Scoping Review
The database search yielded 4,080 nonduplicative publications, most of which were excluded based on review of title and abstracts. We reviewed the full texts of 205 publications and excluded an additional 80, leaving 125 publications that met our criteria for the review. A list of included publications is available separately.
Characteristics of included studies are displayed in Tables 1 and 2. The United States was the most frequent country of origin (n = 84, 67%). Most studies described data collected from patients and families; fewer collected data from healthcare professionals (including physicians, nurses, and others) or both (Table 2). With the exception of six literature reviews, articles reported original data collection. Surveys and interviews were the predominant modes of data collection (Table 2).
We identified no obvious temporal trends in the number of qualifying studies over the 7 years we examined (Figure 1). Notably, 20 articles described studies at cancer centers or focused on oncology-specific test results.7-26 Three of these pertained to the pediatric oncology setting21,22,24 and one review focused on patient portal use in people with cancer.14
Table 1. Included studies by country
| Country | Number of Studies |
|---|---|
| United States | 84 |
| Canada | 10 |
| United Kingdom | 8 |
| Netherlands | 6 |
| Sweden | 4 |
| Iran | 3 |
| Finland | 2 |
| Denmark | 2 |
| Australia | 1 |
| Belgium | 1 |
| Italy | 1 |
| New Zealand | 1 |
| Israel | 1 |
| Spain | 1 |
| Total | 125 |
Table 2. Types of original data collection methods by data source
| Data Source | Survey | Interview | Record Review* | Other Observational Method |
|---|---|---|---|---|
| Patients/families | 55 | 27 | 32 | 7 |
| Healthcare professionals | 7 | 4 | 0 | 1 |
| Both | 7 | 5 | 1 | 2 |
| Total | 69 | 36 | 33 | 10 |
* Record review refers to use of any existing data source maintained by a healthcare organization, including patient portal usage logs and electronic health records.
Note: Totals exceed number of studies due to studies with multiple data collection methods.
Figure 1. Number of included studies (excluding literature reviews) by year of publication and data source

Demographic trends and disparities in portal-based test result access
Studies identified a general trend toward greater adoption and use of patient portals to access test results over time. One of the most robust samples in the literature was from the Health Information National Trends Survey (HINTS), a U.S. nationwide survey of health information technology use. Data from the fifth wave of HINTS (February-June 2020) indicated that 39 percent of the national sample had ever used a patient portal, and of that subgroup, 87 percent had viewed test results through a portal.27 Forty-two percent of respondents indicated that they had used an electronic device to check test results in the past 12 months.28
Increased access to test results through patient portals has not been proportional across all populations.29 Racial and ethnic disparities in access to data in patient portals is well documented.10,20,30-34 For instance, in a study of more than 40,000 adult patients with cancer, one-third of Black patients viewed any test results released through the patient portal during a 5-year period, compared with more than half of White and Asian patients.10 Several factors have been associated with lower rates of patient portal activation and test result access through patient portals:
- Older age.33,35-37
- Lower educational level.38
- Lower health literacy.35
- Public versus private insurance.39,40
- Unmarried status.41
- A primary language other than English.20,30,33,42
A few studies found that female gender predicted a greater likelihood of viewing test results through a portal.30,32,33,40,43
Patterns of patient portal use for test result communication
Fifty-three studies analyzed self-report data and portal usage log data to understand trends in use of portals to access test results (Appendix B). The sampling frame for most of these studies was an ambulatory population at a single health system or facility. A smaller number of studies focused on the hospital or emergency department setting.
