Monitoring for Perinatal Safety: Electronic Fetal Monitoring: Slide Presentation
AHRQ Safety Program for Perinatal Care
Slide 1: Monitoring for Perinatal Safety: Electronic Fetal Monitoring
Monitoring for Perinatal Safety: Electronic Fetal Monitoring
Slide 2: Learning Objectives
Image: This slide shows stair steps for learning objectives:
- Step 1. Describe the role of electronic fetal monitoring for perinatal patient safety.
- Step 2. Identify the key safety elements related to the use of electronic fetal monitoring.
- Step 3. Identify ways to apply key safety elements to your unit policies, procedures, and practices related to electronic fetal monitoring.
Slide 3: Electronic Fetal Monitoring
- Electronic fetal monitoring (EFM) is a commonly used practice on labor and delivery (L&D) units and is a focus of this customizable bundle within the AHRQ Safety Program for Perinatal Care.
- The training materials and tool for this bundle offer key safety elements for the use of EFM.
- Key safety elements
- Provide a comprehensive starting point for each unit to consider as it establishes its processes for ensuring safe practices related to EFM use.
- Can be adapted and applied to other monitoring practices commonly used during intrapartum care.
Slide 4: EFM and Perinatal Safety
- Between 1996 and 2004, 34% of the cases of perinatal death or permanent disability reported to The Joint Commission included inadequate fetal monitoring as a root cause.1
- Common safety issues related to EFM include—1,2,3
- Lack of knowledge related to interpreting EFM.
- High intra-observer and inter-observer variability in the interpretation of EFM.
- Poor communication related to EFM findings.
- Fear of conflict, intimidation, and failure to function as a team.
- These issues may result in delayed or no response to abnormal fetal tracings.
- These issues may also result in unnecessary interventions (surgical or otherwise) in the setting of normal fetal tracings.
Slide 5: Perinatal Safety and Professional Liability
- EFM interpretation and management are a common issue in litigation involving adverse outcomes in term pregnancies.
- According to the 2012 American Congress of Obstetricians and Gynecologists liability survey—4
- 77% of OB-GYN physicians have experienced at least one professional liability claim during their career.
- 20.9% of obstetric claims involved EFM.
Slide 6: Rationale for Safe EFM
- Accurate interpretation of EFM may lead to increased recognition of abnormal fetal heart rate patterns and avoid overintervention for normal patterns.
- A unit culture of safety and teamwork may improve communication of EFM findings and reduce fear of conflict and intimidation.
Slide 7: Safe EFM Tool
- Purpose.
- Who should use.
- How to use.
- Key safety elements.
- Sample cognitive aid.
Slide 8: Key Perinatal Safety Elements for EFM
- Standardize When Possible (CUSP Science of Safety).
- Create Independent Checks (CUSP Science of Safety).
- Learn From Defects (CUSP Module).
- Simulation (Safety Program for Perinatal Care program pillar).
- Teamwork Training (TeamSTEPPS®).
- Patient and Family Engagement (CUSP Module).
Slide 9: Key Safety Elements: Standardize When Possible
- L&D staff should use standard terminology to interpret, communicate, and document fetal heart rate (FHR) and uterine contraction patterns for all patients receiving EFM.3
- The 2008 National Institute for Child Health and Human Development (NICHD) Workshop developed nomenclature that has been adopted by several professional organizations as the standard nomenclature to use for describing and interpreting FHR and uterine contraction patterns.3,5,6
Slide 10: Key Safety Elements: Standardize When Possible
- Increasing staff use of NICHD nomenclature may be supported through unit policies regarding training and certification.
- EFM training courses and certification are offered through several professional organizations, commercial entities, and local colleges or universities.7-12
- Links to several resources for training and certification are provided in the Safe EFM tool.
