Establishing a Program of In Situ Simulations: Slide Presentation
AHRQ Safety Program for Perinatal Care
Slide 1: AHRQ Safety Program for Perinatal Care
Establishing a Program of In Situ Simulations
Slide 2: Learning Objectives
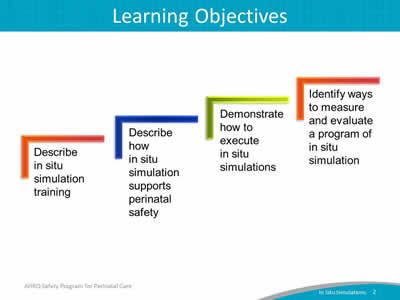
Image: Four ascending steps show the learning objectives:
- Describe in situ simulation training.
- Describe how in situ simulation supports perinatal safety.
- Demonstrate how to execute in situ simulations.
- Identify ways to measure and evaluate a program of in situ simulation.
Slide 3: Simulation Skill Development1
- Technical skills related to clinical assessment or intervention:
- Cervical exams, physical maneuvers, surgical procedures.
- Appropriate clinical management of a specific condition.
- Effective organization and use of supplies and equipment.
- Teamwork and communication (four core TeamSTEPPS® skills):
- Leadership.
- Communication.
- Mutual support.
- Situational awareness.
Slide 4: In Situ Simulation Defined1,2,3,4
- In situ simulations are physically integrated into the usual clinical environment, allowing for practice in one's own hospital setting with familiar resources and equipment.
- Each person involved performs his or her own role as if the scenario were real.
- All disciplines participate, including support personnel (lab, pharmacy, etc.).
- In situ simulation complements simulation training conducted in a dedicated simulation center.
Slide 5: Benefits of In Situ Simulation3,5,6,7
- Provides a method to improve reliability and safety in high-risk areas such as labor and delivery (L&D).
- Allows for experiential learning and practice related to teamwork and communication.
- Improves ability to address latent threats and systems issues.
Slide 6: Evidence for Using Simulations in L&D
- Multiple studies have demonstrated that teamwork training using simulation as an independent intervention results in improvement in knowledge, practical skills, communication, and team performance in acute maternity care situations.8-10
Slide 7: Scenarios for Simulation
- Simulation scenarios can be designed to replay real events that have occurred on your unit.
- Simulation scenarios can be designed for uncommon, but serious, obstetric emergencies requiring rapid recognition and response (e.g., shoulder dystocia, postpartum hemorrhage, cord prolapse).
- Simulation scenarios can be designed to fine-tune existing processes or to train staff on new processes and protocols (e.g., use of safe cesarean section checklist).
Slide 8: Three Components of an In Situ Simulation11
- Briefing.
- Facilitating the simulation.
- Debriefing.
Slide 9: Briefing
- Immediately before the simulation, the facilitator briefs participants about the purpose and ground rules; this usually takes about 10 minutes. The facilitator will—
- Ask participants to treat the simulated event like an actual patient situation.
- Emphasize the primary focus is on how teams communicate and perform as a unit.
- Share information about the timeframe for simulation, use of simulation equipment (if applicable), and rules of participation.
Slide 10: Briefing: Using Video
- Video recording the simulation can be a useful tool for reviewing team performance during the debriefing.3
- Video recording can induce anxiety in participants.
- Explain the purpose of video recording prior to simulation.
- Seek legal guidance and signed releases from simulation participants if the video may be used for purposes other than debriefing, such as for education or training.
Slide 11: Facilitating the Simulation: Scenario Design1
Components of a well-designed scenario include—
- Clinical context:
- Not all contexts are equal for training purposes.
- Context should be appropriate for eliciting the team behavior of interest.
Slide 12: Facilitating the Simulation: Scenario Design1
Components of a well-designed scenario include—
- Event sets (typically 3 to 5 per simulation):
- Triggers: The incident to elicit the team behavior.
- Distractors: Characteristics that may divert the team’s attention (e.g., family member asking questions).
- Expected Responses: The appropriate behavioral responses to each event-set trigger.
Slide 13: Facilitating the Simulation: Execution
- Simulation facilitators are primarily observers.
- Facilitators introduce new information into the simulation as needed.
- Avoid facilitating or "scripting" the simulation too tightly; this makes it difficult to observe targeted responses to a specific trigger.
- Simulations that lead to "one right answer" are not realistic and won’t help teams develop the ability to recognize and adapt to changing circumstances.
Slide 14: Facilitating the Simulation: Execution
- Keep the simulation going for a prespecified period of time, typically up to 15 to 20 minutes.
