Module 5: How To Measure Fall Rates and Fall Prevention Practices—Slide Presentation
Slide 1: How To Measure Fall Rates and Fall Prevention Practices
ADD Hospital Name Here
Module 5
Slide 2: Basic Quality Improvement Principle
If you can’t measure it, you can’t improve it.
Image: Puzzle pieces are labeled “assess readiness,” “manage change,” “implement practices,” “best practices,” “measure,” “sustain,” and “tools.” The piece labeled “measure” is highlighted in blue.
Slide 3: Basic Quality Improvement Principles
- Fall rates and fall prevention practices must be tracked.
- By tracking performance, you will know whether care is improving, staying the same, or getting worse in response to efforts to change practice.
- Continued monitoring will help you see if your improvement gains are being sustained.
Image: Photograph shows a medical provider writing and using laptop.
Slide 4: Module 5 Goals
- The Implementation Team will agree on and develop a plan for:
- Measuring falls and fall-related injury rates.
- Measuring fall prevention practices.
- Communicating trends in fall and fall-related injury rates to key stakeholders.
Slide 5: 2012 NDNQI Definition of a Fall
A patient fall is an unplanned descent to the floor with or without injury to the patient. Include falls that result when a patient lands on a surface where you wouldn’t expect to find a patient.
NDNQI–National Database of Nursing Quality Indicators
Slide 6: NDNQI Definition
- All unassisted and assisted falls are to be included whether they result from physiological reasons (fainting) or environmental reasons (slippery floor).
Images: Photograph shows a staff member using mop and bucket. An icon of a magnifying glass in front of open book refers to Page 70.
Slide 7: Practice Insight
Assisted Falls
Image: Icon of binoculars.
Slide 8: How Will This Hospital Define a Fall?
- Develop a uniform definition and share it throughout the hospital.
- Make sure it is coupled with a culture of trust to encourage reporting fall incidents.
- Will you use NDNQI’s definition to measure and monitor falls?
Slide 9: NDNQI Repeat Fall Definition
- A repeat fall is more than one fall in a given month by the same patient after admission to the unit.
- Do you agree to use this definition?
Image: Photograph shows a person writing on a flip chart,
Slide 10: NDNQI Definitions of Fall Injury

- None or no injury: The patient is free of injuries (no signs or symptoms) resulting from a fall.
- Minor: Bruise, abrasion; needs dressing, ice, limb elevation, topical medications, etc.
Images: Three photographs show medical providers treating an injured knee, examining a patient’s wrist, and treating an injured arm.
Slide 11: NDNQI Definitions of Fall Injury

- Moderate: Needs sutures, Steri-Strips™/skin glue, splint; or resulted in muscle/joint strain.
Images: Two photographs show skin with stitches and a medical provider putting a splint on a patient’s leg.
Slide 12: NDNQI Definitions of Fall Injury

- Major: Needs surgery, cast, traction; and/or results in neurological or internal injury.
- Death: The patient died as a result of injuries sustained from the fall (not from physiologic events causing the fall).
Images: Three photographs show medical providers operating on a patient, a leg in a cast, and an empty hospital bed.
Slide 13: NDNQI Definitions of Fall Injury
- None: No injury
- Minor: Resulted in bruise, abrasion; needs dressing, ice, limb elevation, topical medications, etc.
- Moderate: Needs suturing, splinting; or caused muscle/joint strain
- Major: Needs surgery, cast, traction; results in neurological or internal injury
- Death.
Do you agree to use these definitions? What other definitions of fall injury would be appropriate for this hospital?
Slide 14: Agreed-Upon Definitions

- Definitions of a fall, repeat fall, and level of injury from a fall should be incorporated into:
- Policies and procedures.
- Incident reports.
- Root cause analyses/huddles.
- Staff education.
Image: Photograph shows medical providers using computers.
Slide 15: Measuring Fall Rates

