Questionnaire Results
Nine questionnaires were sent out, all were returned. The responses to our questionnaire were used extensively to develop the tools and conclusions presented here. A summary of the important themes in the responses includes:
- Planning is best done in advance and should involve all potential participants including care providers, emergency managers, emergency medical services, law enforcement, and others.
- Ideally, the role of the ACF should be decided in advance of an incident. This will guide staffing, supply and equipment decisions, and procurement. Possible roles for the ACF include:
- Ward-level care to decompress a hospital and provide surge.
- Ambulatory acute care - i.e., triage and minor wound care.
- Chronic care.
- The ACF will usually have to care for the full age range of patients: children, adolescents, adults, and the elderly. This should be taken into account in all planning.
- Even with the best of plans, overall flexibility is mandatory and should be maintained.
- If possible, a college campus would make an excellent ACF because of the availability of appropriate space, human resources, food service, security, bathrooms, and showers.
- Proximity to a hospital is desired if diagnostic tests will be needed that cannot be administered at the ACF.
- Point of care clinical laboratory testing should be considered. At a minimum, glucometers for measuring blood glucose should be available.
- Adequate toilet and shower facilities are very important.
- The nature of the disaster may dictate that nursing home patients are cared for en masse at an ACF.
- Lighting control and noise control are issues that may be difficult to solve if the ACF is housed in a single large area (such as a gymnasium).
- It is usually best to try to keep families together.
- If palliative care will be necessary, those patients should be cohorted, preferably in a separate area or unit.
- Caring for patients' pets should be considered.
- Security is extremely important. Individuals in uniforms (even if not true security) can assist with this. Law enforcement should be included in any advance planning with a commitment to provide security for any ACF.
- Incident command of an ACF is probably best done by a physician or nurse who understands both incident command and patient care issues.
- In most situations, pediatric patients made up about 10% of patients.
- Chronic-care medications (e.g., for hypertension, diabetes mellitus, etc) are extremely important as are pain medications and antibiotics.
- Replenishing narcotics at an ACF may be an issue due to Drug Enforcement Administration regulations. This should be investigated as part of the planning process.
- Most medical providers worked 12 hour shifts with decreased staff during the night.
- Chronic dialysis may become a significant chronic-care issue.
- Although ACF incident command usually works well, there are sometimes issues interfacing with local area command.
- Early establishment of rules of behavior for the ACF ("House Rules") is mandatory for smooth operation.
A more complete enumeration of the (de-identified) questionnaire results is provided in Appendix D.
Alternate Care Facility Selection Tool
The original version of the ACF selection tool was developed under an earlier AHRQ contract in 2004.1 That tool is a simple spreadsheet with the potential site specific factors listed on the vertical axis and the different potential sites listed on the horizontal axis. Each factor is scored on a scale of 0 to 5 for each site representing how closely each factor at the site in question approximates that of a hospital. These values were then summed for each site. Since the release of the initial site selection tool, many States and communities have used the tool as a starting point for ACF site selection including California, Illinois, Florida and Washington with several additions and improvements.
Based on responses to the questionnaire as well as information provided from several States, no deletions of ACF factors were made in the new facility selection tool and several additions were made. The new tool is offered in both an Excel version and a Web-based version. The tool was reformatted for the inclusion of general demographic information for each potential facility and better visual grouping of the evaluation factors in the five categories of site infrastructure, total space and layout, utilities, communication, and other services (Figure 1 shows the Web version of this page.).
Figure 1—Facility selection tool for a single potential ACF (Web version)
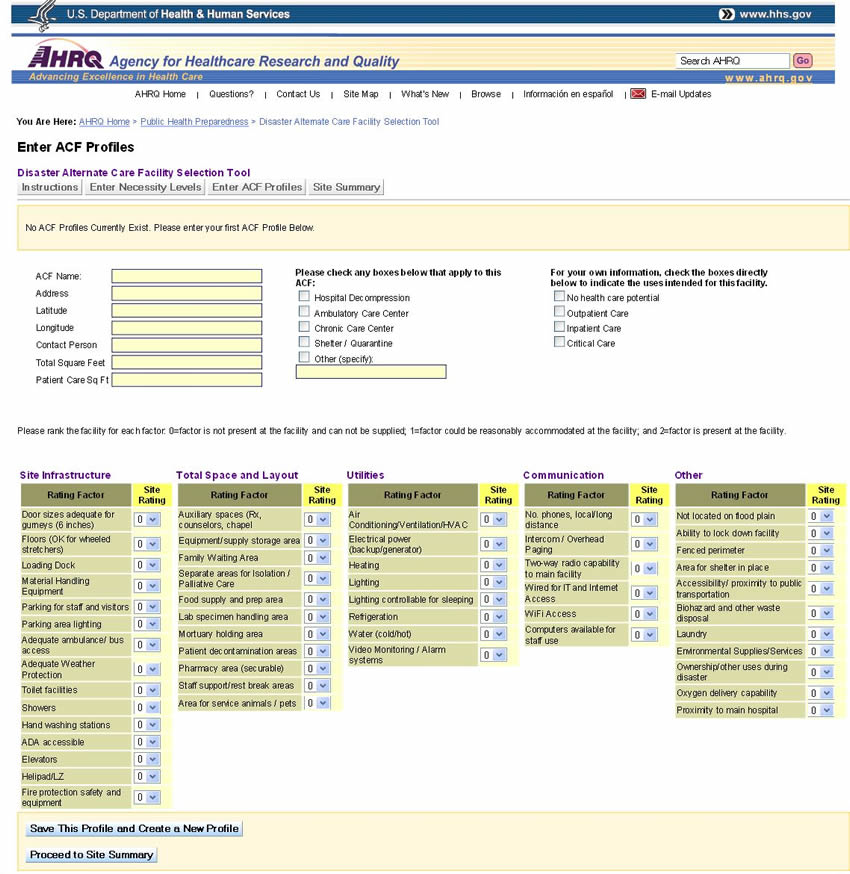
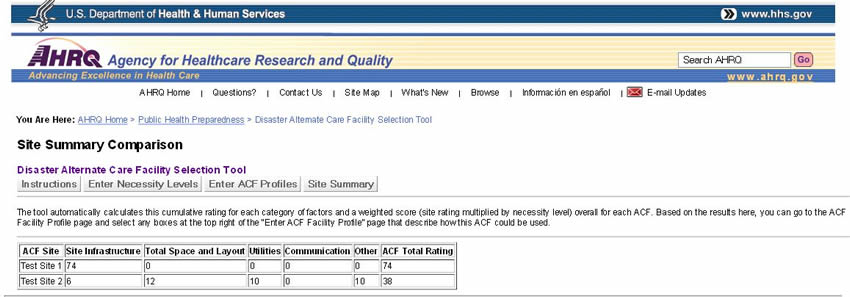
The factor rating system was also simplified to a three-level scoring range in which 0=factor not present, 1=factor not present but easily provided for, and 2=factor present. For certain types of disasters, for certain populations or in certain situations, some factors are not necessary while others may be of extreme importance. To address this issue, a factor "Necessity Level" was established to indicate the importance of the factor in the evaluation of a candidate site for a specific incident or specific use. The Necessity Level can be a value from 0 to 5, with 5 being the highest/most important and 0 being not necessary. In this schema, a value of 3 could represent a factor that is desired but not absolutely required. For each factor evaluated, the selection tool produces a product of the rating value and the Necessity Level resulting in a weighted score that can be a value from 0 to 10. These weighted scores are then totaled for each category and for the facility overall. A 'Facility Summary' section provides an automatically generated facility evaluation summary which allows easy comparison of the summary data for however many potential facilities the user has entered (Figure 2 shows the Web version of the summary). Step-by-step user instructions for the tool are at the "Instructions" tab on the tool.
Figure 2: Facility Evaluation Summary
Alternate Care Facility Operations Template
A major aspect of successful operation of an ACF is the preparation and use of an operations guide (referred to as a "concept of operations" or "ConOps"). Each implementation of an ACF is unique and dependent on the population served, the nature of the disaster, the duration of operation, and other factors. Thus, it is not possible to provide a "one-size-fits-all" operations guide; however, we have attempted to develop a template for such a document, which is provided below. This template should be altered during the planning phase to reflect local variables and the planned use of the ACF.
Introduction
A catastrophic man-made or natural event that produces a large number of ill or injured victims could cause a deficit in the bed capacity of health care facilities and organizations. In order to meet the surge of patients and provide for the medical care needed in such an event, emergency preparedness and response authorities, including hospitals and health care organizations, must develop response capabilities that include the development, implementation, and operation of ACFs that will augment the existing health care delivery services. This section serves as an initial template for the description and operation of such a facility.
ACF Concept Overview
An ACF is a temporary health care delivery site that usually is set up either in a non-traditional patient care location within a health care organization or in an existing structure ("building of opportunity") that may or may not be directly on the campus of existing health care facilities, that has adequate utilities or where adequate utilities can be provided, and that serves to either augment existing health care services that have been overwhelmed with a surge of patients or to replace health care delivery facilities that have been damaged or destroyed in the incident.
An ACF can help provide a focused, timely medical response to a mass casualty catastrophe by expanding the surge capabilities and assets of local health care providers and agencies. When integrated with acute care and public health preparedness, the ACF can aid in mitigating the effects of a mass casualty event by easing the patient burden on local medical facilities, enhancing the capability to provide quarantine, caring for large numbers of low acuity patients, and relieving the medical care infrastructure so it can focus care on more critical patient medical needs.
Assumptions
A number of basic assumptions can be made in the event of a mass casualty event:
- A large-scale natural or man-made disaster or attack is likely to produce casualty numbers that overwhelm routine medical response resources.
- Surge bed capacity in hospitals is limited.
- Hospital resources will need to be redirected to care for the more seriously ill
- Assistance from outside of the impacted area, if available, may be needed to care for lower acuity patients.
