical issues you are trying to address through this partnership.
- Reach out to a service provider, or group of providers who provide similar services, to initiate a transparent, data-informed planning discussion to explore improving linkages to services for patients. Set up a meeting.
- Prepare data on your hospitals’ target population, how many target population discharges there are per day/week, and a description of your working understanding of what factors contribute to readmissions.
- Prepare questions to learn more about the services they offer and their capabilities.
Slide 16: Cross Continuum Coordination—Getting Specific
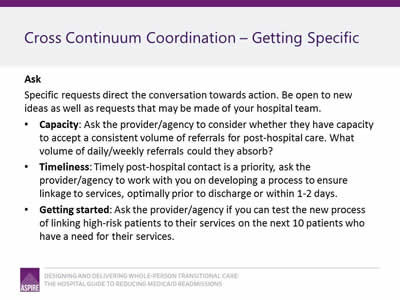
Ask
Specific requests direct the conversation towards action. Be open to new ideas as well as requests that may be made of your hospital team.
- Capacity: Ask the provider/agency to consider whether they have capacity to accept a consistent volume of referrals for post-hospital care. What volume of daily/weekly referrals could they absorb?
- Timeliness: Timely post-hospital contact is a priority, ask the provider/agency to work with you on developing a process to ensure linkage to services, optimally prior to discharge or within 1-2 days.
- Getting started: Ask the provider/agency if you can test the new process of linking high-risk patients to their services on the next 10 patients who have a need for their services.
Slide 17: Cross Continuum Coordination—Getting Specific
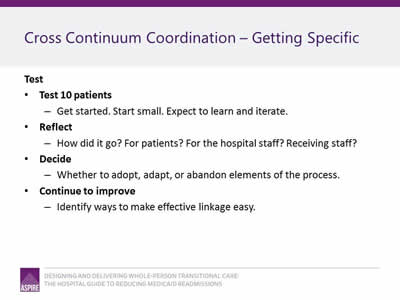
Test
- Test 10 patients:
- Get started. Start small. Expect to learn and iterate.
- Reflect:
- How did it go? For patients? For the hospital staff? Receiving staff?
- Decide:
- Whether to adopt, adapt, or abandon elements of the process.
- Continue to improve:
- Identify ways to make effective linkage easy.
Slide 18: Cross Continuum Coordination—Getting Specific
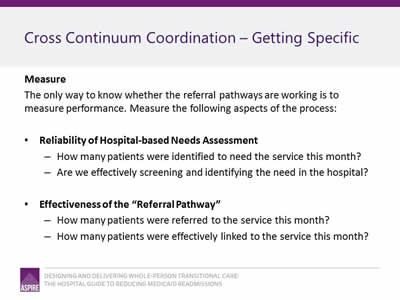
Measure
The only way to know whether the referral pathways are working is to measure performance. Measure the following aspects of the process:
- Reliability of Hospital-based Needs Assessment
- How many patients were identified to need the service this month?
- Are we effectively screening and identifying the need in the hospital?
- Effectiveness of the "Referral Pathway"
- How many patients were referred to the service this month?
- How many patients were effectively linked to the service this month?
Slide 19: In Practice: Collaborating with the MCO care manager
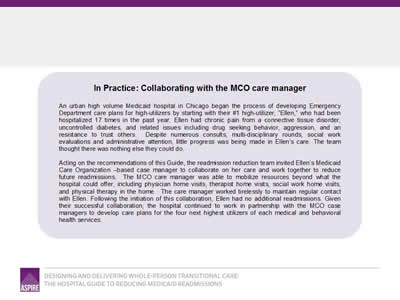
An urban high-volume Medicaid hospital in Chicago began the process of developing Emergency Department care plans for high-utilizers by starting with their #1 high-utilizer, "Ellen," who had been hospitalized 17 times in the past year. Ellen had chronic pain from a connective tissue disorder, uncontrolled diabetes, and related issues including drug-seeking behavior, aggression, and a resistance to trust others. Despite numerous consults, multi-disciplinary rounds, social work evaluations, and administrative attention, little progress was being made in Ellen's care. The team thought there was nothing else they could do.