Slide 16: Measurement Recommendations
- Measure falls over time within a unit to see if care is improving.
- Calculate falls as a rate (the rate of falls per 1,000 occupied bed days).
- This measure considers if the unit census is running high or low.
- Use this measurement approach consistently throughout the hospital.
Slide 17: Needed for Fall Rate Calculation
- Use incident reports to track data about the fall, date, patient, unit, location, circumstances, and level of injury.
- Some hospitals have electronic incident reporting systems, making it easier to count falls.
- What system do you use?
Images: Two photographs show a medical provider writing on a clipboard and medical providers looking at a laptop.
Slide 18: Incident Report Information
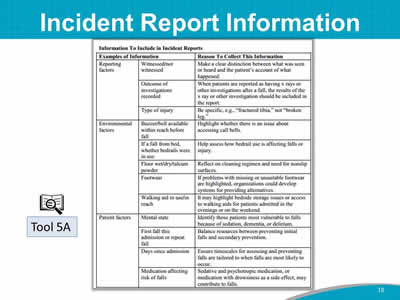
Images: A sample incident report is shown in table form. An icon of a magnifying glass in front of open book identifies this report form as Tool 5A.
Slide 19: Needed for Fall Rate Calculation
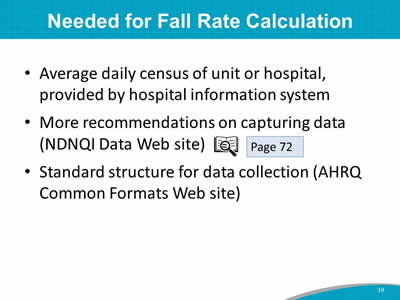
- Average daily census of unit or hospital, provided by hospital information system.
- More recommendations on capturing data (NDNQI Data Web site).
- Standard structure for data collection (AHRQ Common Formats Web site).
Image: An icon of a magnifying glass in front of open book refers to Page 72.
Slide 20: How To Calculate Fall Rate
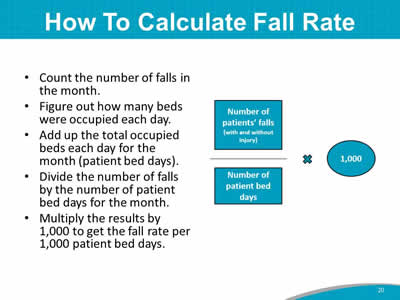
- Count the number of falls in the month.
- Figure out how many beds were occupied each day.
- Add up the total occupied beds each day for the month (patient bed days).
- Divide the number of falls by the number of patient bed days for the month.
- Multiply the results by 1,000 to get the fall rate per 1,000 patient bed days.
Image: A diagram depicts the calculation: Number of patients’ falls (with and without injury) divided by number of patient bed days times 1,000.
Slide 21: Fall Rate Calculation Example
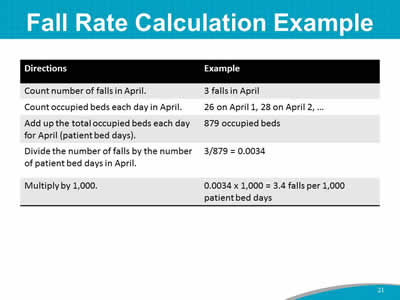
| Directions | Example |
|---|---|
| Count number of falls in April. | 3 falls in April |
| Count occupied beds each day in April. | 26 on April 1, 28 on April 2, ... |
| Add up the total occupied beds each day for April (patient bed days). | 879 occupied beds |
| Divide the number of falls by the number of patient bed days in April. | 3/879 = 0.0034 |
| Multiply by 1,000. | 0.0034 x 1,000 = 3.4 falls per 1,000 patient bed days |
Slide 22: Calculate Fall Rate
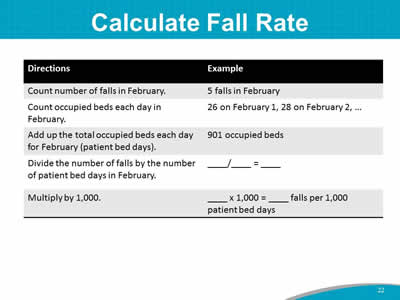
| Directions | Example |
|---|---|
| Count number of falls in February. | 5 falls in April |
| Count occupied beds each day in February. | 26 on February 1, 28 on February 2, ... |
| Add up the total occupied beds each day for February (patient bed days). | 901 occupied beds |
| Divide the number of falls by the number of patient bed days in February. | ___/___ = ___ |
| Multiply by 1,000. | ___ x 1,000 = ___ falls per 1,000 patient bed days |
Slide 23: Calculation of Fall Rates
When you complete your Action Plan, you will:
- Identify sources of data to collect.
- Select a person or team responsible for doing the calculations and tracking. Count the number and level of injury of falls in a month.
Images: Two photographs show medical providers looking at a computer screen and a medical provider using a tablet.
Slide 24: Use of Data
- Examine the rates for trends over time.
- Graph data in a run chart to visually examine.
- Are rates getting better or worse?
- Can you relate changes in rates to changes in practice?
- Rates are probably quite different by patient unit.
- Focus on trends over time. There will be fluctuations. Don’t overreact.
Slide 25: Fall Rate Data

