Module 2: How To Manage Change—Slide Presentation
Slide 1: How to Manage Change
ADD Hospital Name Here
Module 2
Slide 2: QI Change Process
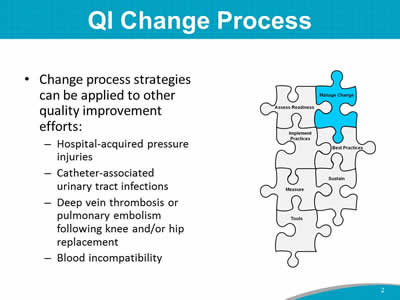
- Change process strategies can be applied to other quality improvement efforts:
- Hospital-acquired pressure injuries.
- Catheter-associated urinary tract infections.
- Deep vein thrombosis or pulmonary embolism after knee or hip replacement.
- Blood incompatibility.
Image: Puzzle pieces are labeled “assess readiness,” “manage change,” “implement practices,” “best practices,” “measure,” “sustain,” and “tools.” The piece labeled “manage change” is highlighted in blue.
Slide 3: Module 2 Goals
- Identify actions needed to improve organizational readiness.
- Maximize the possibility of successful implementation of the Fall Prevention Program by addressing the following questions:
- How can you set up the Implementation Team for success?
- What needs to change, and how do you redesign practice?
- How should goals and plans for change be developed?
- How do you bring staff into the process?
Slide 4: Expected Outcomes of Module 2
- Finalize Implementation Team members and assign roles. (Tool 2A)
- Present the completed process analysis on one patient care unit. (Tool 2C)
- Present the assessment of current fall prevention policies and procedures. (Tool 2D)
- Team Leader or designee completes assessment, and folds recommendations into the Action Plan.
Slide 5: Expected Outcomes
Begin to write a draft fall prevention Action Plan, tailored to your hospital.
Image: Photograph shows medical providers seated at table.
Slide 6: Implementation Team Guidelines
- How often will you meet?
- What are the ground rules for managing meeting time and communication?
- How will you communicate with each other?
- How will you communicate successes?
- How will the Team do its work?
- Small group work.
- Working meetings.
Slide 7: Finalize Team Members

The first goal is to finalize the Implementation Team members and assign roles.
Image: Photograph shows medical providers standing behind seated patient.
Slide 8: Successful Implementation Team
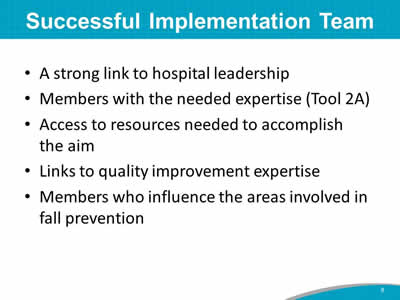
- A strong link to hospital leadership.
- Members with the needed expertise (Tool 2A).
- Access to resources needed to accomplish the aim.
- Links to quality improvement expertise.
- Members who influence the areas involved in fall prevention.
Slide 9: Interdisciplinary Team
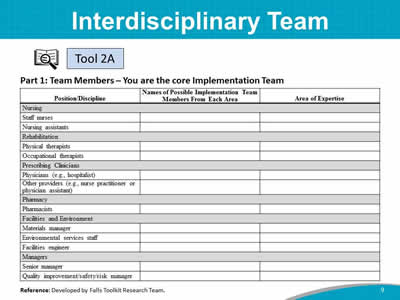
Images: A table captioned "Part 1: Team Members – You are the core Implementation Team" charts Position/Discipline, Names of Possible Implementation Team Members From Each Area, and Area of Expertise for the following potential team members:
- Nursing:
- Staff nurses.
- Nursing assistants.
- Rehabilitation:
- Physical therapists.
- Occupational therapists.
- Prescribing Clinicians:
- Physicians (e.g., hospitalist).
- Other providers (e.g., nurse practitioner or physician assistant).
- Pharmacy:
- Pharmacists.
- Facilities and Environment:
- Materials manager.
- Environmental services staff.
- Facilities engineer.
- Managers:
- Senior manager.
- Quality improvement/safety/risk manager.
An icon of a magnifying glass in front of open book refers to Tool 2A.
Reference: Developed by Falls Toolkit Research Team.
Slide 10: QI Process
- Link the Fall Prevention Program with quality improvement.
- This information helps you define resources your hospital has for quality improvement.
- Plan, Do, Study, Act (PDSA) is one systematic approach to analysis and implementation.
Images: Photograph shows medical providers looking at laptop together. An icon of a magnifying glass in front of open book refers to Tool 2B. An icon of a magnifying glass in front of open book refers to Page 21.
Slide 11: QI Process
- Your Implementation Team Leader has filled out many assessment forms already.
- We’ll be working to find solutions for positive change.
- Let’s hear from your Implementation Team Leader now about your hospital’s QI program and how to link with QI.
Image: Photograph shows a medical provider holding papers.
Slide 12:
- Use process mapping to examine key processes on selected units.
- Analyze the process maps.
- Do your processes incorporate best practices? (See Module 3.)
- Which practices need changing?
- How should processes be changed to build in the new practices?
Image: An icon of a magnifying glass in front of open book identifies process mapping as Tool 2C.
Slide 13: Process Map Example 1

Images: Icon of binoculars; process map of initial patient risk assessment using Morse Scale.
