Module 1: Preventing Falls in Hospitals—Slide Presentation
Slide 1: Preventing Falls in Hospitals
ADD Hospital Name Here
Module 1
Image: Cover of Preventing Falls in Hospitals Toolkit.
Slide 2: Ice Breaker
Describe an interesting fact about yourself.
Image: Photograph shows a goldfish jumping from one fishbowl to another to join other goldfish.
Slide 3: Compelling Reasons to Implement Program
- Falls are common.
- They are the most frequently reported incident in adult inpatient units.
- The rate of falls ranges from 1.3 to 8.9 falls per 1,000 patient days or bed days.
- Module 5 will discuss how to measure fall rates.
Image: Medical papers labeled “fall risk.”
Slide 4: Compelling Reasons to Implement Program

- Falls increase costs, which are associated with:
- Increased length of stay.
- Additional costs ($14,000 on average).
- Higher rates of discharge to nursing homes.
- Medicare won’t pay for increased costs due to injury from inpatient falls.
- Falls harm patients.
- 30% to 51% of falls result in injury.
- Many falls are preventable.
Image: Photograph shows a medical provider treating an injured knee.
Slide 5: Compelling Reasons to Implement Program
- Multicomponent fall prevention programs reduce falls.
- Systematic reviews* show that fall prevention programs result in statistically and clinically significant reductions in fall rates.
- A 27% to 31% decrease in fall rates was found.
Source: Miake-Lye IM, Hempel S, Ganz D, et al., 2013.
Slide 6: Are You Ready to Change?
- Do organizational members understand why change is needed? (Tool 1A)
- Is there urgency to change? (Tool 1B)
- Does senior leadership support this initiative? (Tools 1C, 1D)
- Who will take ownership of this effort?
- What resources are needed? (Tools 1E, 1F)
Slide 7: Practice Insight

Value of Pre-Assessment Tools
Image: Icon of binoculars.
Slide 8: Implementation Training Objectives
- Educate hospital leadership and Implementation Team on the Preventing Falls in Hospitals Toolkit to facilitate the change process in hospitals.
- Develop hospital-specific action plans for implementing a Fall Prevention Program using the Toolkit.
- Address specific challenges of preventing falls in your hospital.
- Use and adapt the tools and resources to implement the Fall Prevention Program.
Slide 9: Today’s Group Dynamics
- Your Implementation Team Leader (or the designee) will present assessments of your hospital’s current procedures and policies.
- Everyone here plays an important role.
- We encourage everyone to participate in planning activities.
Slide 10: Today’s Group Dynamics
- Parking lot” to capture your ideas:
- We’ll try to address your comments. We may need to address them later during the Implementation Phase.
- Much ground to cover today:
- We will follow the timeframe listed on the agenda.
Slide 11: Implementation Training
The Toolkit focuses on:
- Reducing falls during a patient’s hospital stay.
- Successfully negotiating a change process at your hospital.
Image: Puzzle pieces are labeled “assess readiness,” “manage change,” “implement practices,” “best practices,” “measure,” “sustain,” and “tools.”
Slide 12: Preventing Falls in Hospitals Toolkit
Toolkit Sections:
- Is your hospital ready for this change?
- How will you manage change?
- Which practices do you want to use?
- How do you implement best practices?
- How do you measure fall rates and prevention practices?
- How do you sustain an effective Fall Prevention Program?
Image: Cover of Preventing Falls in Hospitals Toolkit.
Slide 13: Toolkit Approach
- The Toolkit is focused on an interdisciplinary approach.
- This approach pulls staff members from many areas with needed expertise to address the problem.
- No clinician working alone can prevent falls.
- Fall prevention requires active engagement of multiple disciplines and teams that care for the patient.
Image: Photograph shows medical providers with patient.
Slide 14: Toolkit Approach
- The Toolkit includes accurate, evidence-based, and effective risk assessments that call for:
- Critical thinking and clinical judgment.
- Consistency in approach.
- Identifying and communicating risk at the earliest possible time.
Slide 15: Toolkit Approach
- The Toolkit focuses on optimizing the effectiveness of interventions by:
- Tailoring interventions to address individual risk factors.
- Assessing their effectiveness.
- Modifying interventions as appropriate.
Image: Photograph shows medical provider with patient.
Slide 16: Sustainment
“Holding the gains and evolving as required, definitely not going back to the old way.”
Source: Maher L, 2013; Maher L, 2012.
Image: Photograph of a tree.
Slide 17: When Should We Worry About Sustaining the Gains?
- Actions to ensure sustainability must start at the beginning of a project.
- If you leave it to the end, it will be too late to make any changes that are needed to maximize the potential of sustainability.
- It is very important to ensure that you have things in place from the beginning to achieve and sustain the best improvement outcome you can.
