Although slower than expected, progress in addressing patient safety issues has been made since publication of the Institute of Medicine’s seminal report To Err Is Human: Building a Safer Health System more than 20 years ago.8 National attention by quality and safety improvement organizations, Federal agencies, safety scientists, and scholars led to efforts to facilitate collaboration and coordination, disseminate evidence-based practices, and foster leadership commitment to the creation of learning health systems.9,10
Two decades of patient safety research have shown that improvement efforts work when they span multiple levels and roles within an organization,11 including healthcare leaders, clinicians, patients, regulators, policymakers, and purchasers. These lessons tell us that healthcare leaders need to play an essential role in preventing diagnostic errors, as they have with progress made in addressing other forms of preventable patient harm.
Leadership engagement is a critical driver of safety and quality improvement initiative success,12–17 such as mitigating HAIs, implementing patient safety teams, improving structured communication strategies, and normalizing the use of teamwork tools. Leadership contributes18 to both a learning system and local culture and consistently19 is essential to both staff engagement and successful patient outcomes.
Knowledge of the harms associated with missed, delayed, or inaccurate diagnoses is emerging. The science of diagnostic safety is maturing, and a more standard and pragmatic foundation for diagnostic improvement is beginning to take shape. Figure 2 (Safer Diagnosis Framework) illustrates how key leadership and management functions such as collective mindfulness, organizational learning, improved collaboration, and better measurement tools and definitions are central to diagnostic safety.
Despite the need, healthcare leaders have not been the target audience for much of the diagnostic safety improvement work to date, despite their central role in past safety and quality improvement successes. Therefore, the gap in leadership recognition, prioritization, and investment to address diagnostic safety is not surprising. Best in class diagnostic performance requires both clinical and administrative leadership,20 but clear guidance for leaders on this topic has been elusive.
Figure 2. Safer Diagnosis Framework for Measurement and Reduction of Diagnostic Errors19 (Sociotechnical Work System)
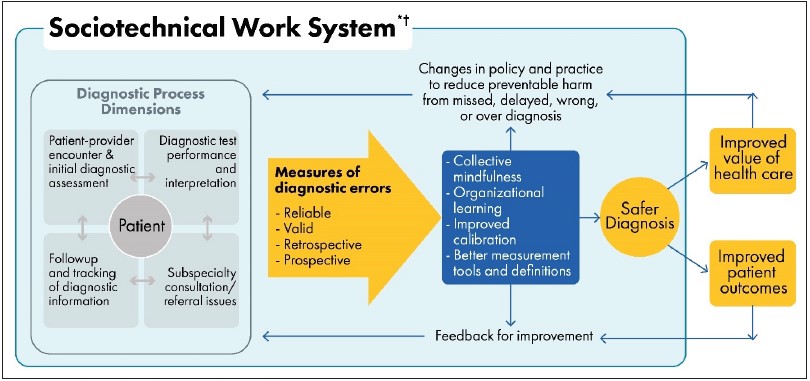
* Includes eight technological and nontechnological dimensions.
† Includes external factors affecting diagnostic performance and measurement, such as payment systems, legal factors, national quality measurement initiatives, accreditation, and other policy and regulatory requirements.



