During diagnostic reasoning, most clinicians apply a variety of cognitive techniques to arrive at a diagnosis. However, surprisingly little research has been done when it comes to causally establishing that high levels of cognitive load may lead to worse diagnostic accuracy. Although not explicitly stated in the literature, this situation is likely due to the difficulty of objectively measuring cognitive load because it inherently occurs in the internal cognitive environment.
As discussed below in the “Measures of Cognitive Load” section, cognitive load cannot be directly visualized and cannot be easily measured with objective tools. Rather, most measurements rely on subjective retrospective tools such as self-reported questionnaires or use objective proxies such as heart rate variability to infer amount of cognitive load. However, two areas that do have some evidence for causality between increasing cognitive load and decreasing diagnostic accuracy are cognitive overload and dual-process thinking.
Cognitive Overload
Cognitive overload occurs when working memory becomes overly burdened, leading to a decreased ability to learn, accurately process information, and execute performance-based tasks effectively.11 Although cognitive overload can occur in many settings, it is most often caused by information overload, multitasking and interruptions, and environmental threats.20
Information overload can occur when a clinician is forced to process excessive or unnecessary information. Within healthcare, this overload can take many forms but can most easily be divided into pushed (passively given to the clinician) and pulled (actively sought by the clinician) information.20
Pushed information is information over which the clinician has little control, such as electronic data, including vast amounts of sometimes poorly organized or redundant EHR data, electronic messages, and information from the patient and other healthcare workers. Pulled data includes information being actively sought, such as the same information streams that produce pushed data, but also include other avenues of research, such as books and online databases.
Pushed and pulled data can contribute to both intrinsic and extrinsic load. When the data are overwhelming, poorly organized, or irrelevant to the primary task, extrinsic load will disproportionately increase, resulting in less intrinsic load capacity to dedicate to the task at hand. In one study, a novel EHR interface designed to minimize extraneous data in a critical care setting reduced subjective workload scores, time for task completion, and number of cognitive errors associated with the assessment of a theoretical bleeding patient.21
Multitasking and task switching can also lead to cognitive overload and result in diagnostic errors.22 When a clinician is interrupted or asked to perform two simultaneous tasks extraneous to their primary task, they have to process information unrelated to the primary task, which increases overall cognitive load (in this case, via an increase in extrinsic load).
In some cases, the clinician has to set aside information being used for their primary task to increase working memory reserves for the secondary task. Switching back to the primary task requires both remembering to return to the task after the interruption and efficient retrieval of all information previously being used for the initial task. In one study of 18 emergency department healthcare workers, only 87 percent of interrupted clinical tasks were resumed after the interruption.23 In another simulated study with 10 intensive care unit nurses, interrupted tasks were temporarily or permanently forgotten 5.5 percent of the time.24
If information is not retrieved with a high degree of accuracy, it can also lead to errors.25,26 In one study, radiology residents had a 12 percent increased likelihood of a diagnostic error when receiving just one phone call above the average baseline number of calls.27 Further complicating this concept is that some interruptions are more worthy of a clinician’s time than others, such as interruptions related directly to the patient at hand or a critical update related to a different patient. However, clinicians have limited ways to decide whether a particular update, alert, or new piece of data is worth interruption at any given time; all distractions happen equally.
While multitasking will always be part of a clinician’s job, the ability to triage interruptions is critical. If clinicians cannot selectively engage with interruptions, cognitive overload will occur if too much irrelevant information is presented.26
Finally, the environment itself can contribute to cognitive overload. Clinical environments can be auditorily and visually stimulating. Alarm fatigue is widely acknowledged to be a significant patient safety concern,28 and frequent alarms result in a large amount of extrinsic cognitive load.29 Chaotic and loud environments in emergency rooms can lead to ineffective patient handoffs and may negatively impact patient safety and diagnostic accuracy.30 Poorly integrated and visually complex clinical decision support systems, rather than assisting in diagnostic accuracy, can instead lead to cognitive overload and inaccurate decision making.31
Hospital environments are uniquely suited to benefit from information ergonomics,32 especially as it applies to optimizing the cognitive environment, but so far this area of study has been underemphasized.