Twenty-nine studies analyzed data from patient portal usage logs maintained by the researcher’s health system. For instance, studies have found that 5 percent of all outpatient imaging results44 and 9 to 12 percent of lab and imaging results from emergency room visits32,33 were subsequently accessed via patient portal. Studies indicate temporal trends toward increased use of patient portals to access test results over the past several years, especially since implementation of the Cures Act,10,29,33,45 and decreased time to view results after they are made available.10,40
Fifteen studies quantified the frequency of using a portal to view test results compared with other portal activities or features. In most of these studies, accessing test results was found to be the most frequently used or second most frequently used feature.14,15,17,18,31,38,41,46-53 Surveys of patients suggest that viewing test results was also one of the most valued features of patient portals.37,46,47,54-56
Patient attitudes, perceptions, and behaviors related to automatic test result release
Surveys and interviews of patients highlight several perceived advantages of accessing test results through portals, including:
- Speed and time saving,7,57-59
- Ability to access information on demand.56,60
- Greater feeling of being engaged, informed, and involved in one’s own care.57,60-63
- Greater endorsement of patient activation.50
- Less need to rely on staff.64
- Perceived safety.57
Accordingly, studies indicated that most patients have favorable views and preferences toward immediate access to test results once they are available.11,47,59,64-67 For example, in one study of more than 4,000 patients, when given the option of a 1-day versus 7-day delay to view laboratory results, 77 percent opted for the shorter delay. In the same study, the authors noted that less than 10 percent of patients changed their preferences, but among those who did, most changed from a longer to shorter delay.67
Despite patient preference mostly favoring immediate access to test results, studies also indicate that most patients want to discuss their results with clinicians. Preferences for the timing of those discussions, relative to accessing results through the portal, were influenced by the sensitivity/urgency of the test result and the wait time to discuss with the clinician.7,11,19,26,65,67-69 This general pattern of findings was summarized by the authors of a study of portal use among oncology patients: “the portal was a welcome alternative if either a phone call or in-person meeting caused any delay in receiving results.”7
Perceived disadvantages of receiving test results through portals included concerns about privacy and confidentiality59,70 and concerns about missing details or context that might have been gained through a face-to-face encounter with the clinician.60 In one of the larger interview-based studies (n = 95), most respondents reported having received test results in a portal without any explanation or way to interpret those results.71 However, in a large survey of patients recruited from four academic medical centers, 87 percent of patients who viewed test results through the portal indicated that a clinician eventually contacted them about their results.66