- Few studies have examined the individual effects of formal EFM training or certification on perinatal health outcomes, though many perinatal safety interventions include EFM courses or certification as one component of a multicomponent approach.13,14
Slide 11: Key Safety Elements: Standardize When Possible
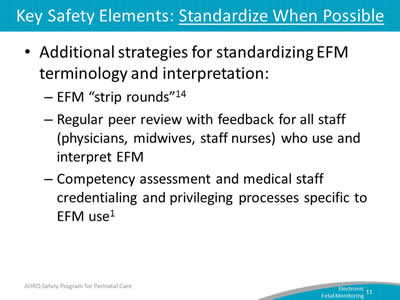
- Additional strategies for standardizing EFM terminology and interpretation:
Slide 12: Key Safety Elements: Create Independent Checks
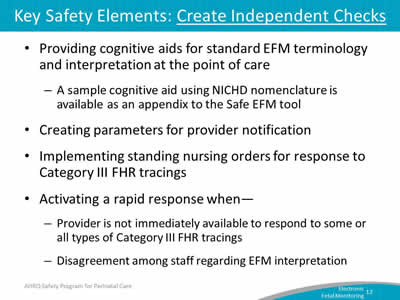
- Providing cognitive aids for standard EFM terminology and interpretation at the point of care
- A sample cognitive aid using NICHD nomenclature is available as an appendix to the Safe EFM tool.
- Creating parameters for provider notification.
- Implementing standing nursing orders for response to Category III FHR tracings.
- Activating a rapid response when—
- Provider is not immediately available to respond to some or all types of Category III FHR tracings.
- Disagreement among staff regarding EFM interpretation.
Slide 13: Key Safety Elements: Learn From Defects
- Debrief and analyze near misses and adverse events, and the contribution of EFM use, EFM interpretation, and communication of EFM findings.
- Have a process in place to review severe maternal or neonatal morbidity and mortality events.
- Share outcomes or process improvements from the debriefings and from formal analysis with staff to achieve transparency and enhance organizational learning.
Slide 14: Key Safety Elements: Simulation
- In situ simulation can improve knowledge, practical skills, communication, and team performance in acute situations.
- Several sample scenarios in the Safety Program for Perinatal Care can be used to train teams on some key elements of safe EFM use.
- These scenarios reinforce teamwork and communication related to—
- Situational awareness;
- Ability to get additional help quickly.
- Use of cognitive aids for nomenclature to use for interpreting and communicating EFM findings.
- Timely use of standing orders for managing Category III FHR tracings.
- Communication with rapid responders.
- Communication with patient/family.
- Use of briefings, huddles, and debriefings.
Slide 15: Key Safety Elements: Teamwork Training
- Have situational awareness during use of EFM.
- Use SBAR, callouts, huddles, and closed-loop communication techniques.
- Use predetermined approach to call for additional rapid assistance.
- Communicate during transitions of care.
- Have high-reliability teams.
Slide 16: Key Safety Elements: Teamwork Training
- Characteristics of high-reliability teams
- Anyone can sound an alarm, request help, or challenge the status quo.
- Hierarchy is minimized.
- Communication is continuous, valued, and expected.
- Team members protect one another from work overload.
- Team members will advocate for the patient when one person's viewpoint does not coincide with another's.
- Team members manage conflict using a constructive positive approach to emphasize "what is right, not who is right."
Slide 17: Key Safety Elements: Patient and Family Engagement
- Engaging patient in decisions to use continuous EFM versus other approaches in appropriate candidates.15
- Communicating with patient and family during an episode involving an abnormal fetal tracing.
- Disclosing any unintended outcomes using unit policy for adverse events.
Slide 18: Unit Next Steps
- Decide whether to select the Safe EFM bundle for implementation locally. Factors to consider:
- Organizational culture regarding use of EFM suggesting need for a unit-based approach:
- Is standard NICHD terminology consistently used for interpretation and communication of EFM findings?
- Do timely and appropriate clinical responses occur with respect to EFM findings?
- Past adverse events related to EFM use.
- Synergy with related or similar initiatives.
- Interest and enthusiasm of unit staff for implementing.
- Organizational culture regarding use of EFM suggesting need for a unit-based approach:
Slide 19: Unit Next Steps
- Review Key Safety Elements tool with implementation team, considering any existing facility processes or procedures related to EFM use.
- Support implementation of Key Safety Elements through—
- Unit policies and procedures.
- Staff training/communication.
- Simulation.
- Monitor implementation progress and impact, collect data for quality improvement.
Slide 20: Tips for Implementation Success
- Use Comprehensive Unit-Based Safety Program (CUSP) principles for implementing teamwork and communication (e.g., incorporating diverse perspectives) to develop consensus on the unit's approach to safe EFM use.