- A system to rapidly expand health care delivery services is necessary to treat a large affected population.
- This expanded health care delivery system is developed and used in conjunction with local emergency management, emergency medical services, and public health agencies.
ACF Basic Functions
The ACF may serve any one of several health care delivery functions during a mass casualty event, including provision of:
- Bed capacity and surge relief by offering non-acute (ward) inpatient services to allow for decompression of existing hospitals or to augment in-patient ward care capacity.
- Primary medical care and behavioral/mental health services for persons and residents with pre-existing chronic diseases who, as a result of the event, are unable to access their routine sources of health care, including supportive care for family members and pets.
- Primary medical care and behavioral/mental health services for displaced or sheltered special needs persons with chronic diseases, limited mobility, or other impairments making them unqualified for general population shelters, including supportive care for family members and pets.
- Pre-hospital evaluation and triage services to determine the need for hospital care.
- Evaluation and support to isolation and quarantine operations.
- Provide a site for mass immunization and prophylaxis and point of dispensing services for mass medication distribution.
- Bed capacity and surge relief by offering acute, intensive care level services to allow for decompression or existing hospitals or to augment in-patient intensive care unit capacity.
- Community outreach to, and assessment of, affected populations.
Description of an ACF
Mission
An ACF will provide health and medical care to those patients who have medical, behavioral/mental health, or other health-related needs that cannot be accommodated or provided for with the existing medical care capabilities or in the general shelter population. An ACF is designed to provide health and medical care for patients with needs such as:
- Conditions that require observation, assessment, or maintenance.
- Chronic conditions that require assistance with the activities of daily living and do not require hospitalization.
- Medications and vital sign monitoring that cannot be provided at home.
- Conditions that require the level of care provided by the ACF.
An ACF is not, in most cases, a substitute for an acute care hospital or emergency department.
Scope of Care
Non-Critical Care Capability. The ACF can be used to assist in providing bed capacity for hospital relief and may offer non-ambulatory care, ambulatory care, inpatient ward-level care, outpatient care, or some combination thereof. The staffing, supplies and equipment of an ACS result in a limited scope of care for hospital relief. The scope of care includes:
- nursing care for stabilized internal medicine, trauma, orthopedic, and obstetric patients;
- medical workups and examinations required during recovery or preoperative cases;
- nursing care for special needs patients;
- administration of treatments;
- administration of vaccines or other countermeasures; and
- preparation for transport for patients who require transfer to hospitals.
The ACF does not provide surgical or intensive/critical care. If provided, the equipment and supplies may allow for resuscitative intervention if needed in individual cases.
Intensive Care Capability. The ACF may be used to assist in providing acute or intensive care level of services for hospital relief. The staffing, supplies, and equipment of an ACS must be appropriately increased to provide such intensity of care. In rare instances when staffing, supplies, and infrastructure permit, the ACF may be configured to provide surgical intervention. The scope of care for such a configuration includes:
- Administration of intravenous medications and drips;
- Cardiac monitoring; and
- Ventilator support.
Quarantine Capability. The ACF may provide support to quarantine operations with the capability to evaluate and hold persons suspected of being either exposed to or affected by a quarantine disease. The ACF, when located in an appropriate building of opportunity, equipped with staff, and provided with service support facilities enables:
- Holding and segregation of persons;
- Taking of biological samples for submission to local, State or Federal laboratories;
- Short-term isolation of patients pending transfer to a hospital isolation ward;
- Personal respiratory protection to ACF staff and quarantine subjects;
- Vaccination or administration of other countermeasures; health communications;
- Security and safety of subjects and staff;
- Reasonable comfort of subjects;
- Containment and security of luggage while in quarantine, with reasonable owner access.
Since the ACF's capability is finite and relatively small in terms of numbers of beds, its utility in a large-scale pandemic response would be limited.
Staffing Framework
Personnel Requirements
Enormous numbers of patients seeking treatment during a disaster will cause hospitals to fill to capacity. Available staff will be fully engaged. Planning efforts for implementing an ACF will need to specify where additional staff may be obtained for ACF staffing. An affected community may not have the staffing resources to activate an ACF independently, so staffing may have to come from outside the affected area. The staffing plan needs to identify projected health and medical staffing shortfalls.
ACF Staff Skill Mix
The ACF is staffed to maximize the use of limited staffing resources, not only to provide for an expected large quantity of patients, but also to ensure sustainability while providing the highest quality care possible given the limited resources. The staff skill mix should be appropriate to serve patients admitted to the ACF facility within the scope of care planned for the ACF. The issue of personnel requirement and staff skill mix are discussed in further detail elsewhere in this report.
ACF Staff Activation
ACF staff members will, in most cases, be activated by the agency or organization responsible for implementation of the ACF. Ideally, notification of staff will be accomplished by contacting each team member via cell phone, work phone, home phone, or e-mail to provide activation information or by using other agency-specific internal procedures to activate the team. On activation, ACF staff members should report to the specified location for assignment.
Risk Analysis
All ACF staff activities involve variables and unknowns which may have a substantial impact on the health and welfare of staff members. These potential risks require frequent identification, assessment, analysis, and planning to minimize their impact. Risks should be assessed based on the likelihood of occurrence and potential severity. A mitigation plan for each risk should be developed to reduce the likelihood or severity of each risk.
ACF Command and Control
Overview
Homeland Security Presidential Directive-5 (HSPD-5) provides a National Incident Management System (NIMS) through which all incident response agencies and assets are to be integrated and coordinated.
Operating under NIMS principles, each ACF will be integrated into the Incident Command System (ICS) structure implemented in the local community for response to the incident.
Internally, each ACF will follow an ICS structure for a public health or medical emergency and provide necessary operations as stated in the incident action plans (IAPs) for the specific event. The Hospital Incident Command System (HICS) provides a template for applying the Incident Command System to the health care setting at. http://hicscenter.org/SitePages/HomeNew.aspx.
Each ACF using HICS is organized into an ICS structure that includes command staff with public information, safety, and liaison officers; general staff assigned to operations, planning, logistics, and finance/administration sections; and a medical technical specialist as needed.
Figure 3: Command Staff and General Staff
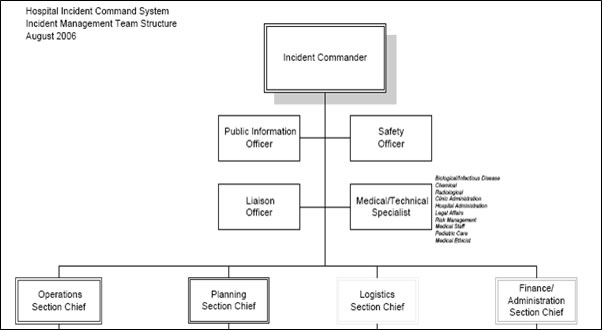
Note: Details of the General Staff positions are given in Figures 4-7.
All ICS positions describe functional considerations that may be needed during a particular event or incident. These positions do not necessarily require that one individual be assigned to each functional role. An individual may be assigned to and perform one or more of these functional roles. The decision about how many functional roles an individual may perform will be based on the magnitude of the event and the performance demands on that person. In the case of small incidents, one person may be able to perform multiple functions. In the case of large events, it is likely that a separate individual will have to be assigned to each specific functional role.
Consistent with the ICS, each staff position should receive a job action sheet (JAS), which is a simple checklist that describes the role, responsibility, and reporting structure of each position within the ICS structure. These forms should be prepared in advance of the incident for rapid distribution to participating staff on their arrival to the ACF. HICS job action sheets that can be downloaded and modified for use in an ACF are available at: http://hicscenter.org/SitePages/HomeNew.aspx. Detailed information and training programs for HICS can be found at the same address.
Command Staff
The Incident Commander is responsible for oversight of the entire response to the incident. This individual will determine the response priorities for the IAP.
The Safety Officer will monitor safety conditions and develop measures for assuring the safety of all team personnel and any ACF patients.
The Incident Commander or Safety Officer may halt operations at any time based on a safety or security risk.
Security is critically important to assure the safety of both staff and patients. The type and number of security personnel will depend on the situation.
The Liaison Officer's role is to serve as the point of contact between the Incident Commander and various agencies and groups assisting in the response. The Liaison Officer's responsibilities include the following:
- Serving as a point of contact for any agency representatives supporting the incident.
- Briefing incoming agencies and answer any questions they may have about the operation.
- Responding to requests from incident personnel for interorganizational contacts.
- Monitoring incident operations for current or potential interorganizational problems.
- Participating in planning meetings to provide the current resource status, limitations, and capabilities of other agency resources.
The Public Information Officer's role is to develop and release information about the incident to the news media, incident personnel, and other appropriate agencies and organizations. The Public Information Officer's responsibilities include the following:
- Advising the Incident Commander on issues related to information sharing and media relations.
- Serving as the primary contact for anyone needing information about the incident and the response.
- Serving the interests of both an external audience (through the media) and an internal audience (incident staff and agency personnel).
- Coordinating with other public information staff to ensure that confusing or conflicting information is not released.
- Obtaining information from the Planning Section, which is responsible for gathering intelligence and other information pertinent to the incident.
- Providing information to the community, the media, and others, and then share that information with the Planning Section Chief and the Incident Commander.
The Medical/Technical Specialist role is dictated by the needs of the specific incident and is meant to provide expert advice to the Incident Commander about issues that require technical expertise. For example, an incident involving a biologic agent might require the involvement of an infectious disease or public health specialist whereas a cyber attack incident would require an information technology expert.