Slide 18: Steps to Sustainability
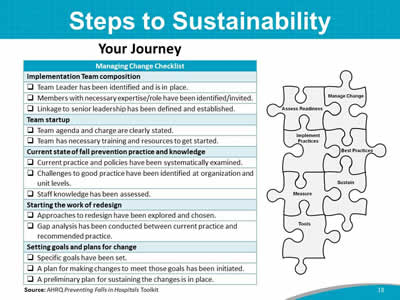
Your Journey
Managing Change Checklist
Implementation Team composition:
- ___ Team Leader has been identified and is in place.
- ___ Sustain: Changes need to become so integrated into existing organizational structures and routines that they are no longer noticed as separate from business as usual.Members with necessary expertise/role have been identified/invited.
- ___ Linkage to senior leadership has been defined and established.
Team startup:
- ___ Team agenda and charge are clearly stated.
- ___ Team has necessary training and resources to get started.
Current state of fall prevention practice and knowledge:
- ___ Current practice and policies have been systematically examined.
- ___ Challenges to good practice have been identified at organization and unit levels.
- ___ Staff knowledge has been assessed.
Starting the work of redesign:
- ___ Approaches to redesign have been explored and chosen.
- ___ Gap analysis has been conducted between current practice and recommended practice.
Setting goals and plans for change:
- ___ Specific goals have been set.
- ___ A plan for making changes to meet those goals has been initiated.
- ___ A preliminary plan for sustaining the changes is in place.
Source: AHRQ Preventing Falls in Hospitals Toolkit.
Image: Puzzle pieces are labeled “assess readiness,” “manage change,” “implement practices,” “best practices,” “measure,” “sustain,” and “tools.”
Slide 19: Sustaining Change
Sustain: Changes need to become so integrated into existing organizational structures and routines that they are no longer noticed as separate from business as usual.
Image: Puzzle pieces are labeled “assess readiness,” “manage change,” “implement practices,” “best practices,” “measure,” “sustain,” and “tools.” The piece labeled "sustain" is highlighted in blue.
Slide 20: High-Reliability Organizations
- High-reliability organizations:
- Provide consistent performance at high levels of safety over long periods of time.
- Practice “collective mindfulness,” understanding that even small failures in safety protocols or processes can lead to catastrophic or adverse events if action is not taken to solve the problem.
- Eliminate deficiencies in safety processes through the use of powerful tools to improve their processes.
- Create an organizational culture that focuses on safety; they are constantly aware of the possibility of failure.
Source: Chassin MR, Loeb JM, 2013; Chassin MR, Loeb JM, 2011.
Slide 21: Components of Sustainability
Four key strategies:
- Engage Leadership.
- Measure Continuously/Evaluate for Change.
- Collaborate With All Disciplines.
- Hardwire Practices and Educate.
Slide 22: Leadership Engagement

- High-level senior leadership buy-in.
- Designated fall prevention Implementation Team Leader.
- Designated fall prevention Implementation Committee/ Interdisciplinary Team.
Image: Photograph shows leaders and medical providers seated at a table.
Slide 23: Engage Leaders
It is the right thing to do—patient stories, their stories.
- WIFM: What’s in it for me/them?
- Cost avoidance estimation.
- Patient throughput.
- Turnover reduction.
- Leaders: Alignment of improvement efforts and organizational priorities.
- Senior executives: Rounding on units.
Source: Duval-Arnould J, Mathews SC, Weeks K, et al., 2012; Waters HR, Korn R Jr, Colantuoni E, et al., 2011
Slide 24: Engage Leaders
- Leadership support:
- Seek vice president or higher.
- Engage support for Team’s work.
- Rounding on unit—be purposeful.
- Script the rounds.
- How will the next patient in this unit be harmed?
- How can I help to remove barriers so that the safety defects we are most concerned about can be better addressed?
- How well does teamwork occur on this unit?
- What doesn’t work well?
- Use learning board as unit’s meeting point.
- Script the rounds.
Source: Sexton JB, 2010
Slide 25: Practice Insight
Increase Leadership Buy-in
Image: Icon of binoculars.
Slide 26: Components of Sustainability
Four key strategies:
- Engage Leadership.
- Measure Continuously/Evaluate for Change:
- Harness the power of local data to drive improvement efforts.
- Track prevention practices.
- Learn from defects.
- Collaborate With All Disciplines.
- Hardwire Practices and Educate.
Slide 27: Using Data for Continued Improvement
- Continue to collect process and outcome data.
- Set targets for process and outcome data.
- Gather information from defects.
- Use the data to identify opportunities and hardwire practices.
- Share data with:
- Improvement Team.
- Frontline staff.
- Leadership.