Cognitive Load and Dual-Process Thinking
Cognitive load also directly impacts dual-process thinking. The dual processing model of cognition posits two main types of thinking processes. Type 1 cognition is fast, intuitive, and easy, while type 2 cognition is slow, analytical, and effortful. Type 1 processing relies on intuition and patterns to formulate a rapid diagnosis. In a fast-paced healthcare environment, this type of processing is needed for efficient and effective healthcare delivery.33
Type 2 processing is required when a clinician has less clinical experience, such as during medical school or in the earlier years of training; when a complex, unusual, or ambiguous clinical problem arises; or when a common clinical condition does not evolve as expected.34
One type of processing is not necessarily better than the other. It may make intuitive sense that more rapid and frequently heuristic cognition is more error prone. But type 1 thinking is not universally associated with worse diagnostic accuracy,35-38 especially among more expert attending clinicians who have spent years building their mental schemas and knowledge base. In addition, type 1 and type 2 processing are often both needed during a clinical encounter.
Cognitive load directly affects clinicians’ ability to engage in dual-process thinking. The ability to come to the correct diagnosis, especially in the face of diagnostic uncertainty or an evolving clinical course, is predicated on the ability to quickly and appropriately switch between type 1 and type 2 cognition. However, if working memory is overloaded by extrinsic distractions, the clinician will face cognitive overload and may be unable to switch between type 1 and 2 cognitive processes.13,39
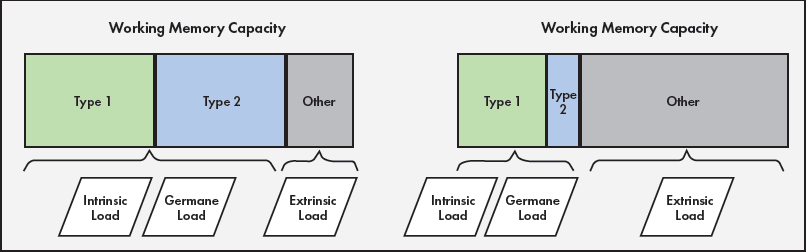
Figure 2 illustrates how cognitive load affects cognitive processing. Working memory has a finite capacity. If extrinsic load is low, both type 1 and type 2 thinking can occur. Conversely, if extrinsic load increases, as can occur with a chaotic environment, distractions, unsafe workload, and multitasking, the ability to engage in more effortful type 2 thinking decreases due to the cognitive bandwidth required for this type of thinking. Instead, the clinician will rely on more intuitive type 1 thinking, which can increase the risk of errors in situations that necessitate parallel type 1 and 2 processing or a transition to type 2-predominant processing.
Figure 2. The impact of cognitive load on type 1 and 2 thinking
Clinical Example
The impact of cognitive load on diagnostic reasoning can be explored by returning to the example of a hospitalist admitting a patient with congestive heart failure. As the patient arrives in the emergency department, the hospitalist attempts to look up whether they might benefit from newer guideline-directed medical therapy. But the hospitalist must sift through primary research, meta-analyses, and clinical decision support tools, none of which are integrated within the EHR (information overload).
Next, the hospitalist tries to bring up the patient’s record but finds that the patient has duplicate charts and the hospitalist has to toggle between the charts to review baseline lab values and prior diagnostic workups (task switching). Concurrently, they receive multiple electronic messages that they read while listening to the patient describe their symptoms (multitasking). As the hospitalist becomes more cognitively overloaded, they rely more heavily on type 1 thinking to rapidly process the elevated troponin, chest x ray with diffuse haziness, and lower extremity edema.
The hospitalist diagnoses the patient with congestive heart failure. However, they fail to consciously process that the patient mentioned a new cough, do not notice the patient’s slightly elevated temperature, and discount the mildly elevated white blood cell count as reactive. Because of limited working memory capacity, they do not switch into type 2 thinking and miss that this patient has multifocal pneumonia in addition to heart failure.
In this example, the presence of overwhelming extrinsic load and cognitive overload leads to a diagnostic error. This error results in a missed diagnosis and lack of treatment for pneumonia, which can progress to more serious conditions, including respiratory failure and sepsis.