General Staff
The Operations Section (Figure 4) conducts tactical medical operations to carry out the IAP. Activities will include basic medical services, behavioral/mental health support, ancillary medical services and preventive medicine. The Operations Section is responsible for the following:
- Developing and managing the Operations Section to accomplish the incident objectives and strategies set by the Incident Commander;
- Developing and implementing tactics to achieve the incident objectives, including organizing, assigning, and supervising all of the resources assigned to an incident;
- Working closely with other members of the Command and General Staff to coordinate tactical activities;
- Working with the Planning Section Chief and the Safety Officer to develop the Operational Planning Worksheet, and Incident Safety Analysis portions of the IAP; and
- Assuring the health and well-being of the ACF staff and the affected population following a medical crisis.
Figure 4: Operations Section
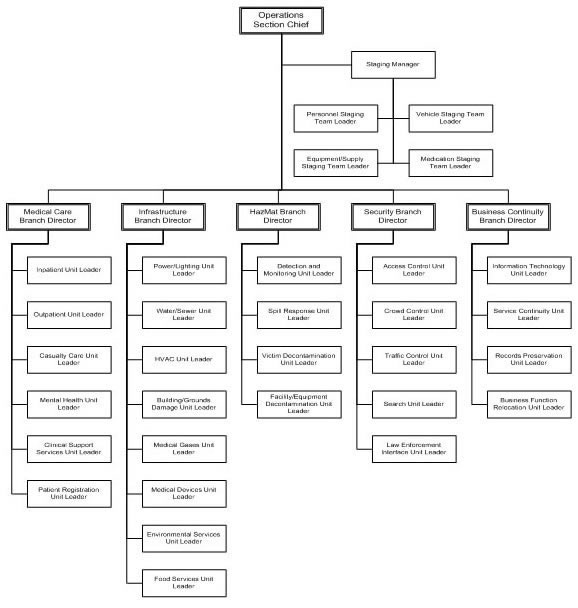
The Operations Section includes the following functional Branches: Staging Manager, Medical Care, Infrastructure, HazMat, Security, and Business Continuity. Each branch may have one or more units activated (as described in the HICS Guidebook, referenced above) based on the nature of the event and the type of ACF. The Medical Care Branch will typically be the focal point of the Operations Section.
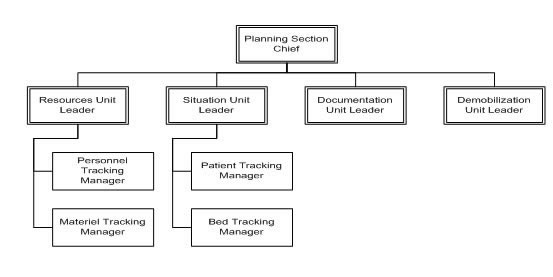
The Planning Section (Figure 5) prepares and documents the IAP by collecting and evaluating information and maintaining resource status and documentation for incident records. The Planning Section is organized according to ICS principles into the following units: Resources, Situation, Documentation, and Demobilization. A full description of this section can be found in the HICS Guidebook.
Figure 5: Planning Section
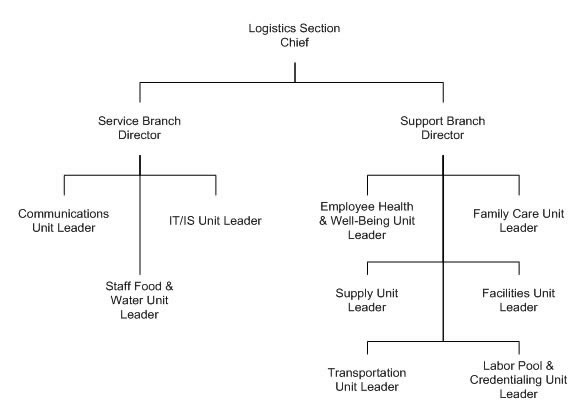
The Logistics Section (Figure 6) provides support, resources, and other services, including personnel, needed to meet operational objectives. The Logistics Section is is organized according to ICS principles and divided into the Service and Support Branches. The Service Branch includes the following units: Communications, Information Technology/Information Services, and Staff Food and Water. The Support Branch includes the following Units: Employee Health and Well-Being, Family Care, Supply, Facilities, Transportation, and Labor Pool and Credentialing. These branches are further described in the HICS Guidebook.
Figure 6: Logistics Section
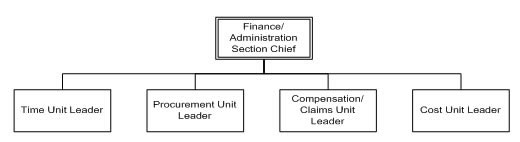
The Finance/Administration Section (Figure 7) provides time recording, procurement, accounting, and cost analysis. Within these units, functions such as team member and patient tracking, award processing and management, medical records management, and other administrative tasks may be carried out. The Finance/Administration Section works in conjunction with the Logistics Section to monitor costs incurred.
Figure 7: Finance Section
ACF Facility Selection
Selection Criteria
Health care agencies and facilities, in coordination with State and local officials, will locate and determine the suitability of an existing facility that can be used to support an ACF, consistent with its intended purpose for specific incidents. Pre-identification of possible ACFs should be included in emergency medical plans. The identified existing structure should be as close as practical to a supporting hospital for ease of transferring patients and sharing resources such as laboratories and diagnostic capabilities. Facilities that may be suitable for use as an ACF include National Guard armories, college campuses, gymnasiums, schools, convention centers, hotel conference rooms, health clubs, community centers, and climate-controlled warehouses.
Infrastructure Requirements:
- Climate controlled enclosed space.
- Perimeter security.
- Waste removal (to include biomedical waste).
- Electrical power source and distribution.
- Potable water.
- Ice.
- Fork lift for off-loading/set-up.
- Local transportation.
- Latrines/showers for staff and patients.
Additional Requirements for Each Facility:
- Communications support.
- Food service for staff and patients.
- Medical oxygen.
- Laundry services.
- Mortuary support.
- Refrigeration.
The Agency for Healthcare Research and Quality (AHRQ) funded an initial site selection tool to assist planners in choosing the most appropriate available structure in which to place an ACF (https://archive.ahrq.gov/research/altsites.htm). This tool has since been updated and revised to reflect experiences of ACF implementation since the original publication and is being published in conjunction with this report.
ACF Operations and Logistics
Decision to Open
The need to open an ACF is normally made as a coordinated decision with health care provider organizations and local and State Government representatives.
The person responsible for making the decision to open an ACF should be identified as part of the planning process. The person may be a hospital administrator or chief executive officer if the ACF is opened by a health care organization, the local or regional public health director, or the designated emergency manager. Once the decision to open an ACF is made, the capabilities and capacity of the ACF must be described. In coordination with hospitals, State and local officials will determine site location, suitability of an existing facility, and the day-to-day operations of the ACF, consistent with its intended purpose for the specific incident.
Supplies and Equipment
The initial supplies and equipment will come from pre-positioned materiel delivered to the ACF from local or State caches or from participating hospitals. A medical resupply system to continue operations for prolonged periods of time must be established.
Generally, all medical and surgical supplies should be stored in a secure, climate-controlled area in close proximity to the patient treatment area.
Most pharmaceuticals are labeled with storage temperatures. The United States Pharmacopeia (USP) defines the various temperatures as:
- Controlled Room Temperatures: 59-86° F or 15-30° C.
- Refrigerator: 36-46° F, or 2-8° C.
- Freezer: 32° F and lower or 0° C and lower.
Pharmaceuticals that are stored at other than USP standard temperatures, are considered to be "adulterated" and therefore unfit for human use.
Communications
Internal Communications. Mechanisms for internal communication between ACF functional areas and associated staff must be determined. In many cases portable two-way radios may be available and used.
External Communications. When normal communications are not disrupted and the ACF facility is equipped with phone service, the primary means of communication will be via existing phone lines. The ACF may also be equipped with portable radios, which augment external communications with ambulance transports and support services and serve as the primary option for backup external communications when normal communications are disrupted. Options for alternate backup communications include satellite phones, Internet connections, and fax machines, along with disconnected or wireless methods of communication such as pagers, Blackberries, personal digital assistants, and cellular telephones. Ideally, a standardized electronic information system is employed at the State, local, or regional level that supports clinical management, patient tracking, and command and control.
Operational Support
The ACF requires the following external support services:
- Refrigeration. Onsite refrigeration should be provided or there should be an adequate electrical supply to handle the demand of temporary refrigeration containers, which can be leased.
- Waste disposal. Waste removal should be available, but if not available during the disaster, planners should have arrangements already in place to haul waste products, including biological hazardous waste, away from the site.
- Laundry. Laundry service needs may be minimized through the use of disposable supplies, except for the blankets, sheets, and pillowcases. Laundry capability should be available at the facility. If laundry support is not available, planners must arrange a contingency contract for this service.
- Food. Planners should arrange for food support.
- Security. Security plans should be in place prior to activation of the ACF.
- Water. Basic daily water support, such as showers, toilets, and sinks, should be available. If water is available for hand washing, basins should be available in every patient care area in readily accessible locations at a ratio of 1 to every 10-25 beds, depending on layout of the facility. Waterless, alcohol-based hand cleaners can also be used in lieu of the basin setup. Although the structure's water supply could be purified by chemical means, bottled water is more convenient and palatable for daily drinking.
- Transportation. Transport for both ambulatory and non-ambulatory patients to and from the associated hospital will be necessary.
- Fuel. Fuel may be needed for external power generation systems.
- Latrines and showers. Latrine and shower availability depends on the specific selection and use of the ACF building.
- Mortuary. The ACF may be required to manage human remains during a catastrophic event.
Security
Physical security of the ACF staff, equipment and the facility is essential. Physical security points include the following:
- Entry and exit points to the area (e.g., the city block), if practicable.
- Access and egress to the building.
- High-risk or high-value areas within the building, such as the temporary morgue and pharmacy.
Patient Management
Based on the predetermined role of the ACF, patients will arrive either by private transportation or by ambulance. A reception area for initial evaluation and registration should be in place and easily accessible for arriving patients.
A medical record system must be planned for and put in place on activation of the ACF. Every patient encounter should be documented using the medical record system planned for the ACF.
