
Now you are ready to begin implementing the bundle of pressure ulcer prevention best practices you have identified. No matter how good the bundle that you develop is, if it is not used by the staff it will not be successful. To this point, you have looked at your organization's readiness to improve pressure ulcer prevention (section 1); assessed needs, set goals, and begun preparing for change (section 2); and examined best practices (section 3). In this section, the Implementation Team will work with the Unit-Based Teams and Wound Care Team to bring this earlier work to bear on actually implementing the new prevention practices at the frontline care level.
Your organization may already be using some of the best practices you identified in your bundle, but other practices will involve changes in the way you complete tasks. You will need to be flexible and may need to modify your plan to fit the needs of your organization. For the new practice bundle to be fully implemented and sustained, it will need to be customized to your organization and integrated into ongoing work processes rather than simply layered on top as a special project. As you progress, your improvement efforts may still have interim steps or midcourse corrections along the way and you will recognize that quality improvement is an ongoing process.
The questions in this section are intended to guide you in multiple aspects of implementation, from determining the specific roles that different clinical and support staff will play to putting the practices into operation first on a pilot basis and then across the organization. To successfully implement your change program, you should answer three sets of questions:
- What roles and responsibilities will staff have in preventing pressure ulcers?
- How do we assign roles and responsibilities?
- What role will the Wound Care Team play?
- What if our hospital has no formal Wound Care Team?
- What role will the Unit-Based Team play?
- What role will the Unit Champions play?
- How should the prevention work be organized at the unit level?
- What pressure ulcer prevention practices go beyond the unit?
- How do we put the new practices into operation?
4.1 What roles and responsibilities will staff have in preventing pressure ulcers?
In section 2 you examined current practices and identified aspects needing improvement and in section 3 reviewed the bundle of best practices. Now you need to define specifically what needs to change to put your selected bundle into practice and to decide who is going to do what in each aspect of the bundle. Specific areas of responsibility and paths of communication and accountability will be needed.
Hospitals and units within them vary in their staffing patterns and usual ways of doing business. You will need to consider staff roles based on the features of your organization overall and the individual units involved in pressure ulcer prevention. The Implementation Team will want to involve members of the Unit-Based Team and Wound Care Team in these decisions. That way, the implementation of the new practices will be tailored to each unit's staffing and operating practices and staff will be engaged in the change process, which will increase the likelihood of success.
Staff roles should be clearly defined so that everyone will understand if and how their roles will change. If you will implement the prevention bundle with current staff, you will want to take their skills and strengths into account in allocating responsibilities. You will need to consider not only what individual responsibilities are but also how the roles interact and what ongoing communication and reporting are needed. As highlighted earlier, successful pressure ulcer prevention will require teamwork. Teams at all levels must work together in an interdisciplinary manner.
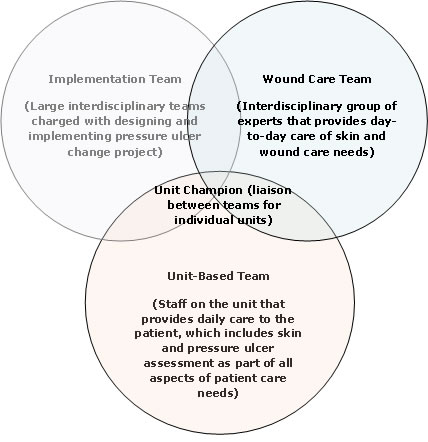
The figure below illustrates the overlapping responsibilities of different staff involved in pressure ulcer prevention. We introduced this figure in section 2.1.3 to highlight the multiple teams involved in the effort to improve pressure ulcer prevention. The original picture was intended to illustrate with overlapping circles the distinct but intersecting roles of the Implementation Team, Wound Care Team, and Unit-Based Team in the improvement process.
In this section, the focus shifts to how the new bundle of practices will work in daily operations and to defining what the ongoing responsibilities of the Wound Care Team and the Unit-Based Team will be in that new bundle. In this context, the figure highlights their different but intersecting ongoing roles. Consistent with that shift in focus, a new role of Unit Champion is added to the illustration and the Implementation Team begins to move to the background.
Figure 2. Team responsibilities
The questions below will guide you through the process of considering and specifying the roles and responsibilities of the Wound Care Team, unit staff, and Unit Champion. The questions also will guide you in deciding how best to organize the prevention work at the unit level and how to customize the bundle for specific work units in your organization.
4.1.1 How do we assign roles and responsibilities?
It is important to determine who will perform each specific task identified in the bundle of best practices you have identified. In some cases, a group will perform a task based on their specific role or title, such as Certified Nursing Assistants (CNAs). Other tasks may be assigned to a specific individual. In that case, always make sure you have a backup; it is important that everyone knows who the backup is when the assigned individual is unavailable.
As you work through this section, you should consider taking each task from your bundle and entering it into the summary page of the worksheet provided as Tool 4A in Tools and Resources. Then assign specific individuals or groups to each task. Sections 4.1.2 through 4.1.5 include examples of responsibilities different staff might take on; those examples are summarized in Tool 4B. In making these assignments, make sure you work with the unit manager or Unit Champions from the units in which you are implementing change.