Emotional reactions, especially anxiety and worry, were frequent outcomes of interest in studies of patient experiences. Giardina, et al., reported that more than twice as many patients experienced a negative emotion after using the portal to access an abnormal test result compared with a normal result.71 On the other hand, using the portal as a means of reassurance and anxiety management (i.e., reducing the anxiety of waiting for results) were themes in several studies.7,21,25,57,72
Turer, et al., reported that most patients reported decreased worry or no change in worry when viewing test results before discussing with a clinician, whereas only 5 percent of patients felt more worried when they viewed test results in the portal before speaking with a clinician.73 Fewer studies have examined other negative emotions, such as anger and disgust. A content analysis of patient-generated messages in response to test results suggested that more messages reflected negative emotions after implementation of immediate test result release.74
We found little information about specific adverse events related to viewing test results in the portal. One study compiled problems and adverse events from a single institution using patient complaints, staff event reports, information technology help desk queries, and a survey of clinical staff. Patient-reported concerns were chiefly related to access barriers, discovery of inaccurate information in the medical record, and technical problems. Clinician- and staff-reported concerns focused on patient distress, lack of provider availability near the time of test result release, and patient-identified errors in the medical record.72
Portal design and usability
Problems with the usability of patient portals were a frequent finding in the literature. The predominant barrier to usability for patients was difficulty with interpretation of medical terminology and lab values.46,75-84 In usability evaluations of specific interfaces, lower health literacy was associated with more usability difficulties.80,85 In experimental and quasi-experimental studies, visual displays and verbal or video explanations of test results seemed to influence patient interpretation and engagement.86-89
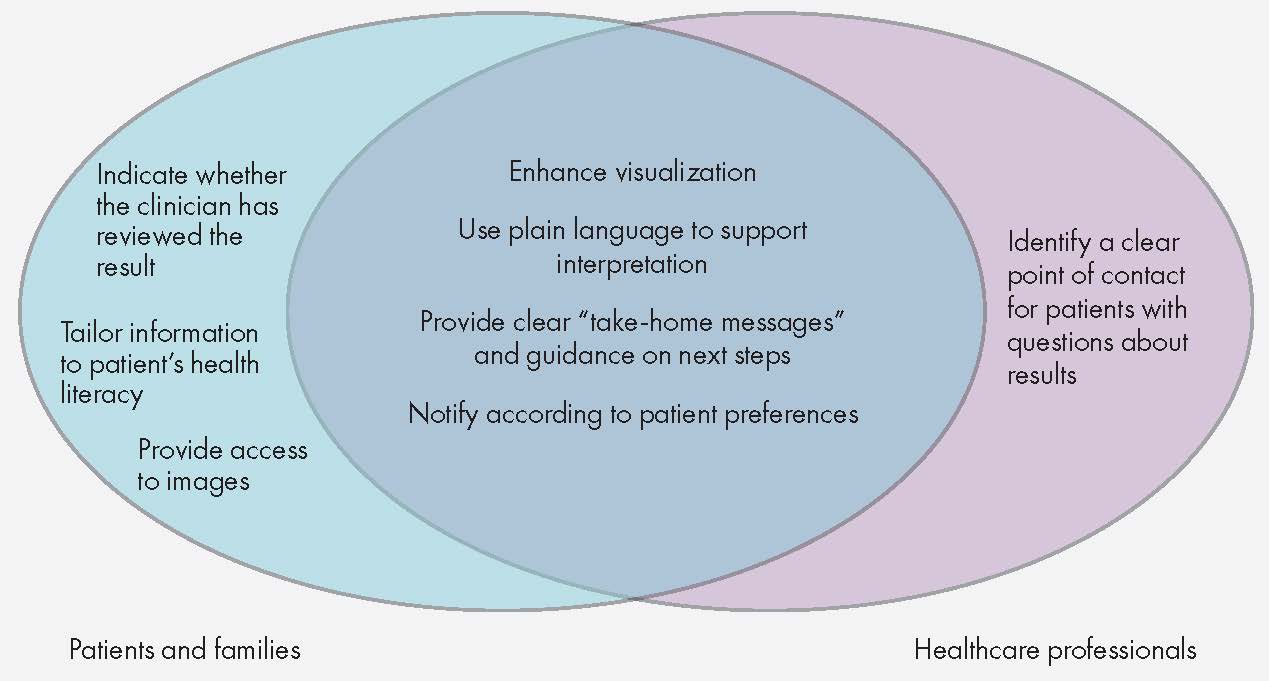
Twelve studies solicited suggestions and feedback from patients and physicians to improve the design of test result interfaces.13,47,60,70,84,90-96 Themes overlapped considerably between patient and physician suggestions for improvements across studies (Figure 2).
Figure 2. Patient- and physician-generated suggestions to improve test result communication in patient portals
Sixteen studies described various approaches to assessing the design and usability of interfaces to display test result data using prototypes or “mock-up” scenarios. These studies included observational and experimental designs, and they used a variety of usability testing methods such as process mapping, cognitive interviewing, qualitative interviewing, and task completion paradigms. Patient-oriented enhancements, such as lay explanations of test results and improved visualization formats, were found to be helpful and perceived positively by patients.
