Safe Medication Administration: Slide Presentation
AHRQ Safety Program for Perinatal Care
Slide 1: AHRQ Safety Program for Perinatal Care
Safe Medication Administration
Slide 2: Learning Objectives
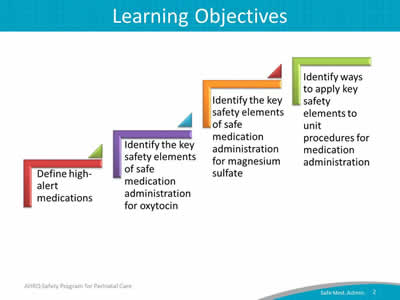
Image: Four ascending steps show the learning objectives:
- Define high-alert medications.
- Identify the key safety elements of safe medication administration for oxytocin.
- Identify the key safety elements of safe medication administration for magnesium sulfate.
- Identify ways to apply key safety elements to unit procedures for medication administration.
Slide 3: Safe Administration of Medications in L&D
- The safe administration of two commonly used high-alert medications in labor and delivery (L&D) units is the focus of one customizable bundle within the AHRQ Safety Program for Perinatal Care (SPPC):
- Oxytocin.
- Magnesium sulfate.
- The training materials and tools for this bundle offer key safety elements of safe medication administration for these medications.
- Key safety elements.
- Provide a comprehensive starting point for each unit to consider as it establishes its processes for ensuring safe medication administration of these drugs.
- Can also be adapted and applied to other high-alert medications used on L&D units.
Slide 4: High-Alert Medications1
- High-alert medications are "drugs that bear a heightened risk of causing significant patient harm when they are used in error."
- Although mistakes are not necessarily more common with these drugs, the consequences of errors are more serious for patients.
- These medications require special safeguards to reduce the risk of errors, such as the following:
- Improving access to information about these drugs.
- Limiting access.
- Using auxiliary labels and automated alerts.
- Standardizing the ordering, storage, preparation, and administration.
- Employing redundancies such as automated or independent double checks when necessary.
Slide 5: Safe Medication Administration Tools
- Purpose.
- Who should use.
- How to use.
- Key safety elements.
- Sample procedure.
Slide 6: SPPC Key Perinatal Safety Elements for Safe Medication Administration
- Standardize When Possible (CUSP Science of Safety).
- Create Independent Checks (CUSP Science of Safety).
- Simulation (SPPC Pillar).
- Learn From Defects (CUSP Module).
- Teamwork Training (TeamSTEPPS®).
- Patient and Family Engagement (CUSP Module).
Slide 7: Oxytocin
Oxytocin
Slide 8: Rationale for Safe Medication Administration Tool
- Oxytocin is a high-alert medication.
- Oxytocin is commonly used on L&D units, but administration procedures vary greatly due to lack of standardization, local culture, and individual provider training and preferences.
- Inappropriate use of oxytocin is one of the top areas of preventable perinatal harm.2,3
- Types of inappropriate use:
- Use of oxytocin when contraindicated (i.e., elective inductions prior to 39 completed weeks).
- Errors and slips in medication administration, fetal and maternal monitoring, and delays in responding to oxytocin-induced complications (e.g., uterine tachysystole).
- Types of inappropriate use:
Slide 9: Key Safety Elements: Standardize When Possible
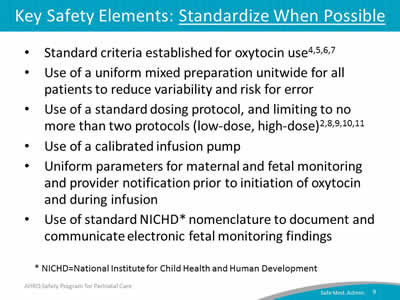
- Standard criteria established for oxytocin use.4,5,6,7
- Use of a uniform mixed preparation unitwide for all patients to reduce variability and risk for error.
- Use of a standard dosing protocol, and limiting to no more than two protocols (low-dose, high-dose).2,8,9,10,11
- Use of a calibrated infusion pump.
- Uniform parameters for maternal and fetal monitoring and provider notification prior to initiation of oxytocin and during infusion.
- Use of standard NICHD* nomenclature to document and communicate electronic fetal monitoring findings.
* NICHD=National Institute for Child Health and Human Development.
