Rapid Response for Perinatal Safety: Facilitator Guide
AHRQ Safety Program for Perinatal Care
Slide 1: AHRQ Safety Program for Perinatal Care
Say:
The Rapid Response for Perinatal Safety bundle provides information establishing a unitwide approach, also referred to as a rapid response system, for responding to urgent maternity care issues.
Slide 2: Learning Objectives
Say:
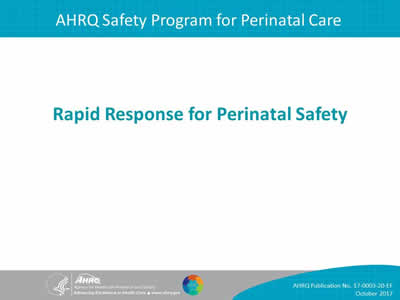
In this module, we will do the following:
- Define components of a rapid response system.
- Identify the key safety elements of a robust rapid response system.
- Identify ways to apply key safety elements to your unit procedures for rapid response to urgent maternity care issues.
Slide 3: Rapid Response
Say:
- Rapid response for maternal and fetal physiologic deterioration and urgent conditions are the focus of this bundle of the AHRQ Safety Program for Perinatal Care, or SPPC.
- The training materials and tools in this bundle review the key elements of a rapid response system or RRS, within the framework of the Comprehensive Unit-based Safety Program, or CUSP.
- The key safety elements provide a comprehensive starting point for each unit to consider as it establishes its processes for ensuring rapid response capabilities.
Slide 4: Rapid Response System
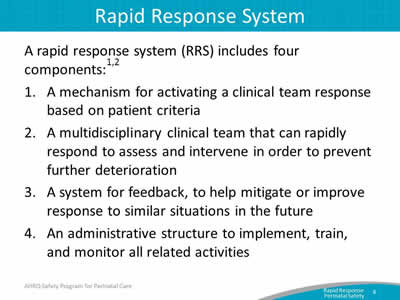
Say:
To start, we will define what makes up a rapid response system. In general terms, a rapid response system includes the following four components:
- A mechanism for activating a clinical team response based on patient criteria. Activation can result from concerns identified by the primary clinical staff caring for the patient but may also include activation by patients, family members, or others supporting the patient.
- A clinical team that can rapidly respond to assess and manage a patient who is deteriorating physiologically. A key element of any rapid response system is to have a planned, multidisciplinary team response that can assess and intervene to prevent further maternal or fetal physiologic deterioration.
- A system for feedback, to help mitigate or improve response to similar situations in the future. A rapid response system is more than a team that responds to emergencies. It involves feedback and monitoring to continually improve overall care.
- An administrative structure to implement, train, and monitor all related activities. For rapid response systems to be sustainable, they need ongoing support, resources, and governance.
Slide 5: Obstetrical RRS
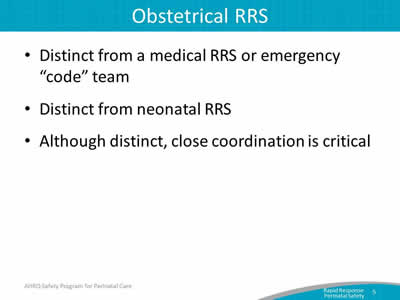
Say:
A rapid response system and teams that provide a rapid response for maternity care urgencies and emergencies are somewhat different from other types of medical emergencies that activate “code” teams. A rapid response system is intended to assess a greater number of patients, with a broader range of issues than most medical “code” teams assess. The intent of a rapid response is to intervene earlier than a cardiopulmonary arrest, with the aim of preventing further deterioration. With respect to obstetrical rapid response, the aim is to assess and intervene early, before a serious maternity care crisis or emergency occurs. However, maternity patients can experience nonobstetrical care conditions and emergencies while pregnant, in labor, and postpartum; thus, close coordination with medical rapid response and “code” teams is critical.
Similarly, obstetrical rapid response systems are distinct from neonatal rapid response systems. Neonatal rapid responders typically assume care and responsibility for neonates immediately after birth. Obstetrical rapid response systems are developed in order to intervene when maternal OR fetal physiologic deterioration is occurring; thus, some patients may require activation of both a neonatal rapid response AND an obstetrical rapid response to coordinate response and care.