Slide 28: Annotated Run Chart
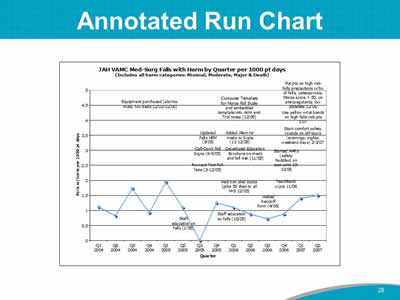
Image: Line graph shows JAH VAMC Med-Surg falls with harm by quarter per 1,000 patient days.
Slide 29: Components of Sustainability
Four key strategies:
- Engage Leadership.
- Measure Continuously/Evaluate for Change.
- Collaborate With All Disciplines:
- Collaborate with multiple disciplines.
- Identify physician and nurse champions.
- Tap into the wisdom of the frontline staff.
- Hardwire Practices and Educate.
Slide 30: Sustainable Collaboration
- Senior leadership support is important, but change comes most effectively from frontline staff. Tap into their wisdom.
- Multidisciplinary collaboration is essential to carrying out fall prevention.
- Gaining buy-in from all involved results in shared ownership of positive prevention results.
Image: Photograph shows leaders and medical providers seated at a table.
Slide 31: Sustainable Collaboration
- The fall prevention group should:
- Continue to meet (or merge with an existing group).
- Report up through a quality structure.
- Have a vision with clearly defined goals and an associated Action Plan. (Update every 6-12 months.)
- The Team and its goals should be:
- Aligned with its organization’s goals of preventing harm.
- Part of the dashboard.
Slide 32: Components of Sustainability
Four key strategies:
- Engage Leadership.
- Measure Continuously.
- Collaborate With All Disciplines.
- Hardwire Practices and Educate:
- Standardize care: prevention practices.
- Include practices in patients’ daily goals.
- Train new staff in evidence-based prevention practices.
Slide 33: Resource Needs Assessment
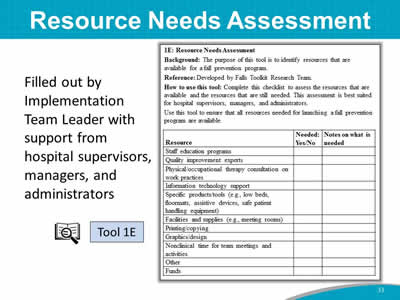
Filled out by Implementation Team Leader with support from hospital supervisors, managers, and administrators.
Images: Icon of a magnifying glass in front of an open book; checklist from Tool 1E: Resource Needs Assessment.
Slide 34: Resource Needs Assessment Results
Team Leaders: Let’s share results of this assessment for your organization.
Slide 35: Team Charge
Implement a Fall Prevention Program within 8-10 months.
Image: Photograph shows a medical provider holding the arm of a patient using a mobility device.
Slide 36: References
- Chassin MR, Loeb JM. High-reliability health care: getting there from here. Milbank Q 2013 Sep;91(3):459-90. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3790522/. Accessed June 16, 2017.
- Chassin MR, Loeb JM. The ongoing quality improvement journey: next stop, high reliability. Health Aff (Millwood) 2011 Apr;30(4):559-68. http://content.healthaffairs.org/content/30/4/559.long. Accessed June 16, 2017.
- Duval-Arnould J, Mathews SC, Weeks K, et al. Using the Opportunity Estimator tool to improve engagement in a quality and safety intervention. Jt Comm J Qual Patient Saf 2012 Jan;38(1):41-7,1.
- Maher L. Starting for Success. Partners In Care Programme: Webcall One. Health Quality & Safety Commission New Zealand. Counties Manukau Health. 2013. https://www.hqsc.govt.nz/assets/Consumer-Engagement/Partners-in-Care-Resource-page/Webex-1-starting-for-success-Oct-2013.ppt. Accessed June 16, 2017.
- Maher L. Welcome to the Partners In Care Webex 6 – 3 October 2012. Health Quality & Safety Commission New Zealand. NHS. https://www.hqsc.govt.nz/assets/Consumer-Engagement/Partners-in-Care-Resource-page/Sharing-Partner-in-Care-Webex-6-Oct-2012.ppt. Accessed June 16, 2017.
- Miake-Lye IM, Hempel S, Ganz D, et al. Chapter 19. Preventing in-facility falls. In: Making Health Care Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices. Rockville, MD: Agency for Healthcare Research and Quality; March 2013. https://www.ncbi.nlm.nih.gov/books/NBK133389/. Accessed June 15, 2017.
- Sexton JB. Engaging Leaders Webinar. 2010.
- Waters HR, Korn R Jr, Colantuoni E, et al. The business case for quality: economic analysis of the Michigan Keystone Patient Safety Program in ICUs. Am J Med Qual 2011 Sep-Oct;26(5):333-9.