Preprinted order sheets and care plans will facilitate the management of patients, consistent with the planned role of the ACF. A system for tracking patient location within the ACF or disposition after completion of treatment at the ACF must be put in place.
Family Management and Support
Consideration for housing patient family members and potentially their pets must be part of the operational plan. Rules and regulations for the operation of the facility ("house rules") must be put into place and include number of visitors, noise management, "lights out," weapons rules, rules about drug or alcohol use.
Staff Management and Support
Ideally, private space for staff should be available to include incident briefing and medical report areas as well as eating, sleeping, toilet, showering, and rest facilities apart from the general patient population.
Demobilization
A strategy for demobilization of the ACF should be developed at the time of mobilization. Criteria for making the determination that the ACF is no longer necessary should be determined in advance.
Facility Operations Template Glossary
Finance/Administration: The Section responsible for all incident costs and financial considerations. Includes the Time Unit, Procurement Unit, Compensation/Claims Unit, and Cost Unit.
Base: The location at which primary logistics functions for an incident are coordinated and administered. There is only one base per incident. (Incident name or other designator will be added to the term base.) The Incident Command Post may be collocated with the base.
Branch: The organizational level having functional or geographic responsibility for major parts of the Operations or Logistics functions. The Branch level is organizationally between Section and Division/Group in the Operations Section and between Section and Units in the Logistics Section. Branches are identified by functional name (e.g., medical, security).
Cache: A pre-determined complement of tools, equipment, and/or supplies stored in a designated location, available for incident use.
Camp: A geographical site, within the general incident area separate from the Incident Base, equipped and staffed to provide sleeping, food, water, and sanitary services to incident personnel.
Chain of Command: A series of management positions in order of authority.
Check-In: The process whereby resources first report to an incident. Check-in locations include: Incident Command Post (Resources Unit), Incident Base, Camps, Staging Areas, Helibases, Helispots, and Division Supervisors (for direct line assignments).
Chief: The ICS title for individuals responsible for functional sections: Operations, Planning, Logistics, and Finance/Administration.
Command: The act of directing and/or controlling resources by virtue of explicit legal, agency, or delegated authority. May also refer to the Incident or Team Commander.
Command Post: See Incident Command Post.
Command Staff: The Command Staff consists of the Public Information Officer, Safety Officer, Liaison Officer, Deputy Incident or Team Commander, and Medical Technical Specialist as needed. They report directly to the Incident or Team Commander. They may have assistants as needed.
Communications Unit: An organizational Unit in the Logistics Section responsible for providing communication services at an incident. A Communications Unit may also be a facility (e.g., a trailer or mobile van) used to provide the major part of an Incident Communications Center.
Delegation of Authority: A statement provided to the Incident Commander by the agency executive delegating authority and assigning responsibility. The Delegation of Authority can include objectives, priorities, expectations, constraints, and other considerations or guidelines as needed. Many agencies require written Delegation of Authority to be given to Incident Commanders prior to their assuming command on larger incidents.
Demobilization Unit: A functional unit within the Planning Section responsible for assuring orderly, safe, and efficient demobilization of incident resources.
Deputy: A fully qualified individual who, in the absence of a superior, could be delegated the authority to manage a functional operation or perform a specific task. In some cases, a Deputy could act as relief for a superior and therefore must be fully qualified in the position. Deputies can be assigned to the Team Commander, General Staff, and Branch Directors.
Director: The ICS title for individuals responsible for supervision of a Branch.
Division: Divisions are used to divide an incident into geographical areas of operation. A Division is located within the ICS organization between the Branch and the Task Force/Strike Team. (See Group.) Divisions are identified by alphabetic characters for horizontal applications and, often, by floor numbers when used in buildings.
Documentation Unit: A functional unit within the Planning Section responsible for collecting, recording, and safeguarding all documents relevant to the incident.
Emergency: Absent a Presidential declared emergency, any incident(s), human-caused or natural, that requires responsive action to protect life or property. Under the Robert T. Stafford Disaster Relief and Emergency Assistance Act, an emergency means any occasion or instance for which, in the determination of the President, Federal assistance is needed to supplement State and local efforts and capabilities to save lives and to protect property and public health and safety, or to lessen or avert the threat of a catastrophe in any part of the United States.
Emergency Operations Centers (EOCs): The physical location at which the coordination of information and resources to support domestic incident management activities normally takes place. An EOC may be a temporary facility or may be located in a more central or permanently established facility, perhaps at a higher level of organization within a jurisdiction. EOCs may be organized by major functional disciplines (e.g., fire, law enforcement, and medical services), by jurisdiction (e.g., Federal, State, regional, county, city, tribal), or some combination thereof.
Emergency Operations Plan (EOP): The plan that each jurisdiction has and maintains for responding to appropriate hazards.
Event: A planned, non-emergency activity. ICS can be used as the management system for a wide range of events (e.g., parades, concerts, or sporting events).
Facilities Unit: A functional unit within the Support Branch of the Logistics Section that provides fixed facilities for the incident. These facilities may include the Incident Base, feeding areas, sleeping areas, and sanitary facilities.
Federal: Of or pertaining to the Federal Government of the United States of America.
Function: Function refers to the five major activities in ICS: Command, Operations, Planning, Logistics, and Finance/Administration. The term function is also used when describing the activity involved (e.g., the planning function). A sixth function, Intelligence, may be established, if required, to meet incident management needs.
General Staff: A group of incident management personnel organized according to function and reporting to the Incident Commander. The General Staff normally consists of the Operations Section Chief, Planning Section Chief, Logistics Section Chief, and Finance/Administration Section Chief.
Ground Support Unit: A functional unit within the Support Branch of the Logistics Section responsible for the fueling, maintaining, and repairing of vehicles and the transportation of personnel and supplies.
Group: Groups are established to divide the incident into functional areas of operation. Groups are composed of resources assembled to perform a special function not necessarily within a single geographic division. (See Division.) Groups are located between Branches (when activated) and Resources in the Operations Section.
Incident: An occurrence or event, natural or human-caused, that requires an emergency response to protect life or property. Incidents can, for example, include major disasters, emergencies, terrorist attacks, terrorist threats, wildland and urban fires, floods, hazardous materials spills, nuclear accidents, aircraft accidents, earthquakes, hurricanes, tornadoes, tropical storms, war-related disasters, public health and medical emergencies, and other occurrences requiring an emergency response.
Incident Action Plan (IAP): An oral or written plan containing general objectives reflecting the overall strategy for managing an incident. It may include the identification of operational resources and assignments. It may also include attachments that provide direction and important information for management of the incident during one or more operational periods.
Incident Base: Location at the incident where the primary Logistics functions are coordinated and administered. (Incident name or other designator will be added to the term Base.) The Incident Command Post may be collocated with the Base. There is only one Base per incident.
Incident Commander (IC): The individual responsible for all incident activities, including the development of strategies and tactics and ordering and the release of resources. The IC has overall authority and responsibility for conducting incident operations and is responsible for the management of all incident operations at the incident site.
Incident Command Post (ICP): The field location at which the primary tactical-level, on-scene incident command functions are performed. The ICP may be collocated with the incident base or other incident facilities and is normally identified by a green rotating or flashing light.
Incident Command System (ICS): A standardized on-scene emergency management construct specifically designed to provide for the adoption of an integrated organizational structure that reflects the complexity and demands of single or multiple incidents, without being hindered by jurisdictional boundaries. ICS is the combination of facilities, equipment, personnel, procedures, and communications operating within a common organizational structure, designed to aid in the management of resources during incidents. It is used for all kinds of emergencies and is applicable to small as well as large and complex incidents. ICS is used by various jurisdictions and functional agencies, both public and private, to organize field-level incident management operations.
Incident Objectives: Statements of guidance and direction necessary for the selection of appropriate strategy(ies) and tactical direction of resources. Incident objectives are based on realistic expectations of what can be accomplished when all allocated resources have been effectively deployed. Incident objectives must be achievable and measurable, yet flexible enough to allow for strategic and tactical alternatives.
Intelligence Officer: The Intelligence Officer is responsible for managing internal information, intelligence, and operational security requirements supporting incident management activities. These may include information security and operational security activities, as well as the complex task of ensuring that sensitive information of all types (e.g., classified information, law enforcement sensitive information, proprietary information, or export-controlled information) is handled in a way that not only safeguards the information, but also ensures that it gets to those who need access to it to perform their missions effectively and safely.
Liaison Officer: A member of the Command Staff responsible for coordinating with representatives from cooperating and assisting agencies. The Liaison Officer may have assistants.
Logistics: Providing resources and other services to support incident management.
Logistics Section: The Section responsible for providing facilities, services, and materials for the incident.
Mitigation: The activities designed to reduce or eliminate risks to people or property or to lessen the actual or potential effects or consequences of an incident. Mitigation measures may be implemented prior to, during, or after an incident. Mitigation measures are often informed by lessons learned from prior incidents. Mitigation involves ongoing actions to reduce exposure to, probability of, or potential loss from hazards. Measures may include zoning and building codes, floodplain buyouts, and analysis of hazard- related data to determine where it is safe to build or locate temporary facilities. Mitigation can include efforts to educate governments, businesses, and the public on measures they can take to reduce loss and injury.
Mobilization: The process and procedures used by all organizations (Federal, State, and local) for activating, assembling, and transporting all resources that have been requested to respond to or support an incident.
Mobilization Center: An off-incident location at which emergency service personnel and equipment are temporarily located pending assignment, release, or reassignment.
National Incident Management System (NIMS): A system mandated by HSPD-5 that provides a consistent nationwide approach for Federal, State, local, and tribal governments; the private sector; and nongovernmental organizations to work effectively and efficiently together to prepare for, respond to, and recover from domestic incidents, regardless of cause, size, or complexity. To provide for interoperability and compatibility among Federal, State, local, and tribal capabilities, the NIMS includes a core set of concepts, principles, and terminology. HSPD-5 identifies these as the ICS; multi-agency coordination systems; training; identification and management of resources (including systems for classifying types of resources); qualification and certification; and the collection, tracking, and reporting of incident information and incident resources.