Acting on the recommendation of this Guide, the readmission reduction team invited Ellen's Medicaid Care Organization-based care manager to collaborate on her care and work together to reduce further readmissions. The MCO care manager was able to mobilize resources beyond what the hospital could offer, including physician home visits, therapist home visits, social work home visits, and physical therapy in the home. The care manager worked tirelessly to maintain regular contact with Ellen. Following the initiation of this collaboration, Ellen had no additional readmissions. Given their successful collaboration, the hospital continued to work in partnership with the MCO case managers to develop care plans for the four next highest utilizers of each medical and behavioral health services.
Slide 20: In Practice: New Partnership with Behavioral Health Center
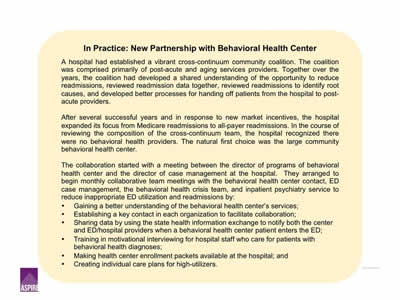
A hospital had established a vibrant cross-continuum community coalition. The coalition was comprised primarily of post-acute and aging services providers. Together over the years, the coalition had developed a shared understanding of the opportunity to reduce readmissions, reviewed readmission data together, reviewed readmissions to identify root causes, and developed better processes for handing off patients from the hospital to post-acute providers.
After several successful years and in response to new market incentives, the hospital expanded its focus from Medicare readmissions to all-payer readmissions. In the course of reviewing the composition of the cross-continuum team, the hospital recognized there were no behavioral health providers. The natural first choice was the large community behavioral health center.
The collaboration started with a meeting between the director of programs of behavioral health center and the director of case management at the hospital. They arranged to begin monthly collaboration team meetings with the behavioral health center contact, ED case management, the behavioral health crisis team, and inpatient psychiatry service to reduce inappropriate ED utilization and readmissions by:
- Gaining a better understanding of the behavioral health center services.
- Establishing a key contact in each organization to facilitate collaboration.
- Sharing data by using the state health information exchange to notify both the center and ED/hospital providers when a behavioral health center patient enters the ED.
- Training in motivational interviewing for hospital staff who care for patients with behavioral health diagnoses.
- Making health center enrollment packets available at the hospital.
- Creating individual care plans for high-utilizers.
Slide 21: Tool 12: Cross-Continuum Collaboration Tool
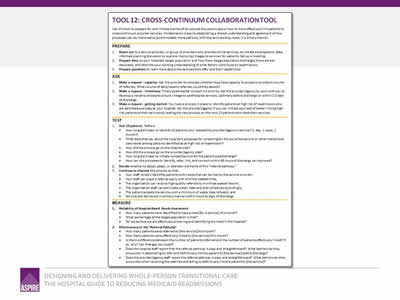
Image: The Cross-Continuum Collaboration Tool.
Slide 22: Summary
- Develop improvement-oriented collaborations with the providers and agencies that can best meet your patients’ transitional care needs.
- Specifically seek to identify Medicaid-relevant providers and agencies: health centers, behavioral health centers, health homes, etc.
- Identify and actively collaborate with care management entities; identify ways to efficiently connect with a care manager if one exists.
- Develop "referral pathways" to reduce barriers (time, knowledge, frustration) to linking patients with needed post hospital services.
Slide 23: Thank You
Thank you for your commitment to reducing readmissions
Amy E. Boutwell, MD, MPP
Collaborative Healthcare Strategies
amy@collaborativehealthcarestrategies.com
Angel Bourgoin, PhD & Jim Maxwell, PhD
John Snow, Inc.
Angel_Burgoin@jsi.com; Jim_Maxwell@jsi.com