Slide 14: Process Map Example 2
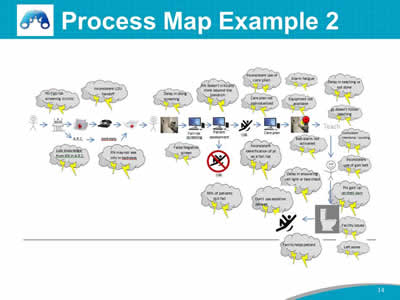
Images: Icon of binoculars; process map of fall prevention processes.
Slide 15: Current Process Analysis
Images: Screenshots show two sample pages of Current Process Analysis. An icon of a magnifying glass in front of open book identifies the text as Tool 2C.
Slide 16: Current Process Analysis
- Let’s hear from the Team members who completed the process analysis.
- Share process analysis from the unit.
- Point out key processes being used.
Image: Two photogaphs show a medical provider holding clipboard in front of laptop, and a medical provider holding clipboard and pen.
Slide 17: Fall Prevention Policies/Practices
Images: Screenshots show two pages of Fall Prevention Policies/Practices in table format. An icon of a magnifying glass in front of open book identifies the text as Tool 2D.
Slide 18: Assess Current Policies
- The Implementation Team Leader identified the policies in place and areas for improvement.
- You’ll want to address these areas in the Action Plan.
- Then, we will compare this assessment with best practices in Module 3.
- A group you designate may opt to do further fine tuning at a later time.
- Let’s look at the completed Tool 2D now.
Slide 19: Fall Knowledge Test
Images: Screenshots show three pages from the Fall Knowledge Test. An icon of a magnifying glass in front of open book identifies the text as Tool 2E.
Slide 20: Staff Knowledge Assessment
- Who will administer Tool 2E?
- How will it be administered?
- Who will be in charge of assessing the results?
Image: Photograph shows people using laptops and writing.
Slide 21: Implementation Action Plan
- The implementation Action Plan for change should address the following:
- Membership and operation of the Implementation Team.
- Standards of care and practices to be met.
- How gaps in staff education and competency will be addressed.
Slide 22: Implementation Action Plan
- The Action Plan also addresses:
- Plans for rolling out new standards and practices, where needed.
- Staff accountable for monitoring the implementation.
- How changes in performance will be assessed.
- How this effort will be sustained.
Slide 23: Action Plan
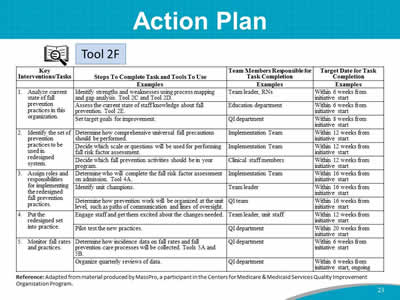
Images: A table charts Key Tasks, Steps To Complete Task and Tools To Use, Team Members Responsible for Task Completion, Target Date for Task Completion. Examples are provided for each task. An icon of a magnifying glass in front of open book identifies the text as Tool 2F.
Slide 24: Action Plan Example – Key Intervention 1
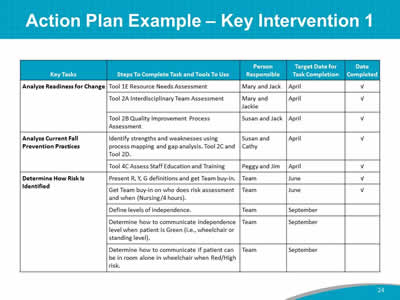
Image: A sample table charts the Key Tasks, Steps To Complete Task and Tools To Use, Person Responsible, Target Date for Task Completion, and Date Completed for each task.
Slide 25: Action Plan
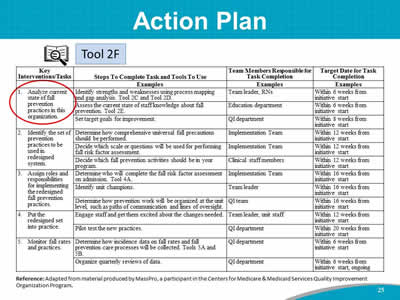
Image: A table shows a sample Action Plan. The first item under Key Interventions/Tasks, "1. Analyze current state of fall prevention practices in this organization," is circled in red. An icon of a magnifying glass in front of open book identifies the text as Tool 2F.
Slide 26: Managing Change Checklist
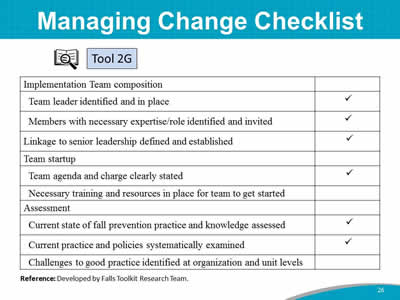
Images: The checklist is shown in table form. The checklist items are:
- Implementation Team composition:
- Team leader identified and in place.
- Members with necessary expertise/role identified and invited.
- Linkage to senior leadership defined and established.
- Team startup:
- Team agenda and charge clearly stated.
- Necessary training and resources in place for team to get started.
- Assessment:
- Current state of fall prevention practice and knowledge assessed.
- Current practice and policies systematically examined.
- Challenges to good practice identified at organization and unit levels.
An icon of a magnifying glass in front of open book identifies the checklist as Tool 2G.
Reference: Developed by Falls Toolkit Research Team.