Tested interfaces and formats included:
- New patient portal designs and prototypes.55,62,92,94
- Mock lab test reports in a format similar to a currently implemented system.97
- Novel patient portal message formats with explanations of results enhanced by graphics, additional written interpretations, or videos.88,89
- Visual displays of laboratory test values and reference ranges as an alternative to numerical data alone.76,85
- Patient-oriented reports to explain lab and radiologic findings in lay language to accompany the standard report.13,25,86,98,99
- Patient-oriented reports to explain genetic test results.87,100
Healthcare professional attitudes and perceptions related to automatic test result release
Twenty-eight studies elicited the attitudes of clinicians, nurses, and other healthcare professionals (e.g., pharmacists,101 social workers,102,103 informatics professionals104) on their attitudes and beliefs about releasing test results to patients through portals. In general, clinicians held less favorable impressions of immediate test result access compared with those of patients.11,12,47,105
Positive perceptions of direct test result access included expectations that this practice would improve patient engagement in care,106 prompt faster discussion of results by the care team,106 and improve reliability and efficiency of test result communication.107 Negative perceptions included concerns about distress or adverse emotional reactions to test results and increased workload.7,11,31,47,61,95,101,106,108,109 A few studies identified healthcare professionals’ concerns about privacy and confidentiality,102,105 including two studies about perceived limitations and technical constraints of proxy access for adolescent patients.104,110
We found only two prospective studies that measured health professionals’ attitudes both before and after implementation of the Cures Act. One of the studies, focusing on clinicians in a neonatal intensive care unit, found that both positive and negative expectations decreased pre- to postimplementation.103
The second study surveyed oncology clinicians over 1 year and found that the percentage of respondents who opposed immediate release of test results decreased from 82 percent to 58 percent the following year.8 High attrition makes it difficult to interpret these findings, but attitudes toward immediate release of test results appeared to become somewhat more favorable over time, possibly due to fewer than expected negative outcomes after the policy was implemented.
Subjective assessment of changes in workload has been mixed,12,101 and one study suggested that using the portal to report test results could streamline work in some situations.107 Three studies provided objective data to quantify workload related to portal-based release of test results. One of these examined data at the patient level (N = 439) and found that patient portal activation status was unrelated to the average number of telephone calls about test results or medications.111
Another study examined data at the practice level (more than 3 million test results distributed among approximately 300,000 patients over 16 months). The researchers found that the number of patient-generated messages sent to providers after viewing test results doubled after implementation of immediate test result release.112 Finally, findings from an academic dermatology practice suggested that the volume of patient-generated messages per provider increased by 11 percent after implementation of the Cures Act.74
Considerations for implementation
Several years after implementation of the Cures Act, a few studies have focused on implementation of immediate test result release. These have focused on two key issues: (1) the ability of patients to “opt out” of test result notifications and (2) challenges of establishing proxy access for minors and those who rely on caregivers to use the patient portal on their behalf.
With regard to the first issue, a qualitative study of 27 patients and 29 clinicians in the cancer care setting found that both patients and clinicians favored flexibility in implementing immediate release of test results. Both groups shared a belief that delayed release might be beneficial to certain patients and in certain situations and that decision making about test result communication should be more individualized.
Other studies have reported similar concerns about customizing test communication,95,102 but how to operationalize this flexibility within current systems is less clear. A study in one academic medical center examined the impact of a policy to change the default patient notification settings for new test results, effectively making notifications an “opt-in” rather than “opt-out” feature. While the impact on patient-generated messaging was marginal, the authors noted that within the first month of this policy change, fewer than half of patients (42%) changed back their preferences to be notified each time a new test result was available.
Other studies have noted the importance of preparing patients in advance for the possibility that they might see their test results before a clinician has had an opportunity to review them.103
The issue of proxy access presents several challenges. Both minors and older adults may be concerned about privacy when sharing access to their test results with a parent or caregiver.113 Different state laws and organizational policies create variation in how proxy access is implemented.
Patients want more granular control over proxy access (e.g., restricting access to certain information), but most systems offer only an “all or nothing” approach to a proxy user’s access to information, in part due to EHR limitations.104,110 Organizations have adopted a variety of strategies to balance access and privacy for patients who share access to test results with a parent or caregiver.110
Subject Matter Expert Interviews (Qualitative Evaluation)
We identified five main themes from interviews with SMEs. Below, we describe each theme and subtheme, with representative quotes included to illustrate and contextualize these topics.