Tools
In Tools and Resources, you can find a worksheet to use in deciding how responsibilities will be assigned in your organization (Tool 4A, Assigning Responsibilities for Using Best Practice Bundle) together with a summary page illustrating how responsibilities might be organized (Tool 4B, Staff Roles).
4.1.2 What role will the Wound Care Team play?
Most hospitals have a Wound Care Team that directs wound care and assists in preventive practices. The Wound Care Team is your hospital's content expert on pressure ulcer prevention. The Wound Care Team may be a formal or informal department, or it may be an individual clinician. The team may consist of nurses (RN, LPN), physical therapists, dietitians, or nurse aides, as well as health care providers (physicians, physician assistants, and nurse practitioners).
Team members may or may not be certified in wound care and may be led by a physician, nurse, or physical therapist. The team may provide day-to-day care for wounds in both inpatient and outpatient settings. Regardless of the team's size or composition, the team members are the hospital experts and resources in current wound care practice and evidence. When people have questions, this is where they go for answers.

Practice Insights
Beyond serving as content experts, the Wound Care Team may engage in a variety of different activities, such as:
- Providing formal educational activities for clinicians, including lectures and inservice sessions.
- Providing education to patients and families.
- Developing hospitalwide policies and procedures related to pressure ulcer prevention and treatment.
- Rounding on pressure ulcer patients.
- Rounding on high-risk patients.
- Rounding periodically with unit staff to ensure that prevention practices are being carried out and any identified pressure ulcers are being appropriately staged and treated.
- Organizing and participating in prevalence and incidence audits; examining clinical practice, care planning, and documentation by unit staff
What if your hospital has no formal Wound Care Team?
Not all hospitals have a formal Wound Care Team. Small hospitals may have one nurse or physical therapist who handles all wound care or may contract with an outside company to provide wound care when needed. The available wound care expertise, or lack thereof, must be carefully considered by the Implementation Team in planning the change project. The Implementation Team may have to advocate for the recruitment of additional expertise through hiring of new staff or outside contracts. Other options are providing advanced wound training by interested staff or using experts from nearby universities or your State Quality Improvement Organization (QIO).

Action Steps
- Determine what responsibilities the Wound Care Team will have in preventing pressure ulcers.
- Highlight which of these responsibilities will differ from the Wound Care Team's current role and therefore will require changes in practice. These will require special attention as you manage the implementation of the new bundle (section 4.2).
- If there is no formal Wound Care Team or designated wound care lead, determine how this role will be filled before going further.
- If there are other barriers to the Wound Care Team or designated wound care lead filling the defined roles, highlight them for use in planning your change strategies (discussed in section 4.2).
4.1.3 What role will the Unit-Based Team play?
The Unit-Based Team consists of staff members who provide daily direct patient care by conducting comprehensive skin and risk assessment, planning care for risk prevention, and ensuring that care is performed and documented. In other words, they are responsible for the performance of your bundle of best practices. In most cases, the Unit-Based Team will include everyone on the unit, such as RN, LPN, CNA, hospitalist, dietitian, and other staff assigned to a unit on a regular basis.
The types of staff working in your hospital may differ from these. You will need to assign roles appropriate to your staffing configuration. An example of the allocation of roles between nurses, aides, and other staff is shown below ("Practice Insights"). It is important to be clear on what roles have or have not changed and what is permitted in each State's practice acts.