National Response Framework: A plan mandated by HSPD-5 that integrates Federal domestic prevention, preparedness, response, and recovery plans into one all-discipline, all-hazards plan.
Officer: The ICS title for the personnel responsible for the Command Staff positions of Safety, Liaison, and Public Information.
Operations Section: The section responsible for all tactical operations at the incident. Includes Medical Care, Infrastructure, HazMat, Security and Business Continuity Branches as well as Staging Area, Task Forces, Strike Teams and Single Resources.
Planning Section: Responsible for the collection, evaluation, and dissemination of information related to the incident, and for the preparation and documentation of the Incident Action Plan. The section also maintains information on the current and forecasted situation and on the status of resources assigned to the incident. Includes the Resources, Situation, Documentation, and Demobilization Units.
Procurement Unit: functional unit within the Finance/Administration Section responsible for financial matters involving vendor contracts.
Public Information Officer: A member of the Command Staff responsible for interfacing with the public and media or with other agencies with incident-related information requirements.
Resources Unit: A functional unit within the Planning Section responsible for recording the status of resources committed to the incident. The Unit also evaluates resources currently committed to the incident, the impact that additional responding resources will have on the incident, and anticipated resource needs.
Safety Officer: A member of the Command Staff responsible for monitoring and assessing safety hazards or unsafe situations and for developing measures for ensuring personnel safety. The Safety Officer may have assistants.
Section: The organizational level having responsibility for a major functional area of incident management, such as Operations, Planning, Logistics, Finance/Administration, and Intelligence (if established). The Section is organizationally situated between the Branch and the Incident Command.
Service Branch: A Branch within the Logistics Section responsible for service activities at the incident. Includes the Communications, Information Technology/Information Services and Staff Food and Water Units.
Situation Unit: A functional unit within the Planning Section responsible for the collection, organization, and analysis of incident status information and for analysis of the situation as it progresses. Includes the Patient Tracking and Bed Tracking Managers and reports to the Planning Section Chief.
Staff Food and Water Unit: A functional unit within the Service Branch of the Logistics Section responsible for providing meals for incident personnel.
Staging Area: Location established where resources can be placed while awaiting a tactical assignment. The Operations Section manages Staging Areas.
Supply Unit: A functional unit within the Support Branch of the Logistics Section responsible for ordering equipment and supplies required for incident operations.
Support Branch: A Branch within the Logistics Section responsible for providing personnel, equipment, and supplies to support incident operations. Includes the Employee Health and Well-Being, Family Care, Supply, Facilities, Transportation, and Labor Pool and Credentialing Units.
Technical Specialists: Personnel with special skills that can be used anywhere within the ICS organization.
Unit: The organizational element having functional responsibility for a specific incident Operations, Planning, Logistics, or Finance/Administration activity.
Staffing Recommendations
Staffing an ACF is key to its successful operation and may be one of the largest challenges, depending on the nature of the incident. A review of the literature reveals that relatively few proposals have been put forth for staffing an ACF. One important work that has been used as the basis for some surge capacity plans is the Modular Emergency Medical System (MEMS) and two of its components, the Acute Care Center (ACC) and the Neighborhood Emergency Help Center (NEHC).1 MEMS was developed by the U.S. Army Soldier and Biological Chemical Command (SBCCOM) to create a concept of operations for a medical response package that could be created to increase the capacity of States and municipalities to handle a large influx of patients after a biological attack.
While MEMS was originally created to respond to bioterrorism, its principles can be applied to a variety of mass casualty scenarios. The key aspects of MEMS are:
- Integrates all local medical aspects.
- Allows a flexible and timely response through its modular design.
- Serves as a framework to support a massive medical response.
- Augments the existing medical system.
- Is consistent with the Incident Command System.
The ability to develop and deploy these two expandable patient care modules is the foundation of MEMS. Both modules have application to the current concept of an ACF. The NEHC is designed to serve as a primary triage and evaluation facility capable of screening up to 1000 patients per day. At the NEHC, patients who are potentially exposed to an infectious agent can be screened and prophylactically treated and/or immunized. At the same time, information regarding the incident can be disseminated. The NEHC has limited treatment and holding facilities, so symptomatic patients would be directed to an appropriate health care facility or ACC. The NEHC staffing protocol calls for the following level of staffing:
| Position | Number |
|---|---|
| Facility Manager | 1 |
| Medical Section Operations Chief | 1 |
| Records/Planning Section Chief | 1 |
| Logistics Section Chief | 1 |
| Transportation Officer | 1 |
| Communications Officer | 1 |
| Maintenance Officer | 1 |
| Physician | 3 |
| Physician Assistant (PA) | 1 |
| Family Nurse Practitioner (NP) | 1 |
| Nurse | 7 |
| Paramedics | 3 |
| EMT | 6 |
| Clerks | 14 |
| Security Personnel | 4 |
| Housekeeping Personnel | 2 |
| Volunteers | 32 |
| TOTAL | 80 |
The ACC on the other hand is a true ACF that has both treatment and patient holding capability. It is built around 50-bed subunits with staffing recommendations for the appropriate number of health care providers per subunit. The ACC model suggests the following staffing for a 12-hour shift per 50-bed subunit.
| Position | Number |
|---|---|
| Physician | 1 |
| Physician Assistant (PA) or Nurse Practitioner (NP) | 1 |
| Registered nurses (RN) and/or Licensed Practical Nurses (LPN) | 6 |
| Nursing Assistants and/or Nursing Support Technicians | 4 |
| Medical Clerks (Unit Secretaries) | 2 |
| Respiratory Therapist | 1 |
| Case Manager | 1 |
| Social Worker | 1 |
| Housekeeping Personnel | 2 |
| Patient Transporters | 2 |
| TOTAL | 21 |
It should be remembered, however, that the ACC was, and is, a theoretical proposal that was originally designed to respond to a biological threat but has never actually been implemented. It is not unreasonable to assume, however, that it would also have applicability to other mass casualty situations. It is also interesting to note the omission of pharmacists from both the NEHC and ACC staffing guidelines, a staffing group that has proven to be invaluable in actual operation of ACFs.
Incorporating Real World Experience
After Hurricanes Katrina and Rita struck the Gulf Coast of the United States in the fall of 2005, both the health care system and municipal infrastructure of New Orleans and adjacent coastal areas were nearly destroyed, leaving thousands of people homeless with many requiring medical care. The medical care they needed was no longer available at local health care facilities that had been incapacitated by the storms. What followed was the largest disaster response operation in American history to date. Large shelters were set up in Louisiana and surrounding States for the evacuees and numerous ACFs were created to replace the collapsed health care system. This tragic event has served as a valuable learning opportunity to study how ACFs should operate.
ACF Staffing: The Katrina and Rita Experience
Table 1 compares data points on ACF staffing as reported from eight different ACFs that operated after Hurricanes Katrina and Rita in 2005. The first three rows describe the structure and function of each ACF. The following rows show the duration of operations and give available patient census numbers. Due to the difficulty of recordkeeping in a disaster, the numbers are estimates. Also, the daily patient load varied significantly. Most patients arrived in the early days of the operation and then the numbers of patients gradually tapered off leading to decommissioning of the ACF. Respondents were not able to provide exact daily patient census numbers that would allow for a precise statistical analysis of patient volumes and staffing requirements. Instead, the total number of patients seen is documented. In some cases a daily average and peak census were given.
The remaining rows document how many of each type of health care provider were on duty at a given time. Again, there was a great deal of flux in the post-disaster environment with day-to-day variability of the exact number of providers. The respondents were asked to give a number that represents an average of how many of each type of provider were present on any given day of the ACF operation.
Table 1: Hurricanes Katrina and Rita 2005 ACF Staffing Matrix
| Site 1 | Site 2 | Site 3 | Site 4 | Site 5 | Site 6 | Site 7 | |
|---|---|---|---|---|---|---|---|
| Function | Pediatric shelter support | General shelter support | Ambulatory and inpatient health care replacement | Ambulatory health care replacement | Ambulatory and surgical health care replacement | Special- needs in-patient care | Ambulatory health care replacement |
| Structure | Fixed facility | Fixed facility | Fixed facility | Fixed facility | Mobile | Fixed facility | Fixed facility |
| Inpatient Capability | Y | N | Y | N | Y | Y | N |
| Days of Operation | 13 | 16 | NDA | NDA | 10 | NDA | NDA |
| Total Patients | >3,500 | >10,000 | >6,000 | >20,000 | 7400 | 200 | 400 |
| Daily Average Census | NDA | 619 (+/- 301) | NDA | NDA | 25-300 | NDA | NDA |
| Peak Daily Census | 400 | 1,125 | NDA | NDA | 500 | NDA | NDA |
| Shift Length (hours) | 8, 12, or 24 | 4,8, or 12 | 8 for most, 12 for nurse managers | 12 | 12 | 12 | NDA |
| Day/Night Staffing Difference | Y | Y | Y | N | Y | Y | NDA |
| Total Staff | NDA | 7 common staff / 1000 volunteers | "several hundred" | 50 | 60-100 | 100 | 300 at various times; daily total not listed |
| Physicians | 6 | 16 AM /4 PM | 25 | NDA | 11 | 4 | 7 |
| Midlevel Providers (PA/NP) | Present but number not recorded | N | 20 | NDA | 1-2 | 5 | 3 |
| Nurses | 5 | 20 | 50+ | NDA | 8-10 | 20 | 10 |
| LPN/EMT | N | N | 50+ | NDA | 8-10 | NDA | 1-2 |
| Pharmacists | 1 | 2/1 | 6+ | 2-3 | 2-3 | 2 | 1-2 |
| Clerks/Administrative | 1 | 5 AM /1 PM | 50+ | 1-2 | 1-2 | NDA | 6 |
Y=yes or present but number unknown
N=no
NDA = No Data Available
Fields that have two numbers listed in a "x/y" format indicate a difference in staffing between day & night Due to difficulties with record keeping and in light of day-to-day variations in staffing, all numbers should be viewed as estimates
Table 2 provides a look at the ratio of patients to providers at each site. Only Sites 1, 2, and 5 indicated how many days their site was operational. Without that data point as the denominator for all sites, the total number of patients seen per day is difficult to determine. As all surveyed sites were responding to the same overall event, the average of the number of days of operations of Sites 1, 2, and 5 (13 days) was arbitrarily applied to Sites 3,4,6,7, and 8 (grayed columns). The total number of patients was then divided by the actual or calculated number of days of operation to yield the number of patients seen per day. As previously noted, the daily census varied greatly depending on the number of days after the event.