When you first start tracking, you may notice increased fall rates. This is not necessarily due to worse care. Instead, unit staff members are becoming better at reporting falls that were missed in the past.
Images: Two photographs show medical providers looking at papers and at a computer screen.
Slide 26: Use of Data
- Find ways to disseminate the information to key stakeholders and unit staff.
- Post monthly rates where all staff can see how the unit is doing.
- Send reports to leadership.
Image: Photograph shows administrators holding a meeting.
Slide 27: Examining Data
- Study your post-fall huddle data in detail to understand what leads to each fall.
- Determine whether falls are irregular events, or whether there is a pattern in the types of falls (e.g., related to toileting).
Image: An icon of a magnifying glass in front of open book refers to Page 76.
Slide 28: Benchmarks for Comparison?
- Currently, no national benchmarks exist for comparing fall rates.
- It’s difficult to compare patients across hospitals because some patients are more likely to fall.
- Focus on improvement over time in your hospital.
- There are a number of ongoing initiatives to determine fall rates using a standardized method.
- Monitor current literature on fall rates for benchmarking.
Image: An icon of a magnifying glass in front of open book refers to Page 77.
Slide 29: Practice Insight
Benchmarking
Image: Icon of binoculars.
Slide 30: Displaying Data/Storytelling
- Run charts.
- Control charts.
- Annotation (show your interventions).
Slide 31: Run Charts
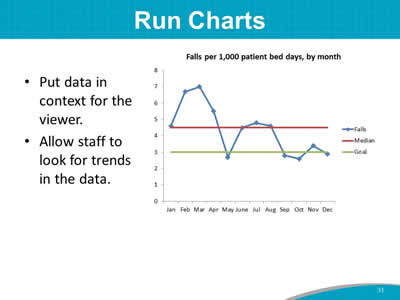
- Put data in context for the viewer.
- Allow staff to look for trends in the data.
Image: Example of run chart: falls per 1,000 patient bed days, by month
Slide 32: Control Charts
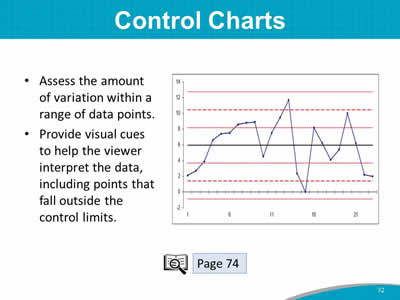
- Assess the amount of variation within a range of data points.
- Provide visual cues to help the viewer interpret the data, including points that fall outside the control limits.
Images: Example control chart. An icon of a magnifying glass in front of open book refers to Page 74.
Slide 33: Falls per 1,000 Patient Days
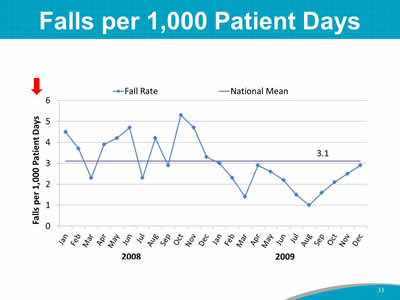
Image: Run chart: falls per 1,000 patient days.
Slide 34: Calculate Fall Rate by Type of Fall
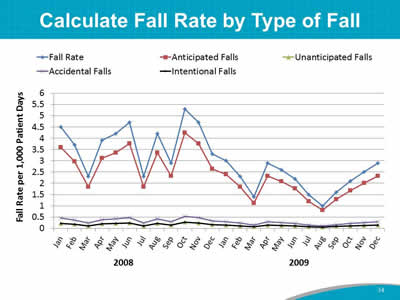
Image: Run chart: fall rate by type of falls.
Slide 35: Annotated Run Chart
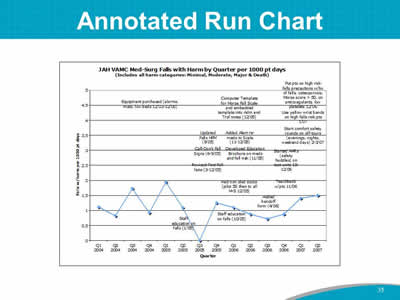
Image: Annotated run chart: med-surg falls with harm by quarter per 1,000 patient days.
Slide 36: Painting the Picture With Data
- Is your program improving?
- Are your patients safer?
Slide 37: Measuring Fall Prevention Practices
Slide 38: Measuring Fall Prevention Practices
- Measuring fall rates tells you how your facility is performing.
- Measuring fall prevention practices may tell you how to improve care.
- If the fall rate is high, what specific areas should you focus on?
- Are key practices to reduce falls being done consistently?
Slide 39: What Practices Should Be Measured?
Initially, look at two practices:
- Performance of fall risk factor assessment within 24 hours of admission.
- Performance of care planning that addresses each risk factor identified during fall risk factor assessment.