Slide 10: Key Safety Elements: Create Independent Checks
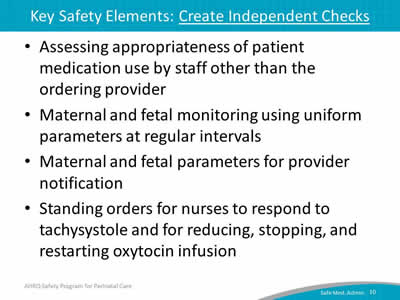
- Assessing appropriateness of patient medication use by staff other than the ordering provider.
- Maternal and fetal monitoring using uniform parameters at regular intervals.
- Maternal and fetal parameters for provider notification.
- Standing orders for nurses to respond to tachysystole and for reducing, stopping, and restarting oxytocin infusion.
Slide 11: Key Safety Elements: Learn From Defects

- Debrief and analyze near misses and adverse events related to oxytocin use.
- Have a process in place to review—
- Inductions outside of policy-defined indications.
- Severe maternal or neonatal morbidity and mortality events.
- Share outcomes or process improvements from informal and formal analysis with staff to achieve transparency and organizational learning.
Slide 12: Key Safety Elements: Simulation
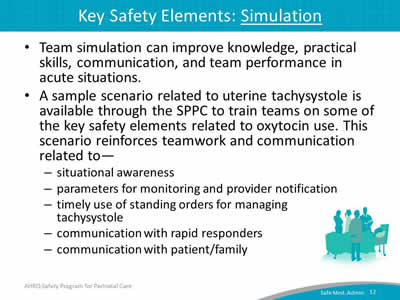
- Team simulation can improve knowledge, practical skills, communication, and team performance in acute situations.
- A sample scenario related to uterine tachysystole is available through the SPPC to train teams on some of the key safety elements related to oxytocin use. This scenario reinforces teamwork and communication related to—
- Situational awareness.
- Parameters for monitoring and provider notification.
- Timely use of standing orders for managing tachysystole.
- Communication with rapid responders.
- Communication with patient/family.
Slide 13: Key Safety Elements: Teamwork Training
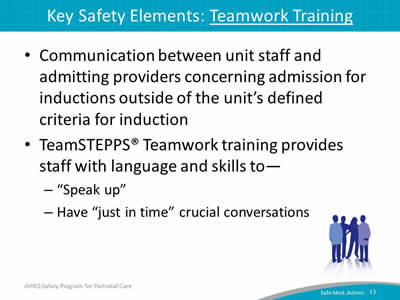
- Communication between unit staff and admitting providers concerning admission for inductions outside of the unit’s defined criteria for induction.
- TeamSTEPPS® Teamwork training provides staff with language and skills to—
- "Speak up."
- Have "just in time" crucial conversations.
Slide 14: Key Safety Elements: Teamwork Training
- Have situational awareness during oxytocin use. This includes—
- Staff alertness for early signs of nonreassuring fetal or maternal status.
- Knowing the plan for a timely response to prevent further deterioration.
- Use SBAR, callouts, huddles, and closed-loop communication techniques. Useful for—
- Communicating sense of urgency.
- Briefing arriving care team members.
Slide 15: Key Safety Elements: Teamwork Training
- Communicate during transitions of care. Ensures a shared mental model of plan of care and perceived risks—
- Between shifts.
- Between units.
- Between individuals within the same unit.
- Have high-reliability teams.
- Anyone can sound an alarm, request help, or challenge the status quo.
- Hierarchy is minimized.
- Communication is continuous, valued, and expected.
Slide 16: Key Safety Elements: Patient and Family Engagement
- Discuss risks and benefits of oxytocin use for labor induction or augmentation with patient.
- Provide patient/family education regarding oxytocin use.
Slide 17: Tool: Safe Oxytocin Administration
- Provides additional details about the six key safety elements and ways they can be customized based on unit needs or preferences.
- Offers a sample oxytocin administration procedure in the appendix to demonstrate how key safety elements can be customized and operationalized within a unit procedure for safe oxytocin administration.
Slide 18: Magnesium Sulfate
Magnesium Sulfate
Slide 19: Rationale for Safe Medication Administration Tool
- Like oxytocin, magnesium sulfate is a high-alert medication.
- Magnesium is commonly used on L&D units, but administration procedures vary greatly due to lack of standardization, local culture, and individual provider training and preferences.
- Magnesium has a narrow therapeutic window requiring careful attention to appropriate administration.
Slide 20: Key Safety Elements: Standardize When Possible
- Standard criteria established, met, and documented for magnesium sulfate use.
- Uniform and standard drug packaging, preparation, and labeling.12,13
- Standardization of magnesium sulfate dosing using a calibrated infusion pump with free flow protection.
- Limit the number of different kinds of pumps in use.