Practice Insights
Nurse:
- Completes and documents skin and risk assessments.
- Monitors progress or changes in medical/skin condition.
- Documents care and prevention practices.
- Reports patient problems to health care provider.
- Obtains consults and medical orders as needed.
- Works with wound team to prevent or treat pressure ulcers.
- Educates patient and family as appropriate.
- Supervises aides.
- Knows how to obtain needed supplies if the wound nurse is not available.
Nurse aides:
- Examine skin during each position change or skin cleaning.
- Perform appropriate care plan tasks.
- Report task completion and skin issues to the nurse.
Hospitalist:
- Reviews need for specific types of rehabilitation therapy.
- Writes orders for specific interventions.
Dietitian:
- Assesses nutritional status of patient.
- Makes specific recommendations regarding diet, including supplements.
The Unit-Based Team will work collaboratively with the Wound Care Team. Members may notify the Wound Care Team if skin problems arise or if high-risk patients are identified. They also will work collaboratively with the Wound Care Team to design education and care plans for patients and their families. Most important, they must be empowered to ask questions of the Wound Care Team. They should all feel able to contact the experts if they are unsure what care they should be providing.
Special attention is required when temporary staff rotate onto the unit. They will not be aware of how care is organized on the unit and what their critical role is in pressure ulcer prevention. Given how frequently this occurs on most hospital units, unit managers should develop plans in advance so that temporary staff can be rapidly oriented to their exact roles on the team. Make sure you have a plan in place for temporary staff and can provide appropriate monitoring and assistance.

Action Steps
- Define the roles for all members of the Unit-Based Team. Worksheet 4A in Tools and Resources may help in this process. You may need to tailor roles to accommodate differences in staffing and practices in different units.
- Develop a plan for orienting and monitoring temporary staff.
- Be sure staff roles you have developed are in compliance with your State practice acts.
- Highlight which of these responsibilities will differ from the Unit-Based Team members' current roles and therefore will require changes in practice. These will require special attention as you manage the implementation of the new bundle (described in section 4.2).
- If you anticipate barriers to unit staff filling the defined roles, highlight them for use in planning your change strategies (described in section 4.2).

Tools
The summary sheet presented as Tool 4B, Staff Roles, can help you think through these issues, and Tool 4A, Assigning Responsibilities for Using Best Practice Bundle, can help you record your decisions.
4.1.4 What role will the Unit Champions play?
Many successful improvement efforts have relied on Unit Champions as critical members of the Unit-Based Team, especially during the implementation process. A Unit Champion is a staff member who serves as the liaison between the Implementation Team, the Wound Care Team, and the unit staff. The Unit Champion is someone who is familiar with the program goals, bundles of care, and outcome data that will be used. He or she is often the initial "go to" person when staff have questions. The Unit Champion posts results and reports on program progress and provides updates in staff meetings. He or she helps conduct outcome audits. Most important, the Unit Champion is often the "cheerleader" who encourages staff during the difficult implementation process. A Unit Champion may be anyone who works on the unit, including nurses (RN, LPN) and nurse aides.
A promising approach would be to have two champions per shift. This approach ensures that a champion is always available and assists with succession planning if one person leaves. However, some hospitals might not have enough staff to have this many champions. For example, in smaller hospitals, two champions for days and one for nights could be enough for the entire hospital. The number of champions should be customized to fit the needs of your hospital.
The role of the Unit Champion can be temporary and only needed for getting the program started. Once practices are routinized, the champion may not be needed. However, maintaining a "go to" person may help with program sustainability and ease introduction of additional changes or modifications.
Another approach that has been used successfully is to have several staff on the unit serve as pressure ulcer resources without the formal title of Unit Champion. This has occurred when frontline staff have become engaged in and excited about pressure ulcer prevention, usually as a result of their early involvement in improvement efforts. While this approach may not have the public visibility of a Unit Champion, it brings the benefits of engaging more staff and embedding knowledge of good prevention practices more deeply in each unit. The characteristics of these individuals and their roles would be similar to the Unit Champions during the improvement process, and they would remain in place after pressure ulcer prevention has become routine.
You should consider which approach will be most successful in your organization.