Slide 15: Debriefing: Definition
- Debriefing helps participants understand the complex team skills and knowledge required for quality patient care.3,11
- Provides a structure for understanding the scenario.
- Helps ensure everyone takes away similar lessons from the experience.
- Helps to keep the discussion focused on events relevant to the learning objectives of the simulation.
Slide 16: Debriefing: Logistics
- Takes about 3 to 5 minutes to debrief for every minute of the actual simulation.
- So a simulation run for 15 minutes will need at least 45 minutes to debrief. (This does not include time needed to review video if the simulation is being recorded.)
- Consider reserving a separate space for the debrief, especially if a screen to review a video recording of the simulation is needed.
Slide 17: Debriefing: Introduce the Debrief Process
- All team members in the simulation participate.
- The focus is primarily on team performance.
- Teamwork and communication skills are the focus of the debriefing questions.
- So that clinical/technical issues or questions are not overlooked, can use debrief to quickly clarify an issue, but individually directed remediation should be handled outside of the debrief.
- Consider a dual debrief, where one portion focuses on teamwork and communication, and a separate portion focuses on the clinical/technical response.
Slide 18: Debriefing: Describe What Happened
- First, each participant states their name, role, and what they think went well during the simulation.
- If simulation was recorded, watch the video. Pause at intervals to discuss the following:
- What went well?
- What could have gone better?
- What would you want to do differently next time?
Slide 19: Debriefing: Describe What Happened
- It is important for the participants to realize it is "their debriefing."
- An internal discussion of teamwork and communication principles is one of the goals of the debriefing.
- Video review is extremely helpful in allowing the participants to see exactly what communication occurred and what kind of teamwork was employed.
- Ideally everyone participates so that their unique perspective (such as their role) is heard.
Slide 20: Debriefing: Conduct a Performance Analysis
- Consider using a simulation assessment tool:
- It can be used by any observers of the simulation.
- If the simulation was video recorded, participants can use it to evaluate themselves as they watch the video.
- Compare the team’s performance with expected responses:
- Were the expected behaviors performed when necessary?
- If so, were they performed correctly, or could they be improved?
Slide 21: Debriefing: Identify Lessons Learned
- The final step is to look ahead to how the team members can generalize what they learned in the scenario to their daily practice.
- The team discusses what behaviors it should begin performing.
- Explicit measures associated with the simulation scenario can help promote reflection about how to transfer what went well in the simulation to the actual clinical environment.
Slide 22: Planning
Planning
Slide 23: Engage Leadership
- Discuss and determine a shared vision for the unit’s program of in situ simulation training.
- Be clear about the purpose of simulation training (i.e., teamwork development vs. individual performance evaluation).
- Identify concrete training goals.
Slide 24: Staff Readiness
- Ensure unit staff receive teamwork and communication training (e.g., TeamSTEPPS) before implementing an in situ simulation training program.
- This provides the team with a common language and communication framework.
- Ensure enough staff members know how to facilitate simulations.
Slide 25: Participants
- All disciplines involved in providing services or care to patients on L&D units should participate in simulations, including—
- Maternity care providers (obstetricians/family physicians/midwives).
- Nursing staff.
- Neonatal providers.
- Anesthesiology staff.
- Residents (all specialties that provide care on labor and delivery).
- Operating room technicians/assistants.
- Administrative support personnel (unit clerks).
- Lab and pharmacy staff.
Slide 26: Participants
- Define clear requirements for staff participation:
- Decide how often to conduct simulations. How many different scenarios?
- Will incentives or consequences be used to drive staff participation?
Slide 27: Simulation Scenarios
- Determine the simulation scenarios your unit or program will use.
- Sample simulation scenarios for the following topics are available through the Safety Program for Perinatal Care:
- Postpartum hemorrhage.
- Shoulder dystocia.
- Umbilical cord prolapse.
- Uterine tachysystole.
- Antepartum hemorrhage.
- Preeclampsia/seizure.
- Severe abdominal pain/vaginal birth after cesarean.
- Postoperative cesarean section complication.
- Magnesium toxicity.
Slide 28: Simulation Scenarios
- Other sample scenarios are available from professional organizations, perinatal quality and safety organizations, and commercial entities.12-14
- An accompanying video offers an example of an in situ simulation, including the briefing and debriefing process:
- Link to video: https://youtu.be/UhIuGgZB60g
- Also located in the AHRQ Toolkit for Improving Perinatal Safety: https://www.ahrq.gov/professionals/quality-patient-safety/hais/tools/perinatal-care/modules/situ.html
Slide 29: Equipment
- In situ simulations generally use the equipment of the clinical area in which the simulation takes place.