- Avoidance of high-risk practices, such as using the maintenance infusion for a manual bolus.14
Slide 21: Key Safety Elements: Standardize When Possible
- Immediate removal of the magnesium line from the intravenous port when therapy is discontinued.
- Uniform parameters for maternal and fetal monitoring and provider notification prior to initiation of magnesium sulfate and during infusion.
- Standardization of the unit for laboratory reporting of serum magnesium levels (e.g., mg/dl, mEq/L, or mmmol/L).14
Slide 22: Key Safety Elements: Create Independent Checks
- Assessment of appropriateness of patient magnesium use by staff other than the ordering provider.
- Use of preprinted orders or electronic order entry for magnesium sulfate order.
- Use of independent verification whenever there is a rate change or a new magnesium sulfate bag is hung.14
Slide 23: Key Safety Elements: Create Independent Checks
- Maternal and fetal monitoring using unit-established standard parameters at regular intervals.
- Unit-established process for timely provider notification and response expectations.
- Standing orders for nurses to respond to signs and symptoms of magnesium toxicity, with quick access to antidote.
Slide 24: Key Safety Elements: Learn From Defects
- Debrief near misses and adverse events related to magnesium sulfate use.
- Put process in place to review—
- Use of magnesium sulfate outside of defined indications.
- Severe maternal or neonatal morbidity and mortality events.
- Share outcomes or process improvements from the informal (debriefing) and formal analysis with staff to achieve transparency and organizational learning.
Slide 25: Key Safety Elements: Simulation
- Two sample scenarios related to magnesium sulfate use are available through the SPPC. One focuses on magnesium toxicity, and one focuses on preeclampsia/seizure. These scenarios reinforce teamwork and communication related to the following:
- Situational awareness.
- Ability to get additional help quickly.
- Timely use of standing orders for managing magnesium sulfate toxicity.
- Communication with rapid responders.
- Communication with patient/family.
Slide 26: Key Safety Elements: Teamwork Training
- Have situational awareness during magnesium sulfate use.
- Use SBAR and closed-loop communication techniques.
- Communicate during transitions of care.14
- Have high-reliability teams.
Slide 27: Key Safety Elements: Patient and Family Engagement
- Discuss risks and benefits of intrapartum or postpartum magnesium sulfate use.
- Provide patient/family education regarding magnesium sulfate use.
Slide 28: Tool: Safe Magnesium Sulfate Administration
- Provides additional details about the six key safety elements and ways they can be customized based on unit needs or preferences.
- Offers a sample magnesium sulfate administration procedure in the appendix to demonstrate how key safety elements can be customized and operationalized within a unit procedure for safe magnesium sulfate administration.
Slide 29: Customizing the Key Elements
- Adjust the assessment frequency, parameters, or criteria for provider notification.
- Adjust the dosages administered under the protocol.
- Adjust the standing orders for nursing response to tachysystole, seizure, or magnesium toxicity.
- Add additional items under patient/caregiver teaching and communication.
- Build content into the facility’s existing documentation systems.
Slide 30: Unit Next Steps
- Decide whether to select the safe medication administration bundle for implementation locally. Consider these factors:
- Unit data suggesting adverse events or near misses related to oxytocin, magnesium sulfate, or both.
- Synergy with related or similar initiatives (e.g., initiatives to reduce early elective deliveries, other medication safety initiatives).
- Interest and enthusiasm of unit staff for implementing.
Slide 31: Unit Next Steps
- Review key safety elements of tool with implementation team, consider any facility policies or processes, and customize procedures for use within the unit.
- Support implementation of unit procedure.
- Staff training/communication.
- Simulation.
- Monitor implementation progress and impact, collect data for quality improvement.
Slide 32: Tips for Implementation Success
- Use CUSP principles for implementing teamwork and communication (e.g., incorporating diverse perspectives) to develop consensus on the "content" of the unit’s approach to oxytocin and magnesium sulfate administration.
- Pilot test any new procedures on a limited scale to work out any bugs or problems.
- Comprehensively review the unit procedures each year to assess the need for updates.
- Create a mechanism for identifying recurrent nonuse or deviation from the established procedure by clinicians.
- Seek to understand why, rather than assign blame.
Slide 33: References
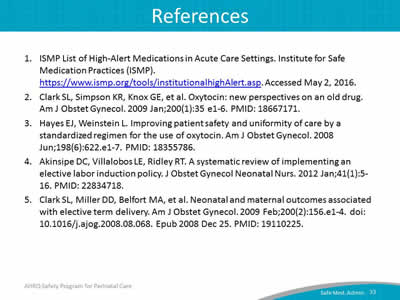
- ISMP List of High-Alert Medications in Acute Care Settings. Institute for Safe Medication Practices (ISMP). https://www.ismp.org/tools/institutionalhighAlert.asp. Accessed May 2, 2016.