Slide 6: Evidence for RRS
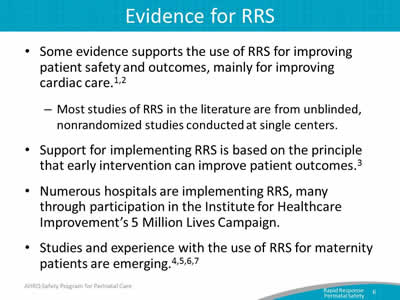
Say:
Some evidence supports the use of rapid response systems for improving patient safety and outcomes, mainly for improving cardiac care.
- Most studies of rapid response systems in the literature are from unblinded, nonrandomized studies conducted at single centers.
Support for implementing a rapid response system is based on the principle that early intervention can improve patient outcomes, and numerous hospitals are implementing rapid response systems, many through participation in the Institute for Healthcare Improvement’s 5 Million Lives Campaign.
- Studies and experience with the use of rapid response systems for maternity patients is emerging.
Slide 7: RRS Tool
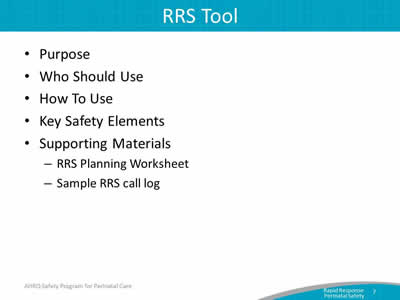
Say:
The purpose of the Rapid Response System tool is to provide a framework for establishing a rapid response system.
This framework is based on SPPC key safety elements that describe what should be included to create a rapid response system.
Nurses, physicians, midwives, anesthesiology providers, neonatal providers, and other labor and delivery or L&D unit staff responsible for antepartum, intrapartum, and postpartum care can use this tool.
We will review the key safety elements in more detail in subsequent slides.
The key safety elements should be reviewed with L&D leadership, relevant unit staff, and staff outside the L&D unit that may be involved with a rapid response system to determine how the elements will be implemented within a hospital.
Two supporting materials, the Obstetrical Rapid Response System Planning Worksheet and the Rapid Response Call Log, are also provided in the Appendix of this tool.
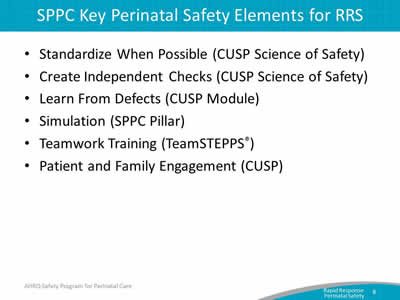
Slide 8: SPPC Key Perinatal Safety Elements for RRS
Say:
As in the other customizable bundles available through the SPPC, the key safety elements for Rapid Response for Perinatal Safety are organized into the following six overarching principles of patient safety derived from the Comprehensive Unit-based Safety Program (CUSP), the TeamSTEPPS® teamwork and communication system. They include the following:
- Standardize When Possible.
- Create Independent Checks.
- Learn From Defects.
- Simulation.
- Teamwork Training.
- Patient and Family Engagement.
In the rest of this presentation, we will highlight each of these key safety elements and how they apply to establishing a rapid response system.
Slide 9: Key Safety Elements: Standardize When Possible
Say:
The first consideration in establishing a rapid response system is to standardize when possible.
This is a core principle from the CUSP Science of Safety module. Standardizing procedures reduces and alleviates duplications of labor and resources, reduces unwarranted variation among providers and staff, and offers a predictable approach that encourages a shared mental model across the unit.
One consideration is establishing a standard unitwide approach for responding to a request for a rapid response.
- The standard unitwide approach could be part of a hospital’s larger rapid response system, with modifications to be specific to responding to maternity care issues, or could be separate.
- A standard unitwide approach also means that that there is a uniform way primary staff (or patients or family) request a rapid response from other clinicians. When a request is made, staff individually and collectively know who is responsible for responding and expectations for the response, uniform expectations for documentation of the rapid response event exist, and a system for feedback exists to monitor and improve the approach.
Slide 10: Key Safety Elements: Standardize When Possible
Say:
There also needs to be standard criteria for activation of a rapid response. Rapid response activation criteria can be general or specific.
Language describing general activation criteria examples include—
- An emergent or potentially emergent maternity care condition.
- An event that requires a team response.