- Some simulations may require a pelvic model or birthing simulator.
- The use of standardized patients ("actors") may replace simulators in many cases.
Slide 30: Logistics
- Create a schedule for simulation trainings that aligns with the unit’s shared vision and staff participation criteria.
- Plan for transportation of simulation equipment to/from unit.
- Store equipment in L&D unit, if possible.
- Set aside time for transport, setup, and dismantling.
Slide 31: Logistics
- Consider whether real or simulated medical supplies (e.g., drugs, blood) and equipment will be used.
- Use of real supplies—
- May prevent simulated drugs/medication/equipment from accidentally being used with real patients.
- Is wasteful, particularly when supply shortages exist.
- Use of simulated supplies—
- Requires vigilance to ensure supplies and equipment are clearly marked so will not mistakenly be used on actual patients.
- Requires use of infection-control practices for reuse of simulation equipment.
- Use of real supplies—
Slide 32: Conflicts With Patient Care
Prospectively designate standards and limits for conducting simulations on the unit.
- Scheduled in situ simulations may be cancelled or end early because of competing patient care demands.
- A time limit may be imposed on simulations and debriefing to reduce impact on clinical care.
Slide 33: Conflicts With Patient Care
Prospectively designate standards and limits for conducting simulations on the unit.
- Discussions with your hospital’s patient advocacy groups, if possible, may be beneficial.
- A Hospital Medical Center reported support from its family advocate group because benefits of simulation training outweighed disadvantages.3
Slide 34: Evaluation
Evaluation
Slide 35: Data for Evaluation
A successful in situ simulation training program requires evaluation and continuous improvement.11
- Consider using data from "safety culture" surveys.
- Collect participant evaluation forms.
- Collect qualitative feedback from staff participants who have participated in simulations.
- Use other measures to track the impact of the simulation program.
Slide 36: Designing Measures: Clarify Purpose1
- Diagnose root causes of performance deficiencies:
- Identify specific weaknesses, such as poor "SBAR."
- Provide feedback:
- Relay information regarding strengths and weaknesses as a remediation plan.
- Conduct assessment:
- Evaluate the level of proficiency or readiness.
Slide 37: Designing Measures: What To Measure1
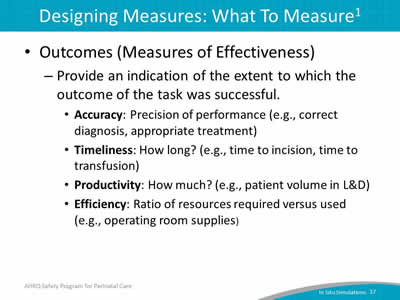
- Outcomes (Measures of Effectiveness):
- Provide an indication of the extent to which the outcome of the task was successful.
- Accuracy: Precision of performance (e.g., correct diagnosis, appropriate treatment).
- Timeliness: How long? (e.g., time to incision, time to transfusion).
- Productivity: How much? (e.g., patient volume in L&D).
- Efficiency: Ratio of resources required versus used (e.g., operating room supplies).
- Provide an indication of the extent to which the outcome of the task was successful.
Slide 38: Designing Measures: What To Measure1
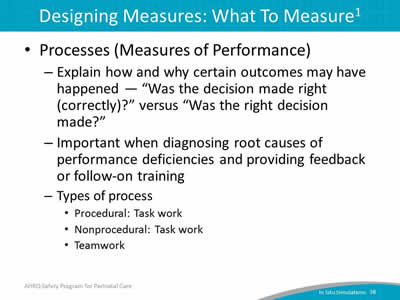
- Processes (Measures of Performance):
- Explain how and why certain outcomes may have happened—"Was the decision made right (correctly)?" versus "Was the right decision made?"
- Important when diagnosing root causes of performance deficiencies and providing feedback or follow-on training:
- Types of process.
- Procedural: Task work.
- Nonprocedural: Task work.
- Teamwork.
Slide 39: Unit Next Steps
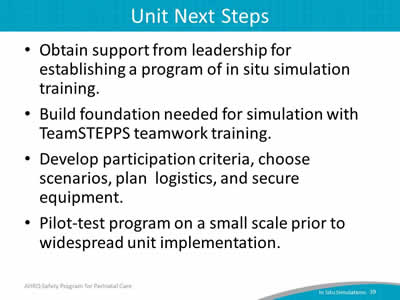
- Obtain support from leadership for establishing a program of in situ simulation training.
- Build foundation needed for simulation with TeamSTEPPS teamwork training.