Images: Three photographs show medical providers at a patient’s bedside, a medical provider and a patient with a mobility device, and a medical provider at a patient’s bedside.
Slide 40: Performance Review of Fall Risk Factor Assessment Within 24 Hours
- Use the Morse Fall Scale (or the one your hospital agreed on).
- Ensure that known risk factors for falls are assessed.
- See the sample protocol for assessing performance.
Images: Photograph shows a pharmacist checking prescriptions. An icon of a magnifying glass in front of open book refers to Page 78.
Slide 41: Care Planning Assessment
- All risk factors identified on the fall risk factor assessment need to be addressed in the care plans.
- Next, act on the care plans.
- Critical thinking by staff.
- Tailored approach to each patient, based on the patient’s risk factors.
- Ensure that care plans address all areas of risk.
Slide 42: Assessment of Care Plan Performance
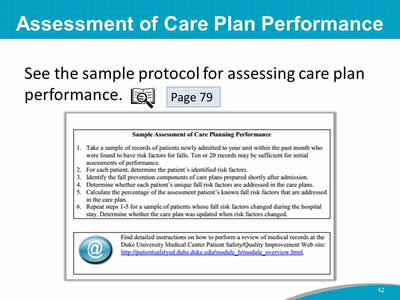
See the sample protocol for assessing care plan performance.
Images: A screenshot shows a sample protocol. An icon of a magnifying glass in front of open book refers to Page 79.
Slide 43: Care Process Assessment
Tool 5B combines medical record review with direct observation.
Image: Photograph shows a medical provider standing at a patient’s bedside.
Slide 44: Assessing Fall Prevention Care Processes
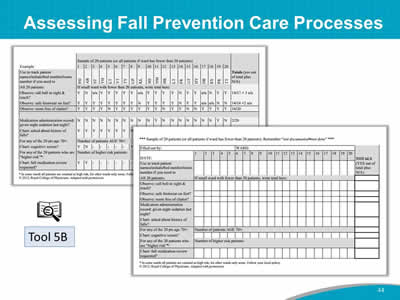
Images: Two screenshots show a sample fall prevention assessment in table form. An icon of a magnifying glass in front of open book identifies this as Tool 5B.
Slide 45: Measurement Action Plan
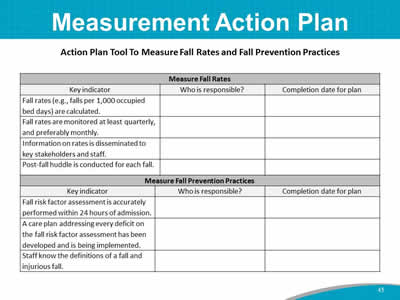
Action Plan Tool To Measure Fall Rates and Fall Prevention Practices
| Measure Fall Rates | ||
|---|---|---|
| Key indicator | Who is responsible? | Completion date for plan |
| Fall rates (e.g., falls per 1,000 occupied bed days) are calculated. | ||
| Fall rates are monitored at least quarterly, and preferably monthly. | ||
| Information on rates is disseminated to key stakeholders and staff. | ||
| Post-fall huddle is conducted for each fall. | ||
| Measure Fall Prevention Practices | ||
|---|---|---|
| Key indicator | Who is responsible? | Completion date for plan |
| Fall risk factor assessment is accurately performed within 24 hours of admission. | ||
| A care plan addressing every deficit on the fall risk factor assessment has been developed and is being implemented. | ||
| Staff know the definitions of a fall and injurious fall. | ||
Slide 46: Action Plan
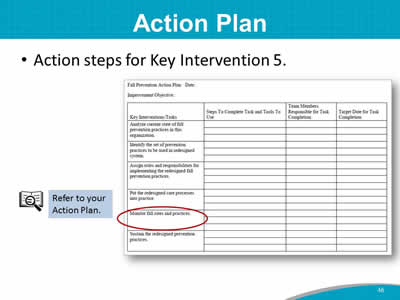
- Action steps for Key Intervention 5.
Images: A sample Action Plan is shown with Key Intervention 5 circled in red. An icon of a magnifying glass in front of open book sits next to the text "Refer to your Action Plan."
Slide 47: Summary
- In this module, we discussed the following:
- This hospital’s definition of a fall.
- How to measure fall and fall-related injury rates.
- How to measure fall prevention practices.
- How to communicate the trends in fall and fall-related injury rates to key stakeholders.
Slide 48: Next Steps

- Over the next several weeks, we will meet weekly to refine your Action Plan for the Fall Prevention Program.
- Thank you for being a part of this Team to make this hospital safer for patients.