- Pilot test any new procedures on a limited scale to work out any bugs or problems.
- Comprehensively review the unit procedures each year to assess the need for updates to ensure content is up to date.
- Create a mechanism for identifying recurrent nonuse or deviation from the established procedures by clinicians. Seek to understand why, rather than assign blame.
Slide 21: References
- The Joint Commission. Sentinel Event Alert: Issue #30 Preventing Infant Death and Injury During Delivery. 2004. http://www.jointcommission.org/sentinel_event_alert_issue_30_preventing_infant_death_and_injury_during_delivery. Accessed May 9, 2016.
- Miller MA. System errors in intrapartum electronic fetal monitoring: a case review. J Midwifery Women's Health 2005 Nov-Dec;50(6):507-16. PMID: 16260365
- American Congress of Obstetricians and Gynecologists. Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol 2009 Jul;114(1):192-202. PMID: 19546798. [Reaffirmed 2015]
- American Congress of Obstetricians and Gynecologists. 2012 ACOG Survey on Professional Liability Results 2012. http://www.acog.org/-/media/Departments/Professional-Liability/2012PLSurveyNational.pdf. Accessed May 9, 2016.
- Macones GA, Hankins GD, Spong CY, et al. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol 2008 Sep;112(3):661-6. PMID: 18757666.
- Macones GA, Hankins GD, Spong CY, et al. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. J Obstet Gynecol Neonatal Nurs 2008 Sep-Oct;37(5):510-5. PMID: 18761565.
- Perinatal Quality Foundation. Fetal Monitoring Credentialing. https://fmc.perinatalquality.org. Accessed May 9, 2016.
- GE Healthcare. Electronic Fetal Heart Rate Monitoring: Definitions, Interpretation, and Management. Clinical Education. http://www3.gehealthcare.com/en/Education/Clinical_Education/Electronic_Fetal_Monitoring. Accessed May 9, 2016.
Slide 22: References
- Association of Women's Health, Obstetric, and Neonatal Nurses. Education. http://www.awhonn.org/?Education. Accessed May 9, 2016.
- NICHD Definitions and Classifications: Application to Electronic Fetal Monitoring Interpretation. National Certification Corporation Guidance. NCC Monograph, Volume 3, No. 1, 2010. http://www.nccwebsite.org/resources/docs/final_ncc_monograph_web-4-29-10.pdf. Accessed May 9, 2016.
- National Certification Corporation. Electronic Fetal Monitoring. http://www.nccwebsite.org/Certification/default.aspx. Accessed May 9, 2016.
- Advanced Practice Strategies. GNOSIS for OB. http://www.aps-web.com/gnosis-for-ob/. Accessed May 9, 2016.
- Ciccone K, Christakis CR, Mathis A, et al. Partnership Improves OB Safety in New York State. Patient Safety and Quality Healthcare. July/Aug 2012. http://www.psqh.com/analysis/partnership-improves-ob-safety-in-new-york-state/. Accessed September 19, 2016.
- Andrews J, Likis FE, Sathe N, et al. Perinatal Safety Intervention Programs: A review of the literature. Prepared by Vanderbilt University Medical Center under Contract No. HHSA290201000024I, TO #3 Rockville, MD: Agency for Healthcare Research and Quality; February 2012.
- Heelan L. Fetal monitoring: creating a culture of safety with informed choice. J Perinat Educ 2013 Summer;22(3):156-65. PMID: 24868127.
Slide 23: Disclaimer
Every effort was made to ensure the accuracy and completeness of this resource. However, the U.S. Department of Health and Human Services makes no warranties regarding errors or omissions and assumes no responsibility or liability for loss or damage resulting from the use of information contained within.
The U.S. Department of Health and Human Services cannot endorse, or appear to endorse derivate or excerpted materials, and it cannot be held liable for the content or use of adapted resources. Any adaptations of this resource must include a disclaimer to this effect.
Reference to any specific commercial products, process, service, manufacturer, company, or trademark does not constitute endorsement or recommendation by the U.S. Government, HHS, or AHRQ of the linked Web resources or the information, products, or services contained therein. The Agency does not exercise any control over the content on these sites.