Clinicians’ concerns about immediate test result release
A dominant theme was clinicians’ concerns about the impact of the Cures Act. Concerns about workflow and potential adverse events echoed themes from recent literature; however, clinicians contributed additional insights about interoperability concerns, potential effects on patient engagement in care, and strategies to mitigate harm.
Disruption in clinician’s workflow/workload: Four participants shared concerns about the increase in patient queries and messages and mentioned a lack of workflows to accommodate the corresponding increase to clinician burden and inbox overload.
- We get a lot of requests like, “Why is my result one point above the normal range?” (R9)
- Ambulatory teams may have a harder time in terms of an increased volume of people reaching out with questions that then require a significant amount of clinical decision making, clinical communication… (R2)
- We did see quite a lot of increased patient-initiated messaging…potentially concerning is that we don’t have fantastic workflows or reimbursement for providers to respond to those types of messages… (R6)
- I think this is what’s most stressing [to] physicians. It’s knowing that we’re all busy, and sometimes as much as we would like to, the system may fail us.… The patient may reach out and the service is not gonna reach out to me for days or hours…. These are system problems that must be addressed. (R3)
Participants were supportive of giving patients the autonomy to specify their preferred means of test result delivery. However, they shared concerns about implementing these communication preferences.
- Patients should be able to say, the route of delivery…. But we just can’t manage that by workflow. We can’t really manage that type of multiple different dissemination routes. (R6)
- So, it’s whoever is going to interact with the majority of these inbox messages that needs to really understand what’s the most efficient way to communicate back. As long as that’s the patient’s preferred method of communication. (R3)
Interoperability: Although less directly related to the issue of immediate test result availability, several participants spontaneously raised concerns about interoperability of EHR systems.
- So, there is a lot of work being done… to try to advance interoperability so that folks can readily exchange health information…. And this takes a tremendous amount of resources to get from where we are to where we want to be. (R5a)
- I guess with regard to telehealth, the challenge there I see is more so in terms of interoperability. How can we best document a telehealth encounter and get patients the record of that encounter in maybe a standardized way that can be shared if they so choose with their provider…. And I’d say that’s kind of hit or miss depending on the telehealth provider. (R4)
- And the other thing that I’ve learned is a lot of my patients don’t get their test results in our system. They get them somewhere else… I think it’s information blocking at the vendor level, not at the provider level, and yet who takes the heat? Often the delivery system does…. That’s what I hear. They’re [patients] very frustrated. I can’t see [their] results. They live 100 miles away. They don’t wanna come in. I understand that. They wanna go somewhere else to their lab or they go to another clinic. And I am not able to help them because I have to wait for things to get faxed to me. (R9)
Adverse outcomes related to test result release: Participants in clinical and operational roles acknowledged concerns among clinicians that releasing certain results could upset or confuse patients, possibly leading to harm. Participants identified few known reports of adverse events ranging in severity that were related to test result release in their systems.
In one case, an adverse outcome led to a change in how patients were informed about abnormal test results (specifically, cancer); however, the incident was related to mailed correspondence and not a patient portal. Another respondent expressed concern about insufficient response to two known adverse outcomes at their organization.
- We haven’t had many [reports of adverse outcomes]. We probably had one since this came up, so there might be an order of magnitude higher than that… but it has not been a recurrent concern that at least gets reported. (R1a)
- So not everyone read the memo, and we’ve had maybe a handful of upset physicians and patients over the several years that we’ve been live. (R3)
- I’m hearing almost nothing…. A single case escalated.… When a single case gets escalated after more than 2 years and thousands and thousands of patients, that is likely an exception that proves the rule that this is generally pretty good. (R7)
- I’m aware of one issue where we had a letter… that indicated that they had terminal cancer. It was written by the provider and there was an adverse outcome, a sentinel event… it changed the process at the facility. (R8)
- This isn’t happening all the time for all patients. This is a pretty exceptional thing, but those are the two [known adverse events] that came before our committee and they weren’t, in my view, respected as they should have been. (R9)
Relatedly, participants highlighted that each patient is unique with different abilities and resources to cope with bad news.