Action Steps
Look for these characteristics in your Unit Champions and resource staff:
- Satisfactory level of performance.
- Excellent communication skills.
- Effective linkage to other staff members.
- A demonstrated positive image of their unit and with nursing personnel.
- The ability to identify and help solve typical nursing issues.
- Knowledge of the benefits and process of pressure ulcer prevention.
- Ability to collaborate with all key stakeholders in the improvement process.

Tools
Tool 4B, Staff Roles, and Tool 4A, Assigning Responsibilities for Using Best Practice Bundle, in Tools and Resources may help you define the role of Unit Champions and resource staff.
4.1.5 How should the prevention work be organized at the unit level?
While the definition of team member roles is the first step in determining how the prevention work will be carried out, attention must also be paid to how the work is organized: What are the paths of ongoing communication and reporting, including the lines of oversight and accountability? What documentation is needed and to whom is it submitted? How will pressure ulcer prevention be integrated with ongoing work processes?
The mapping of current processes and analyses of gaps from best practices that you did earlier (described in section 2.2.2) will help address these questions. The earlier work will help you identify the key points of communication and accountability that need to be addressed and to highlight problem areas that require special attention and may need contingency plans.
What paths of ongoing communication and reporting will be used?
Communication must be between staff at all levels: within the unit (e.g., between nurses, nurses and aides, nurses and physician, nurses and other staff) and between unit staff and the Wound Care Team. Consider where your communication weaknesses or breakdowns are and how they can be addressed. What linkages, for example, can you build in for successful interdisciplinary collaboration within the unit and across departments?
Some organizations monitor pressure ulcers in multidisciplinary patient safety rounds. Others specify processes for exchanging information at each shift change and for nurses sharing information with aides at each shift change. The key aspects are that the communication processes occur regularly and thoroughly with the least amount of time and effort.
Nurse's aides may want to have a mechanism to convey skin issues to their nurse in a written format. Too often if the aide just gives skin information orally, it may be overlooked by the nurse because of time constraints or other urgent patient care needs. You may want to institute a formal method for aides to report skin issues to their supervising nurse. One example is a tablet with pull-off pages. The aide can write the patient name and room number, date/time, and information for the nurse and give it to him or her.
Also consider how you will communicate with patients and their families if the patient is at risk of a pressure ulcer or if the patient's skin deteriorates. Think about whether new processes are needed and, if so, what they will be. You may want to obtain or develop general informational materials for patients about the risks and potential consequences of pressure ulcers.
Practice Insights
Examples of communication and reporting:
- Risk and skin assessment information are included at all shift reports.
- Pressure ulcer risk or presence is documented on a unit flowsheet daily.
- Five-minute standup meetings are used to communicate important patient safety issues and changes in care plans.
- Interdisciplinary "Skin Rounds" are used to examine patients at risk for pressure ulcers.
- Nurse aides have guidelines and tools for reporting new skin or risk problems, such as a tablet with pull-off pages including patient name, room number, and date/time to be given to the designated nurse.
- Nurses have guidelines for treatment if Wound Care Team is not available.
- Patient and family are given pressure ulcer information on admission.
- Patient and family are notified if skin or risk changes.
- Staff have pocket cards to remind them of the practices they should be following.
What will the lines of oversight and accountability be?
Accountability of staff action is critical to successful improvement. Knowing something should be done does not ensure that it is. Skin and risk need to be assessed, care planning is needed to address that risk, and someone has to ensure that the plan is actually carried out. Possible mechanisms to address accountability are competency testing, inclusion of information on staff evaluations, and inclusion in policies, procedures, and care guidelines. Accountability should apply to both the unit and individual staff members.
Practice Insights
Examples of oversight and accountability:
- For unit accountability, Unit Champions post the latest pressure ulcer audit results and work with the Wound Care Team to educate their staff on areas still requiring improvement.
- For individual accountability, supervisory meetings between nurse managers and staff are routinely conducted to review pressure ulcer practices; competency testing is done annually.
How will pressure ulcer prevention be integrated into ongoing work processes?
Building new pressure ulcer prevention practices into ongoing work processes will be key to sustainability. If new practices are simply layered on top of current practices, they are likely to be dropped when the special project is over. Strategies for building into ongoing processes include:
- Making certain procedures universal so that staff do not have to decide which patients they apply to,
- Adding pressure ulcer communication to other established processes such as shift handoffs, and
- Creating visual cues or reminders in physical locations, such as turning clocks to remind staff when repositioning is due.
Practice Insights
Examples of incorporating change into routine:
- A newly admitted high-risk patient automatically triggers a wound care and dietary consult with consult information used by unit staff to individualize care planning to meet the patient's specific needs.
- Pressure-redistributing support surfaces are provided for all patients.
- Regular processes are instituted for ordering special surfaces and ensuring prompt delivery to the units. Correct-sized equipment is readily available.
- Processes are streamlined to order and obtain support surfaces quickly for patients identified as at risk.
- Nurses have access to dressings when wound staff are unavailable.
- Visual or auditory prompts (turning clocks, chimes, etc.) are used to prominently signal turning schedules to ensure that patients are turned at appropriate intervals.
- A "skin cart" incorporates all necessary supplies in one place.
Many hospitals are now using electronic medical records, which provide additional opportunities for integrating best practices into the daily routine. Work with your information technology (IT) department to explore how the electronic medical record may be used in the quality improvement effort. Questions to consider in this context include:
- What information about skin condition and risk is already part of the patient record?
- Are data already in the system that can be used as part of a new process to assess pressure ulcer risk?
- What is the most logical place in the record to collect/organize/assess information about patient skin condition and any necessary precautions?
Practice Insights
Building electronic documentation systems
Quality improvement teams at several sites collaborated with IT to build documentation of pressure ulcer risk and care planning into their computer charting systems. Features that were added to electronic documentation systems included:
- Automatic consults to wound care nurses, dietitians, or physical therapists if a pressure ulcer is recorded or risk assessment scores are below a certain threshold.
- Patient education booklet linked to the documentation system so that it is readily available if needed.
- Pressure ulcer prevention guidelines or quick reference text integrated into the computer charting system.