- An acute situation that the physician or nurse, or patient or family members believe need immediate evaluation and response to avoid fetal or maternal harm or further deterioration.
Language describing specific activation criteria examples include—
- Category III FHR tracing.
- Bright red vaginal bleeding.
- Severe abdominal pain.
- Uterine tachysystole.
- Inability to complete delivery (e.g., with a shoulder dystocia).
- Cord prolapse.
- Hypotension.
- Consistently rising blood pressure.
- Severe headache.
- Inability to control pain.
- Seizure.
It is also important to define patient criteria for which a medical rapid response team, or medical emergency code team, should be activated—for example, cardiac or pulmonary deterioration or arrest.
Slide 11: Key Safety Elements: Standardize When Possible
Say:
It may also be beneficial for staff to adopt standard rapid response kits or carts in their unit. These can be kits or carts that are stocked with supplies, equipment, and cognitive aids that might be used for the more common situations that might activate a rapid response.
Slide 12: Key Safety Elements: Create Independent Checks
Say:
The second consideration is to create independent checks.
This can be done though the inclusion of multidisciplinary rapid responders, who serve as a second opinion, additional resources, and another set of "eyes" on the situation in order to prevent further deterioration and "failure to rescue."
Rapid responders may include staff L&D nurses, nurse midwives, obstetricians, and anesthesiology providers.
In general, rapid responders should—
- Possess specialized maternity care clinical skills, knowledge, and equipment.
- Be able to assess and manage a maternity patient who has deteriorated physiologically.
- Be able to intervene to minimize risk of serious harm and further deterioration.
Slide 13: Key Safety Elements: Create Independent Checks
Say:
Different models for the multidisciplinary team of responders exist and can vary by the following:
- Volume and complexity of maternity patients cared for.
- Availability of in-house obstetric hospitalists (also called laborists) and dedicated L&D anesthesiology support.
- Presence of graduate medical education or nurse midwifery programs with in-house residents or students.
- Other available hospital rapid response teams.
Core rapid response staff typically includes a maternity care provider (obstetrician or midwife) and a staff L&D nurse. A midwife can often serve as an initial rapid responder, but for some activations, an obstetrician or surgeon qualified to perform a cesarean section or other surgical interventions will be needed.
- Other responders may include an anesthesiology provider, an L&D or operating room technician, additional L&D staff nurses, or surgeon with advanced gynecological surgery skills.
- The L&D unit should establish the scope and limits of rapid responders:
- Rapid responders can simply provide role backup and task assistance to the primary maternity care provider and L&D staff nurse, or rapid responders may assume responsibility for directing patient care. The scope and role may vary depending on the unit to which the rapid responders deploy (e.g., L& D, antepartum, postpartum, or emergency department).
- Limits to the situations rapid responders are qualified to address and interventions they are able to execute should also be articulated as part of the scope of a rapid response system.
Slide 14: Key Safety Elements: Learn From Defects
Say:
The third consideration for rapid response systems is to learn from defects.
This is also a core principle from CUSP. This principle calls for L&D unit teams to evaluate their processes and learn from adverse events, errors, and near misses and, when possible, to share what they learn. Learning from defects includes using both informal and formal processes that seek to understand rather than to shame and blame individuals.
The L&D unit can decide its approach to learning from defects based on seriousness of event, expertise available, and data monitoring and tracking capabilities. Options include the following:
- Informal debriefings by clinical team immediately following a rapid response, regardless of the patient outcome. This allows for understanding of what went well, what could have gone better, and what could be done differently next time. A sample rapid response call log form that can be used as part of the debriefing is provided as an appendix to the Rapid Response toolcall
- In addition, clinical teams can debrief and analyze near misses and adverse events, regardless of whether a rapid response was activated.
In additional to clinical debriefings, a regular forum with a multidisciplinary team for reviewing serious maternal or neonatal adverse outcomes using formal methods of analysis reviewed in prior presentations can be used for learning from defects and sensemaking.
- Discovery Form.
- Root Cause Analysis.
- Eindhoven Model.
- Failure Mode and Effects Analysis.
- Probabilistic Risk Assessment.
- Causal Tree Worksheet.
- Interdisciplinary Case Reviews.
Last, staff should share outcomes of process improvement from informal and formal debriefings and analysis with staff to achieve transparency and organizational learning.