- All patients are different, all patients have different levels of coping skills. They have different mental health backgrounds… I do think you have to be very careful with specific populations… (R8)
- I’ve had people tell me they found out they had cancer via MyChart, and what those patients have told me is that the opportunity to get the news in a private space, to cry, to grieve, to sort of collect themselves with their family, come up with questions, and then use the next visit as a productive step forward, allowed them to feel more empowered than otherwise. But I think anybody who works clinically knows that that story about one patient is a story about one patient and that individual preferences are overwhelmingly the most important thing here. (R2)
Two participants noted that real-time access to test results might affect patients’ decisions to continue care.
- In emergency medicine, we worry about… people leaving before the end of their encounter because they see they have a relatively low acuity result and they get up and leave… (R2)
- Genetic testing results are complicated… it may not be as simple as you have or don’t have this condition… results are three pages long… a very short summary of those results, which doesn’t have the nuance that the full results do, is sent because it has to be released. The patient says, “Now I have my results. I don’t need to have that appointment and I will cancel it.” (R9)
Participants noted several ways to mitigate risks to patients who could be vulnerable to adverse outcomes after disclosure of test results. These included proactively identifying patients known to be at risk for self-harm, blocking information in situations that meet the Cures Act’s exception criteria, and maintaining document types that are not released to the patient.
- Within our system, we have a patient record flag that notes if a veteran is high risk for suicide… (R8)
- The Cures Act does have some, some language about immediate harm to the patient, and that one might actually qualify… (R6)
- With notes we have the option when we release them… we have the option to say in this particular case, the benefits to the patient are less than the risks, and that’s a rare thing. But sometimes those circumstances arise and I think we should [block results]. (R9)
- We also had to do some training about how do you prevent release of something that you think may cause harm.… So, the way we approach this in our Cerner [EHR] environment is by document type. And the only document type that we decided not to make available via the portal is this secure document type… and we recommend only securing the portion of your note that may cause significant harm. (R3)
Some participants nonetheless advocated for greater discretion for clinicians to release test results to patients.
- I still think it would be great to have a graded release of information, where if it is a life-changing result… the provider has some control over how that news is delivered to their patient, along with the resources and support that they need. (R8)
- What I envision is the pendulum is gonna swing back a little bit. We were way over to the “no release, let the doctor call you in 2 weeks.” And now it’s immediate. And I think it’s gonna take moderation. And I kind of wished that moderation was part of the initial package. (R9)
Implementation and training issues
A few participants agreed that their organizations implemented the Cures Act with little guidance for clinicians despite the “culture shift” this change might have entailed. One participant mentioned that training focused more on compliance than optimal patient care practices.
- There was a lot of education about the regulation and what it meant and what you could do and what you couldn’t do. And more specifically, the concern was that people would use the block function and then the institution would get cited for information blocking… I’m not aware that best practices exist on how to disclose that you may see your results before I do… I don’t think we got any training. (R2)
- It’s [immediate release of results to patients] not something we’re very much used to culturally. And you know, there’s a lot of objection to it at first. Now it’s required. (R9)
- We put together a number of tip sheets.… We put a few different educational modules on [training website]. Executive leadership decided not to make it required. (R7)
Entrusting patients to take ownership of their test results
Patient preference: Most participants (n=5) supported the idea of giving patients the autonomy to decide how they want their test results to be released or how they want to be alerted and if they want to add a proxy to access their health information. Two participants noted that a limitation of current systems is a lack of granular control over how certain sensitive test results are released to patients and proxy users.