Table 2: Ratios of Health Care Providers to Patients on a Daily Basis
| Site 1 | Site 2 | Site 3 | Site 4 | Site 5 | Site 6 | Site 7 | |
|---|---|---|---|---|---|---|---|
| Function | Pediatric shelter support | General shelter support | Ambulatory and inpatient health care replacement | Ambulatory health care replacement | Ambulatory and surgical health care replacement | Special needs inpatient care | Ambulatory health care replacement |
| Structure | Fixed facility | Fixed facility | Fixed facility | Fixed facility | Mobile | Fixed facility | Fixed facility |
| Days of Operation | 13 | 16 | 13* | 13* | 10 | 13* | 13* |
| Total Patients | 3,500 | 10,000 | 6,000 | 20,000 | 7400 | 200 | 400 |
| Daily Average Census | 269* | 625* | 462* | 1538* | 740* | 15* | 31* |
| Numbers below reflect the ratio of a given category of provider to the number of patients seen on an average day | |||||||
| Physicians | 1:45 | 1:39 | 1:18 | NDA | 1:67 | 1:4 | 1:4 |
| Midlevel Providers (PA/NP) | NDA | NP | 1:23 | NDA | 1:493 | 1:3 | 1:10 |
| Nurses | 1:54 | 1:31 | 1:9 | NDA | 1:82 | 1:1 | 1:3 |
| LPN/EMT | NP | NP | 1:9 | NDA | 1:82 | NDA | 1:16 |
| Pharmacists | 1:269 | 1:313 | 1:77 | 1:513 | 1:246 | 1:8 | 1:16 |
| Clerks/Administrative | 1:269 | 1:125 | 1:9 | 1:1025 | 1:493 | NDA | 1:5 |
NP = Type of provider Not Present
NDA = No Data Available
* Estimated; see text for details.
The daily census was divided by the number of each type of provider to find the ratio of each type of provider to patients seen per day. For example, Site 1 had a calculated daily average patient census of 269 and had an average of 6 physicians on duty per day, so the ratio of physicians to patients is 1:45. As these final ratios are based on several averages and assumptions, they should be taken only as first order approximations.
The final issue to consider when examining this data presented is that the ratios are simply the ratios that existed in each ACF. The data does not indicate that they are the correct ratios. None of the respondents reported being limited by the number of available personnel. There were also no comments in our questionnaire about adverse patient outcomes because of health care provider shortages. That being said, however, the survey instrument did not specifically ask respondents to suggest an ideal staffing ratio, nor did it specifically ask how their staffing ratio differed from what they thought would be ideal.
It is interesting to note, however, that the overall numbers of physicians and nurses (registered nurses and licensed practical nurses) are, in fact, very similar to the recommendations made in the MEMS documents. Thus, a suggested staffing consideration of one physician and six nurses for a 50-bed patient unit may represent a reasonable starting point for an ACF. These numbers can then be increased or decreased depending on the nature of the event and the specific role to be performed by the ACF.
ACF Credentialing
Table 3 summarizes some credentialing issues that had to be addressed by the various sites. One of the themes that emerged was that credentialing was somewhat easier if the responders were part of a previously established disaster response team under the control of either the Federal Government or a State government. A review of the medical literature (see references section) shows that many responders were part of Federal disaster response teams such as Disaster Medical Assistance Teams and Urban Search and Rescue teams, State disaster response teams such as the Illinois Medical Response Team, or military units. These types of teams have an advantage in that they have already gone through a credentialing process, have a government-issued identification card, and work together within a predefined command structure. Some of the other facilities involved in the response were operated under the auspices of local health care institutions and/or county health agencies. Those providers who were already credentialed by the sponsoring institution were easy to verify but these facilities had greater difficulty with incorporating volunteer providers from outside of the sponsoring system. Several respondents commented on the need for an improved system for credentialing providers ahead of time or credentialing them rapidly and efficiently after an event.
Table 3: Hurricane Katrina and Rita 2005 Alternate Care Facility Credentialing Matrix
| Site 1 | Site 2 | Site 3 | Site 4 | Site 5 | Site 6 | Site 7 | |
|---|---|---|---|---|---|---|---|
| Method of credentials verification for health professionals | County Health Department Oversight | Inspection of identification badge from home institution. | Handled by U.S. Public Health Service | >90% were Federal so came credentialed. | Credentialed through sponsoring health care system. | All Federal employees; arrived credentialed. | Credentials not verified due to rapid need for response. |
| Were identification cards created? | Sponsoring hospital ID cards used. Others tried for outside staff with little success | Yes, with a make-shift badge maker | Special wrist bands provided by local University. | No; most had Federal identification cards. | Home State office of EMS ID cards. | Federal ID card. | N |
| If so, was a commercially available product used? | NA | NA | NA | NA | NA | NA | NA |
| Suggested future changes in the credentialing process? | Early credentialing; ideally prior to the event | N | N | NA | N | Develop a standardized credentialing system. | NA |
| Did anyone impersonate a provider to gain access? | One individual tried to impersonate a physician. | N | Impersonator from the media to gain access. No one falsified credentials to provide care. | N | N | N | N |
| Steps taken at the State level to facilitate out-of-state providers? | State allowed instant licensure with sponsorship of the primary hospital. | State was not involved. | NA | NA | EMAC | NA | EMAC |
| Were providers from different health care systems working side by side? | Y | Y | Y | Y | Y | Y | Y |
| If so, did this create any command and control(C2) issues? | No significant issues. Sponsoring hospital retained control. | N | No, too busy to have any turf battles. | No; used clear command system. | N | Minor issues while establishing C2 system. | N |
| Were there any challenges dealing with out-of-state licensing issues? | Y | N | No, handled through U.S. Public Health Service. | Difficulty writing prescriptions for controlled substances. | Y | Y | N |
Y=Yes or present but number unknown; N=No; NA=Not Applicable; U=Unknown; no data available.
One system that has been developed is the Emergency Systems for Advance Registration of Volunteer Health Professionals (ESAR-VHP).2 This program is currently administered by the Office of the Assistant Secretary for Preparedness and Response (ASPR) in the U.S. Department of Health and Human Services (HHS). The goal is to create an electronic database of health care providers who are willing to volunteer to serve after a disaster. The system is designed to be administered separately in each State. Its goals are to:
- Register health volunteers.
- Apply emergency credentialing standards to registered volunteers.
- Allow for the verification of the identification of the identity, credentials, and qualifications of registered volunteers in an emergency.
None of the survey respondents reported any significant contribution of the ESAR-VHP system to credentialing at their respective ACFs, possibly because the system was still in its early stages of State-based development. Several respondents did report that a system like ESAR-VHP could be valuable if it could be further developed and effectively implemented
Another resource that assisted with incorporating out-of-Sate health care providers into the local response was the Emergency Management Assistance Compact (EMAC) (Public Law 104-321).3 All personnel who respond to an event as part of a State's formal response to another State's formal request for aid theoretically are covered under the EMAC. Congress ratified EMAC in 1996 to allow more expeditious response of emergency medical resources and National Guard units from other States to the site of a disaster. EMAC gives four privileges and protections to responders. First, it promises that responders' licenses or certificates from their home State will be honored in the State to which that person is responding. However, the person must be part of the official response element; freelancers are not protected. Second, responders are likely to receive protection from malpractice claims that may arise from their service in the affected area. Third, responders are promised death and disability benefits, although this applies more to civilian responders. Finally, in theory, States that respond through EMAC should be reimbursed for any expenses they incur during response operations.
The sudden nature of the two hurricanes that struck the Gulf Coast in 2005 and the overwhelming number of displaced persons after New Orleans flooded necessitated a very rapid medical response and allowed little time for many ACFs to establish credentialing systems. There were reports of people impersonating health care providers to gain access to facilities. The impersonation cases in our survey represent members of the media or other individuals who wanted to gain access in order to "see what's going on." However, the medical literature reports a woman falsifying her credentials to a National Guard medical unit operating in St. Bernard Parish in order to gain access to the Parish. She did not provide any direct patient care but did manage to insert herself into several high-level planning meetings and even shook hands with President Bush when he met with medical providers in the Parish.3 Clearly, credentialing during disasters can be somewhat difficult; however, it is also critical in order to avoid patients being harmed by imposters.