- Develop participation criteria, choose scenarios, plan logistics, and secure equipment.
- Pilot-test program on a small scale prior to widespread unit implementation.
Slide 40: References
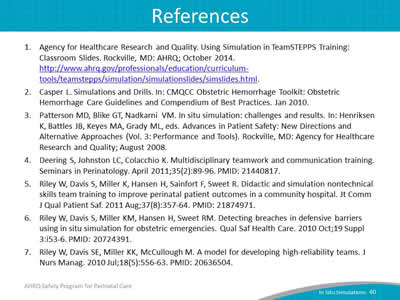
- Agency for Healthcare Research and Quality. Using Simulation in TeamSTEPPS Training: Classroom Slides. Rockville, MD: AHRQ; October 2014. http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/simulation/simulationslides/simslides.html.
- Casper L. Simulations and Drills. In: CMQCC Obstetric Hemorrhage Toolkit: Obstetric Hemorrhage Care Guidelines and Compendium of Best Practices. Jan 2010.
- Patterson MD, Blike GT, Nadkarni VM. In situ simulation: challenges and results. In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools). Rockville, MD: Agency for Healthcare Research and Quality; August 2008.
- Deering S, Johnston LC, Colacchio K. Multidisciplinary teamwork and communication training. Seminars in Perinatology April 2011;35(2):89-96. PMID: 21440817.
- Riley W, Davis S, Miller K, Hansen H, Sainfort F, Sweet R. Didactic and simulation nontechnical skills team training to improve perinatal patient outcomes in a community hospital. Jt Comm J Qual Patient Saf 2011 Aug;37(8):357-64. PMID: 21874971.
- Riley W, Davis S, Miller KM, Hansen H, Sweet RM. Detecting breaches in defensive barriers using in situ simulation for obstetric emergencies. Qual Saf Health Care 2010 Oct;19 Suppl 3:i53-6. PMID: 20724391.
- Riley W, Davis SE, Miller KK, McCullough M. A model for developing high-reliability teams. J Nurs Manag 2010 Jul;18(5):556-63. PMID: 20636504.
Slide 41: References
- Draycott TJ, Crofts JF, Ash JP, et al. Improving neonatal outcome through practical shoulder dystocia training. Obstet Gynecol July 2008;112(1):14-20. PMID: 18591302.
- Phipps MG, Lindquist DG, McConaughey E, et al. Outcomes from a labor and delivery team training program with simulation component. Am J Obstet Gynecol Jan 2012;206(1):3-9. PMID: 21840493.
- Ellis D, Crofts JF, Hunt LP, et al. Hospital, simulation center, and teamwork training for eclampsia management: a randomized controlled trial. Obstet Gynecol March 2008;111(3):723-31. PMID: 18310377.
- Miller KK, Riley W, Davis S, Hansen, HE. In situ simulation: a method of experiential learning to promote safety and team behavior. J Perinat Neonat Nurs 2008;22(2):105-13. PMID: 18496069.
- Wisconsin Association for Perinatal Care. Postpartum Hemorrhage: Resources. https://www.perinatalweb.org/major-initiatives/postpartum-hemorrhage/resources. Accessed May 9, 2016.
- California Maternal Quality Care Collaborative. OB Hemorrhage Toolkit V 2.0. Improving Health Care Response to Obstetric Hemorrhage, Version 2.0: A California Toolkit to Transform Maternity Care. Released March 2015. https://www.cmqcc.org/resources-tool-kits/toolkits/ob-hemorrhage-toolkit. Accessed May 9, 2016.
- American Congress of Obstetrics and Gynecology. ACOG Simulations Consortium Learning Objectives: Postpartum Hemorrhage Caused by Uterine Atony. n.d. https://www.acog.org/~/media/Departments/Simulations%20Consortium/Learning%20Objectives/Postpartum_Hemorrhage.pdf. Accessed May 9, 2016.
Slide 42: Disclaimer
Every effort was made to ensure the accuracy and completeness of this resource. However, the U.S. Department of Health and Human Services makes no warranties regarding errors or omissions and assumes no responsibility or liability for loss or damage resulting from the use of information contained within.
The U.S. Department of Health and Human Services cannot endorse, or appear to endorse derivate or excerpted materials, and it cannot be held liable for the content or use of adapted resources. Any adaptations of this resource must include a disclaimer to this effect.
Reference to any specific commercial products, process, service, manufacturer, company, or trademark does not constitute endorsement or recommendation by the U.S. Government, HHS, or AHRQ of the linked Web resources or the information, products, or services contained therein. The Agency does not exercise any control over the content on these sites.