Action Steps
- Working from the process map for pressure ulcer prevention and gap analysis you developed for your organization in the redesign process (section 2.4), develop your individualized operating rules to specify:
- The paths of ongoing communication and reporting.
- The lines of oversight and accountability.
- Documentation that is needed and people to whom it is submitted.
- Strategies for integrating pressure ulcer prevention into ongoing work processes.
- These rules should include not only regular activities, but also contingencies, such as gaining access to the supply cabinet on weekends when the regular wound nurse is out.
- Consistent with those decisions, complete the worksheet provided as Tool 4A in Tools and Resources to assign specific individuals or groups to each task.
- Determine which changes in practice, if any, will require changes in formal hospital policies and procedures.
4.2 What pressure ulcer prevention practices go beyond the unit?
Our focus in the toolkit is primarily on preventing pressure ulcers at the unit level. However, as you organize the unit work, you should think beyond the unit in two ways. First, consider how information about pressure ulcer risks is conveyed in handing off patients to other units or when discharging patients. Handoffs are generally weak links in our systems. When patients are transferred from the ED or ICU, do you regularly get information on their skin condition? Is there information about how long they were lying in the ED or whether there were problems in transit that could compromise their skin integrity? On discharge, are patients and families given information about skin care and pressure ulcer prevention? Are there gaps in practice that you should address?
Second, consider how the interactions of other members of the hospital staff with patients could contribute to the observation and care of patients on the unit. For example, orderlies who transfer and transport patients on and off the unit can assist in care by ensuring that their transfer techniques are consist with standards of practice and by being alert to the dangers of lying too long on the gurney in one position. Dietary staff who distribute and collect trays can tell you how well the patients are eating and drinking. The environmental staff who are in and out of the rooms can tell you if the patient's pain is adequately controlled or if they are depressed. It can be surprising what patients and their families share with these people and keep from clinical staff.