Section References:
- The Concept of Operations for the MEMS, ACC, and NECC are available on the Northern New England Metropolitan Medical Response System Web site at: http://nnemmrs.org
- Information on the Emergency Systems for Advance Registration of Volunteer Health Professionals is available at: http://www.disasterpreparation.net/resources-hrsa.html
- Information on the Emergency Management Assistance Compact is available at: https://emilms.fema.gov/IS200b/ICS0103260text.htm
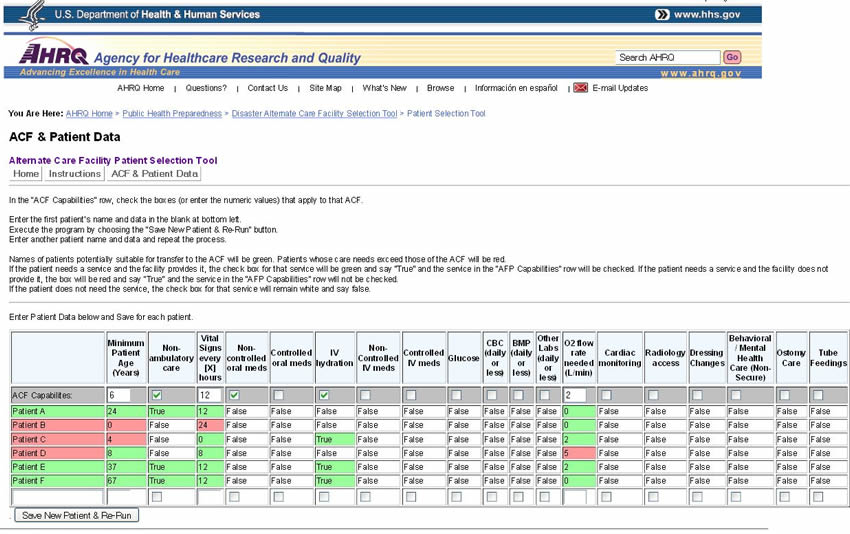
Patient Selection Tool
As mentioned previously, one potential use of an ACF is for off-loading from hospitals less ill hospital patients who are not yet ready for early discharge from the hospital. The challenge, however, is how to quickly determine which inpatients are eligible for transfer to a designated ACF. To assist in the decision process, a Patient Selection Tool was developed (Figure 8). The Patient Selection Tool may be used manually by printing out copies of the tool. Detailed user instructions are included with the tool.
Figure 8. Patient Selection Tool With Sample Data Entered
Equipment and Supply Options
Providing an ACF with the necessary equipment and supplies requires significant advance planning. In most situations, supplies will not be available in large quantities from nearby health care institutions or from normal supply chains. Therefore, supplies must be "cached" in advance for use at the time of the establishment of an ACF. Different levels of supply support have been proposed and implemented.1,2 The following three levels of supply caches are based on their robustness (excluding pharmaceuticals because of their special storage requirements).
Level I: Hospital Augmentation/Limited ACF Cache—approximately $20,000 (Table 4)
Table 4 is a list of supplies that represents a most basic unit of supply support for increased surge capacity of 50 patients, consisting only of items that have very extended shelf life, such as: cots, linens, masks, gowns, gloves, and IV poles. No pharmaceuticals are included. This material is packed in a trailer for mobility. This cache could be used as additional stocking for an existing hospital (i.e. to set up a medical ward in a cafeteria, using other items as necessary from the hospital) or could offer supplies for a limited level care at an ACF.
Table 4. Level I: Hospital Augmentation/Limited ACF Cache (50 Patients)
| Item | Number | Cost Each Item | Total |
|---|---|---|---|
| Disaster/surge capacity trailer | 1 | 10,000 | 10,000 |
| Patient cots | 45 | 50 | 2250 |
| Patient cots, with wheels, collapsible | 10 | 250 | 2500 |
| Linens - Sheets (2 per patient + extras) | 150 | 4.56 | 684 |
| Linens - Blankets | 75 | 13.5 | 1012.50 |
| Linens - Pillows (disposable - case of 15) | 4 | 43.2 | 172.80 |
| Linens - Pillow cases | 100 | 1.14 | 114 |
| N95 masks (case of 210) | 1 | 98 | 98 |
| Gloves - Latex Free Exam - small (case of 1000) | 1 | 36 | 36 |
| Gloves - Latex Free Exam - medium (case of 1000) | 1 | 36 | 36 |
| Gloves - Latex Free Exam - large (case of 1000 | 1 | 38.34 | 38.34 |
| Gloves - Powder Free Exam - small (case of 1000) | 1 | 37.55 | 37.55 |
| Gloves - Powder Free Exam - medium (case of 1000) | 1 | 37.55 | 37.55 |
| Gloves - Powder Free Exam - large (case of 1000) | 1 | 39 | 39 |
| Gowns ( for staff - splash resistant - case of 12) | 10 | 39 | 390 |
| Bag-valve-mask respirators | 10 | 11 | 110 |
| Blood pressure cuffs (manual) | 5 | 40 | 200 |
| Stethoscopes | 10 | 35 | 350 |
| IV Poles | 25 | 60 | 1500 |
| TOTAL EQUIPMENT COSTS | $19,605.74 | ||
Level II: Regional ACF Cache—approximately $100,000 (Table 5)
Table 5 represents a more complete list of material to supply a regional ACF for 500 patients. This implementation of the cache, or medical armory, concept was developed by the Colorado Department of Public Health and Environment and approved by its Hospital Preparedness Advisory Committee. The approximate price for a single cache for 500 patients is less than $100,000. Note that, as with the Level I cache, pharmaceuticals are excluded and only items with extremely long shelf life are included.
Table 5. Level II Regional ACF Cache (500 Patients)
| Product Namea, b | Descriptionc |
|---|---|
| Applicator, cotton tipped | sterile, cotton-tipped, wood shaft; 5 yr shelf life |
| Bag Holder | rectangular aluminum |
| Bag Valve-Mask (adult) | Disposable |
| Bag Valve-Mask (infant) | Disposable |
| Bag, Disposable | Plastic, drawstring, 33 gal. |
| Bag, Disposable, Biohazard | disposable, 2 ml, red, 33 gallon |
| Batteries, AA | for flashlights |
| Bedpan | pontoon type, plastic |
| Bedpan, Fracture | Plastic, female, mauve |
| Blanket, Flannel | |
| Blanket, infant | white, cotton |
| Blanket, thermal | WHI2.2 lb 48 |
| Blood Pressure Unit | Aneroid, Adult, L/F |
| Blood Pressure Unit | Aneroid, Child, L/F |
| Brief, Adult | Trimline, Medium, 8/12'sF |
| Bungy Cords | 20 piece assortment |
| Chair, Folding | Poly |
| Clip Boards | brown clipboard |
| Cots, Portable | Collapsible deluxe aluminum military cot |
| Cots, Portable 500 lb rated | 600 Denier nylon PVC-back poly on aluminum frame |
| Crib, Peds, Portable | single drop rail |
| Diapers, disposable | Baby, Cloth-Like CVR |
| Disinfectants/detergent | Meritz Plus, 32 oz. |
| Emesis Basin | |
| Form, General Medicine | |
| Form, Laboratory, Diagnostic | |
| Form, Registration, English | |
| Form, Registration, Spanish | |
| Gate, Child | Superyard XT Gate by Northgate Industries |
| Gloves | Medium, powder free, chloroprene |
| Gloves | Large, powder free, chloroprene |
| Gown, Patient, disposable | Adult, tissue/poly-tissue, blue; 2 yr shelf life |
| Gown, Patient, disposable | Pediatric, poly, white |
| Gown, Provider | MEDIUM, DuPont ProVent, Open back |
| Gown, Provider | LARGE, DuPont ProVent, Open back |
| Hamper Bag | drawcord, p/c natural |
| Hamper, Linen (soiled) | Rectangular stnd w/o lid |
| Hand Cleaner (waterless) | Epi-Clenz, 4 oz 70% ethyl |
| ID Band, Insert | Adult, vinyl, Blue |
| ID Band, pediatric | vinyl, snap, pink |
| IV Set | 15DR/ML, LL,NO |
| Light, Flashlight | VersaBrite II, 8000 cp |
| Light, Headlamp | Trident halogen w/cloth strap |
| Mask, N-95 particulate respirators | Resp, 8211 N95, Cool Flw |
| Mask, Oxygen, Adult | Medium concent w/7' |
| Mask, Oxygen, Pediatric | Medium concen, 7'TB |
| Mat, Child | Mahar flat rest mat/2" foam (10 yr warranty) |
| Mattress, Portable Crib | Kolcraft, 2.5" thick, nonallergenic |
| Mattress Underpad, Crib | Polymer, Deluxe |
| Name Badge & Holder, plastic clip-on | inkjet/laserjet, 100/box |
| Notepads | White, 100 pages |
| Pack, Ice | Cold Compress |
| Pack, Warm | Solar-Pack |
| Penlight, disposable | 6 /pk |
| Pens, Standard | Bic Clic Stick |
| Pillowcase, disposable | Tissue/Poly, White |
| Pillows, disposable | Protect a Med Cot Pillow, blue |
| Pole, IV | 4 caster, 2 hook |
| Scissors, Lister bandage | 5 1/2" |
| Screen, Privacy, 3-panel | folding, w/casters, flame retardant |
| Sharps Containers, Biohazard | 2 gal. Red |
| Sheets, Stretcher | Tissue/Poly, Blue |
| Soap, Liquid | Protection Plus Antimicrobial |
| Spectacles, Eye Protective | clear, wraparound, poly |
| Stethoscope, dual head | black, 5 yr shelf life |
| Storage container | clear plastic, attached top |
| Stretcher, Folding | Ferno Model 12 |
| Stretcher, w/Wheels | Ferno Model 11 |
| Table, Folding | Gray |
| Tape, Cloth | Cloth |
| Tape, Duct | |
| Thermometer, Disposable Strips | Nextemp 1 use thermometer; 5 yr shelf life |
| Tongue depressor | |
| Tourniquet | latex free |
| Urinal, male | w/Hill-Rom Compatible Handle |
a The inclusion of product brand names is for identification and illustrative purposes only and does not imply any type of endorsement or specific recommendation.
b Quantities must take into consideration both the length of time the site will be in use (before re-supply can occur) and the purpose of the site.
c For storage purposes, calculate the overall space needed based on the size of boxes or containers the items will be stored in.