Slide 15: Key Safety Elements: Simulation
Say:
Another key safety element related to rapid response systems is conducting simulations. Simulations can be used to practice and train teams on rapid response processes.
Many of the sample scenarios available through the SPPC can be used for simulating situations in which a rapid response should be activated. Individuals and teams can use these scenarios to gain experience both as activators of a rapid response and as responders to an activation request.
Through simulation, one can reinforce teamwork and communication related to the following:
- Situational awareness.
- Ability to get additional help quickly and activate a rapid response based on unit-established criteria and processes for activation.
- Communication between primary care team and rapid responders.
- Communication with patient/family.
- Use of briefings, huddles, and debriefings.
Slide 16: Key Safety Elements: Teamwork Training
Say:
The fifth consideration for rapid response systems is teamwork training. This aspect of perinatal safety calls for L&D units to foster a culture of teamwork and communication to promote effective teamwork.
Elements of teamwork training that are important for an effective rapid response systems are—
- Situational awareness. This refers to all staff caring for the patient knowing what the patient’s plan is through briefings and team management, being aware of what is going on and what is likely to happen next, verification and check-back on information, and providing ongoing updates. In the context of rapid response, situational awareness may often result in a decision to activate a rapid response.
- Use SBAR or Situation, Background, Assessment, and Recommendation as well as callouts, huddles, and closed-loop communication among team members.
- Use of transition communication techniques to ensure a shared mental model of plan of care and perceived risks between shifts, between units, and between care teams within a unit. This includes communication between primary team and rapid responders, or between rapid responders and OR team.
- Finally, the use of high-reliability teams is a critical aspect of an effective rapid response.
Slide 17: Key Safety Elements: Teamwork Training
Say:
Characteristics of high reliability teams include:
- Anyone can sound an alarm, request help, or challenge the status quo.
- Hierarchy is minimized.
- Communication is continuous, valued, and expected.
In a high-reliability team, team members protect one another from work overload and place requests or offers for assistance in the context of patient safety. Further, it is expected that assistance will be actively sought and offered. A rapid response system offers a formalized way of requesting assistance.
In addition, team members will advocate for the patient when one person’s viewpoint does not coincide with another’s.
Team members must also manage conflict using a constructive positive approach to emphasize "what is right, not who is right."
Slide 18: Key Safety Elements: Patient and Family Engagement
Say:
The final safety element is patient and family engagement.
To engage patients and family in a rapid response system, units may consider including patient and family member activation criteria for a rapid response in addition to patient- and family-specific instructions for activating, which are explained upon admission or after unit transfers.
Communication with the patient and family during a rapid response, including assigning a staff member to communicate with the family during the response, and providing ongoing reassurance.
Likewise, a unit must be ready to disclose any unintended outcomes.
The unit-established process for disclosing unintended outcomes may include the following:
- Prompt, compassionate, and honest communication with the patient and family.
- Investigation.
- Ongoing communication with the patient and family.
- Apology and remediation.
- System and process improvement.
- Measurement and evaluation.
- Education and training.
Slide 19: Unit Next Steps
Say:
The unit’s next steps:
- Decide whether to select the rapid response system bundle for implementation locally. Consider these factors:
- Unit data suggesting adverse events or near misses that may have been minimized or averted as a result of a rapid response intervention.
- Synergy with related or similar initiatives or hospital rapid response systems.
- Interest and enthusiasm of unit staff and administration for implementing.
Slide 20: Unit Next Steps
Say:
- Staff should review key safety elements of the rapid response tool, including the Planning Worksheet and Sample Call Log available as an appendix in this tool.
- Support implementation of unit systems:
- Staff training/communication.
- Simulation.
- Monitor implementation progress and impact, collecting data for quality improvement to refine the unit approach to the safe use of electronic fetal monitoring.
Slide 21: Tips for Implementation Success
Say:
Here are tips for implementing a unit’s tools successfully:
- Staff should use CUSP principles for implementing teamwork and communication (e.g., incorporating diverse perspectives) to develop consensus on activation criteria and response approach, and response expectations.
- Provide education and training to staff on the use of the rapid response system and make routine education for patients and family on the rapid response activation a part of the admission process.
- Regularly debrief after rapid response events, and solicit ongoing feedback from staff and patients.
Slide 22: References
Slide 23: Disclaimer