All members of healthcare organizations play a vital role in patient safety and quality, but healthcare leaders have a unique responsibility for ensuring that all patients receive patient-centered, safe, effective, efficient, equitable, and timely care. This care includes addressing both established and emerging safety concerns, such as diagnostic errors, which can involve up to 12 million patients annually in U.S. ambulatory settings alone and contribute to death for up to 80,000 patients in U.S. hospitals annually.1
Evidence suggests failures in diagnosis plague the general patient population across all settings of care. Errors involve common conditions and nearly half of them have potential for patient harm. This staggering estimate is not surprising, given that the diagnostic process is complex, and diagnostic accuracy and timeliness are not solely the domain of clinicians,2 but also depend on system-level factors. Leaders occupying roles ranging from individual shift or practice managers to members of the executive team will be critical in meeting the challenge of improving diagnostic safety.
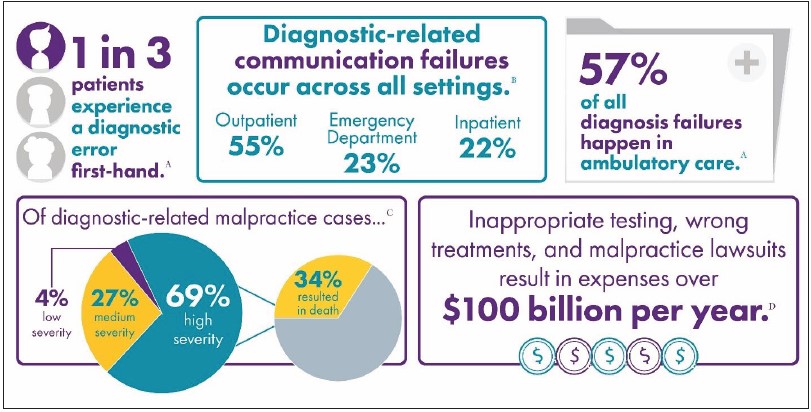
The nature and magnitude of diagnostic errors and their tangible associated costs are drawing the attention of regulators, payers, and patients. Similar to other patient safety issues (e.g., healthcare-associated infections, or HAIs),3 in addition to the moral imperative for preventing diagnostic errors, a strong case can be made for return on investment for improvement efforts, as illustrated in Figure 1.
Figure 1. Location and Impact of Diagnostic Failures
- Balogh EP, Miller BT, Ball JR, eds. Improving Diagnosis in Health Care. Washington, DC: Institute of Medicine; 2015. https://www.nap.edu/catalog/21794/improving-diagnosis-in-health-care. Accessed June 1, 2021.
- 2015 CRICO Strategies National CBS Report: Malpractice Risks in Communication Failures. https://www.rmf.harvard.edu/Malpractice-Data/Annual-Benchmark-Reports/Risks-in-Communication-Failures. Accessed June 1, 2021.
- Hoffman J, Raman S. Communications factors in malpractice cases. In: Communication Challenges. Cambridge, MA: CRICO; 2012. pp. 4-6. https://www.rmf.harvard.edu/-/media/Files/_Global/KC/PDFs/Insight_Comm_2012.pdf. Accessed June 1, 2021.
- Newman-Toker DE. Diagnostic value: the economics of high-quality diagnosis and a value-based perspective on diagnostic innovation. Modern Healthcare Annual Patient Safety & Quality Virtual Conference; June 17, 2015.
Healthcare organizations will undoubtedly face increasing scrutiny and accountability to address this urgent healthcare problem. Federal agencies are actively developing standardized ways to capture diagnostic safety events to guide improvement efforts. Public health advocates such as The Leapfrog Group and Hospital Compare are working on ways to represent organizational commitments to and capabilities in achieving diagnostic excellence4 and to convey this information in a meaningful way to patients and payers. Coalitions and researchers dedicated to improving diagnosis have created resources to address common organizational needs such as measuring diagnostic improvement opportunities.5,6
Meeting the diverse system-level challenges of diagnostic safety requires transformational leadership rooted in a growth mindset—a belief that individual and organizational capabilities can be improved with effort, effective strategies, and input from others.7 Confronting the challenge of diagnostic errors offers healthcare leaders the potential to improve patient care, enhance the work environment for providers, reduce costs associated with malpractice insurance and litigation, and position their organization as a market and industry leader. This brief provides an overview of how healthcare leaders can start to carry out the responsibility of improving diagnosis.