- Clark SL, Simpson KR, Knox GE, et al. Oxytocin: new perspectives on an old drug. Am J Obstet Gynecol 2009 Jan;200(1):35 e1-6. PMID: 18667171.
- Hayes EJ, Weinstein L. Improving patient safety and uniformity of care by a standardized regimen for the use of oxytocin. Am J Obstet Gynecol 2008 Jun;198(6):622.e1-7. PMID: 18355786.
- Akinsipe DC, Villalobos LE, Ridley RT. A systematic review of implementing an elective labor induction policy. J Obstet Gynecol Neonatal Nurs 2012 Jan;41(1):5-16. PMID: 22834718.
- Clark SL, Miller DD, Belfort MA, et al. Neonatal and maternal outcomes associated with elective term delivery. Am J Obstet Gynecol 2009 Feb;200(2):156.e1-4. doi: 10.1016/j.ajog.2008.08.068. Epub 2008 Dec 25. PMID: 19110225.
Slide 34: References
- Bailit JL, Gregory KD, Reddy UM, et al. Maternal and neonatal outcomes by labor onset type and gestational age. Am J Obstet Gynecol 2010 Mar;202(3):245.e1-245.e12. doi: 10.1016/j.ajog.2010.01.051. PMID: 20207242.
- Caughey AB, Sundaram V, Kaimal AJ, et al. Maternal and neonatal outcomes of elective induction of labor. Evidence Report/Technology Assessment No. 176 (Prepared by the Stanford University-UCSF Evidenced-based Practice Center under contract No. 290-02-0017.) AHRQ Publication No. 09-E005. Rockville, MD: Agency for Healthcare Research and Quality. March 2009. http://www.ahrq.gov/research/findings/evidence-based-reports/eiltp.html. Accessed May 2, 2016.
- Budden A, Henry A, Heatley E. Oxytocin infusion regimens for induction of labour. Cochrane Database Syst Rev 2012;3:CD009701. DOI: 10.1002/14651858. CD009701. PMID: 25300173.
- Kenyon S, Tokumasu H, Dowswell T, et al. High-dose versus low-dose oxytocin for augmentation of delayed labour. Cochrane Database Syst Rev 2013 Jul 13;7:CD007201. doi: 10.1002/14651858.CD007201.pub3. Review. PMID: 23853046.
Slide 35: References
- ACOG Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No.107: Induction of labor. Obstet Gynecol 2009 Aug, reaffirmed 2015;114(2 Pt 1):386-97. doi:10.1097/AOG.0b013e3181b48ef5. Review. PMID: 19623003.
- Clark S, Belfort M, Saade G, et al. Implementation of a conservative checklist-based protocol for oxytocin administration: maternal and newborn outcomes. Am J Obstet Gynecol 2007;197:480.e1-480.e5. PMID: 17980181.
- Institute of Medicine (US) Committee on Quality of Health Care in America; Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington (DC): National Academies Press (US); 2000. PMID: 25077248.
- Failure to Set a Volume Limit for a Magnesium Bolus Dose Leads to Harm. Acute Care ISMP Medication Safety Alert. June 3, 2010. http://www.ismp.org/Newsletters/acutecare/articles/20100603.asp. Accessed May 2, 2016.
- Simpson KR, Knox GE. Obstetrical accidents involving intravenous magnesium sulfate: recommendations to promote patient safety. MCN Am J Matern Child Nurs 2004 May-Jun;29(3):161-9; quiz 170-1. PMID: 15123972.
Slide 36: Disclaimer
Every effort was made to ensure the accuracy and completeness of this resource. However, the U.S. Department of Health and Human Services makes no warranties regarding errors or omissions and assumes no responsibility or liability for loss or damage resulting from the use of information contained within.
The U.S. Department of Health and Human Services cannot endorse, or appear to endorse derivate or excerpted materials, and it cannot be held liable for the content or use of adapted resources. Any adaptations of this resource must include a disclaimer to this effect.
Reference to any specific commercial products, process, service, manufacturer, company, or trademark does not constitute endorsement or recommendation by the U.S. Government, HHS, or AHRQ of the linked Web resources or the information, products, or services contained therein. The Agency does not exercise any control over the content on these sites.