- I think we need to continue to educate people that these are their data. These aren’t our data, right? We’re safeguarding it for them and we have some responsibilities around it… but really, it’s the patient’s data. So, I think empowering people to know that it’s theirs and they can do what they want with it is piece number one. (R2)
- Caregivers can have access to records if the veteran allows it, and sometimes you know it’s critical. (R8)
- It’s the ability to choose between immediate release of everything with the ability of setting exceptions. Meaning I wanna see everything immediately, but for some reason… let’s say my tumor marker… I really would rather not see the result until my physician reviewed it… Being able to add a tickler to that. (R3)
- We have a really difficult situation… that Epic has its patient portal set up in such a way that you either have to share everything that you see with your proxies or none of it with your proxies… There’s no mechanism for that kind of granular control over whether you or your proxy or both can see. (R7)
Two participants highlighted the use of test result notification settings in patient portals to make test result communication more patient centered. Another noted that many patients have not set preferences for test result notifications because they are not fully using the portal’s settings.
- …we shouldn’t have a one size fits all policy. Not everybody wants to be immediately notified about these. Some people actually do want to talk to their doctors about it or want to not receive a push notification, or just, like, the next time I log in, I’ll take a look. (R6)
- One of the things we did very early on… was to turn off the default notifications… and we heard loud and clear from our patients that, we want access, but we don’t want you to force it on us. I was very skeptical of this at the beginning, and it was really our patients that changed my mind. (R7)
- I think the bigger issue is lack of awareness. Having changed them [test result notification preferences] myself, it’s three, I think three menu layers deep, pretty far down through a phone [smartphone app] interface. (R2)
Patient Education and Precounseling
The topic of patient preparation frequently came up during interviews where participants in clinical and operational roles (n=6) proposed that clinicians set expectations with patients at the time of test ordering. One participant also suggested providing reliable education materials at the time of release to aid interpretation.
- We have seen an uptick in the number of conversations about… having conversations beforehand, and at the time of ordering or at the time of the initial consult… what is best practice to inform where data may be sensitive and really trying to achieve that engagement… this is a conversation which will evolve over years, but… the Cures Act, I think, spurred that part of the conversation and really the optimization. (R1b)
- …making sure that when you supply those results in an automated form that you have… the resources that the provider would want that patient to have so that they’re not Googling things on their own, but that you have a… respected resource that can help them understand what those results are… (R8)
- I think it’s about spending a minute before the test, [at the] time of ordering, in preparation for what we are going to do with the results or what the results might be. And I’m going to be there for you… it may take some time to connect, but I’m gonna be there with you to have a conversation. (R3)
- I have concerns about a patient opening up their portal account and learning about a new diagnosis of cancer… I’m not saying the way to deal with that is to go back to the delay of test results, but it is possible that the way to handle it would be far better patient precounseling… make sure that people understand that it, you know, it could be this… in which case the following steps are appropriate. (R6)
Suggestions for optimization of test release communication
Participants recommended several system changes and to enable patients to have access to all their medical data, safely and in the modality they prefer to receive it (Table 3).
Table 3. Subject matter experts’ recommendations for practice
| Recommendation | Supporting Quote | Participant # |
|---|---|---|
| Open access to care team | “…open office hours or something where the patient, if they got the results could call back… to the provider or the care team to talk through them.” | R8 |
| Engaging the wider care team when necessary | “It’s important to coordinate that care… work with the care teams [e.g., mental health professionals] to ensure that any resources or support that that [patient] needs is put into place.” | R8 |
| Adapting messaging for different patient populations | “We have a very diverse population… so you have different communities that have vastly different demographics… social constructs, different cultures, that need to have that communication piece developed in a way that is most effective for that particular community.” | R5a |
| Setting expectations and preferences at the time of test ordering | “I think step one is to establish best practices for precounseling patients and for making notification preferences easier to set up…” | R2 |
| “It would be good to figure out how to build that [precounseling] into the clinician’s day and reimbursement structure so that they can actually do a good job of this.” | R6 | |
| “You need to have good education for patients in the form of precounseling and supporting documentation…” | R7 | |
| EHR vendor standards | “…standardizing what the vendors put out there to empower patients to clearly document their wishes…” | R3 |
| “I’d love to see a federal regulation that requires that vendors build patient portals in such a way that it… gives patients granular control of what they share with proxies.” | R7 |