Level III: Comprehensive ACF Cache—no cost estimate currently available (Tables 6-9)
Tables 6-9 provide comprehensive lists of equipment and consumables that were adapted from work done by the U.S. military and published in The Concept of Operations for the Acute Care Center by the U.S. Army Soldier and Biological Chemical Command (SBCCOM).3 These lists represent a specification for a completely supplied 50-bed ACF consisting of items with both long and short shelf-life. This represents a more complete level of cache than levels 1 and 2. The initial specifications also included pharmaceuticals, but they are not included here as separate national, regional and local planning efforts are addressing this issue.
This extensive list has been separated into: Equipment Considerations, Patient Care Related Consumables, Administrative Consumables and Oxygen and Respiratory-Related Equipment Considerations (Tables 6-9). Note that this equipment and the consumables can be pre-acquired and stored in a "medical cache" as well. Consumable items may represent one of the greatest challenges for establishing an ACF due to the number and quantity of items. This comprehensive list also includes oxygen and respiratory-related supplies that should be considered for providing limited respiratory support.
Table 6. Equipment Considerations for Level III Comprehensive ACF Medical Cache (50 Bed Unit)
| Equipment | Infectious | Non-Infectious | Quarantine |
|---|---|---|---|
| Beds/Cots (with extra) | 52 | 52 | 52 |
| Chairs correlation with staffing level | 12 | 12 | 4 |
| Desks correlation with staffing level | 6 | 6 | 2 |
| Fax Machine | 1 | 1 | ? |
| Housekeeping Cart with supplies | 1 | 1 | 1 |
| Internet email Access | 1 | 1 | 1 |
| IV Poles | 50 | 50 | 0 |
| Linens (sheets/pillows/pillow cases/hand towels/ bath towels) | 100 | 100 | 100 |
| Patient Commodes | 4 | 4 | 1 |
| Pharmacy Carts | 2 | 2 | 1 |
| Privacy Dividers | 25 | 25 | 25 |
| Refrigerators (food/meds) | 3 | 3 | 1 |
| Stretchers | 2 | 2 | 0 |
| Supply Carts | 3 | 3 | 1 |
| Telephones | 5 | 5 | 5 |
| Treatment Carts | 2 | 2 | 0 |
| Washing Machine | 1 | 1 | 1 |
| Wheelchairs | 2 | 2 | 1 |
Table 7. Patient Care-Related Consumables for Level III Comprehensive ACF Medical Cache (50 Bed Unit)
| Item Description | Calculations of Quantities | Total Item Count | Unit of Issue | Total UoIs Required |
|---|---|---|---|---|
| Alcohol pads (multiple widespread use) | 2-4 Boxes per 24 hours | 14-28 | Box | 1 Box |
| Catheters, intraosseous module blue (pediatric use) | May use 1/day max. | 6-7/wk of 1 standard size | Each | 7 Each |
| Intermittent IV access device (lock) | 50 pts initially (first day) then 10% | 250/wk | 50/Box | 5 Boxes |
| IV catheters, 18g with protectocath guard | 40% of pts req IVs | 150/wk | 50/Box | 3 Boxes |
| IV catheters, 20g with protectocath guard | 40% of pts req IVs | 150/wk | 50/Box | 3 Boxes |
| IV catheters, 22g with protectocath guard | 10% of pts req IVs | 25/wk | 50/Box | 0.5 Boxes |
| IV catheters, 24g with protectocath guard | 10% of pts req | 25/wk | 50/Box | 0.5 Boxes |
| IV fluid bags, NS, 1000cc (required by 60% of patients) | (50% of pts(25)/day x 3L/pt)x | 315 L/wk | 12/Case | 18 Cases |
| IV fluid bags, D5 1/2NS, 1000cc (required by 40% of patients)l | (50% of pts(25)/day x 3L/9t)x | 210 L/wk | 12/Case | 18 Cases |
| IV start kits | Same # as intermittent access device | 60 | 25/Box | 2.5 Boxes |
| IV tubing w/ Buretrol drip set for peds | 10% peds/wk | 25/wk | 20/Case | 1.25 Cases |
| IV tubing w/ standard macrodrip for adults | Same # as intermittent | 250/wk | 48/Case | 5 Cases |
| Needles, Butterfly, 23g | 10% peds/wk | 25/wk | 50/Box | 0.5 Boxes |
| Needles, Butterfly, 25g | 10% ped/wk | 25/wk | 50/Box | 0.5 Boxes |
| Needles, sterile 18g | 1 box/day | 7 boxes/wk | 100/Box | 7 Boxes |
| Needles, sterile 21g | 1 box/day | 7 boxes/wk | 100/Box | 7 Boxes |
| Needles, sterile 25g | 1 box/day | 7 boxes/wk | 100/Box | 7 Boxes |
| Saline for injection 10cc bottle | 50 bottles/day | 350 bottles/wk | 24 /Box | 14.5 Boxes |
| ABD bandage pads, sterile | 10% pts/day = 5 pads/day+35 pads/wk | 7 boxes/wk | 50/Box | 7 Boxes |
| BandAids | 1 box/day | 7 boxes/wk | 50/Box | 7 Boxes |
| Basins, bath | 20 pts/day | 140/wk | 100/Case | 1.5 Cases |
| Bathing supply, prepackaged (e.g.Bath in a Bag (TM)) | 50 pts every day | 350/wk | 350 | |
| Bedpans - regular | 40 pts/day initially then 10% | 65/wk | 50/Case | 1.25 Cases |
| Toilet Paper | 25 rolls/day | 175 rolls/wk | 175 Rolls | |
| Blankets | 50 pts/day; changed daily | 50/day or 350/wk | 350/Week | |
| Carafes - 1 liter (for variety of uses) | 30/day | 210/wk | 210/Week | |
| Cart, supply | 3/unit (1 for IV's;1 for Pt | 3/unit | ||
| Chux protective pads (many uses) | 3/pt q3hrs = 24 chux/pt/day x 50 pts + 1200/day | 8400/wk | 50/Box | 168 Boxes |
| Cots (have extras available to replace broken equipment) | 50/unit plus 2 extra | 52/unit | 52/Unit | |
| Curtains, privacy (wheeled) | 25 (every other bed) | 25/unit | 25/Unit | |
| Diapers - adult | 10/day | 70/wk | 72/Case | 1 Case |
| Diapers - infant | 8/day/infant x 5 infants/day | 280/wk | 144/Case | 3 Cases |
| Diapers - pediatric | 5/day/ped x 5 peds/day = 25/day | 175/wk | 144/Case | 1.25 Cases |
| Emesis basins | 100/wk | 100/wk | 250/Case | 0.5 Case |
| Facial tissue, individual patient box | 1 box/pt/day | 350 boxes/wk | 200 Boxes | 1.75 Cases |
| Feeding tubes, pediatric | ||||
| - 5 French | 10/wk | 10/wk | 10/Box | 1 Box |
| -8 French | 10/wk | 10/wk | 10/Box | 1 Box |
| Foley Catheters - 16F Kits (includes drainage bag) | >50% of pts wk | 100/wk | 10/Case | 10 Cases |
| Gloves non-sterile, small/medium/large (latex and non latex) | 6 boxes/day | 42 boxes/wk | 100/Box | 42 Boxes |
| Goggles / face shields, splash resistant, disposable | 6 boxes/day | 42 boxes/wk | 100/Box | 42 Boxes |
| Gown, splash resistant, disposable | 3/staff/shift = 36/day | 252/wk | Box | 42 Boxes |
| Mask, N95, for staff (particulate respirator) | 36/day | 252/wk | 210/Case | 1.2 Cases |
| Gown, patient | 75/day | 525/wk | ||
| Mask, 3M 1800 for patient | 150/day | 1050/wk | ||
| Gauze pads, non-sterile, 4x4 size, | 400/day | 2800/wk | ||
| Hand cleaner, waterless alcohol-based | 1 per handwash station/day x | 28/wk | 25 Bottles/Case | 1 Case |
| Paper Towels | 25 rolls/day | 175 rolls/wk | 175 Rolls | |
| Lubricant, Water soluble | 1-2 boxes wk | 25 Boxes | 0.5 Boxes | |
| Medicine cups, 30ml, plastic | 2/pt/day = 100/day | 700/wk | 700/Week | |
| Morgue Kits | Tularemia: 15pt/day mortality | 300/wk | 300/Week | |
| Nasogastric tubes - 18F | 25/wk | 50/Case | 0.5 Cases | |
| OB Kits | 1/wk | 1/Week | ||
| Pen lights | 12/unit | 6/Box | 2 Boxes | |
| Povidone-iodine bottles, 12 oz | 2/day | 14/wk | 48 Bottles | 0.25 Cases |
| Restraints, Extremity, soft - adult | 25/wk | 48/Case | 0.5 Cases | |
| Sanitary pads (OB pads) | 2 women/wk; 10 pads/day | 20 pads/wk | 12 Pads | 2 Boxes |
| Sharps disposal containers - 2 gallon | 2-4/wk/unit | 2-4/wk | 20/Case | 0.25 Cases |
| Sheets, disposable, paper, for stretchers & cots | 100/day | 700/wk | 700/Week | |
| Syringes, 10cc, luer lock | 4 boxes/wk (100 ct box) | 400 wk | 100/Box | 4 Boxes |
| Syringes, 3cc, luer lock, w/ 21g 1.5" needle | 200/day | 1400/wk | 100/Box | 14 Boxes |
| Syringes, catheter tip 60cc | 25/wk | 50/Box | 0.5 Boxes | |
| Syringes, Insulin | 4/day | 28/wk | 100/Box | 0.25 Boxes |
| Syringes, TB | 2/day | 14/day | 100/Box | 0.4 Boxes |
| Tape, silk - 1 inch | 12/day | 96/wk | 12 Rolls/Box | 8 Boxes |
| Tape, silk - 2 inch | 6/day | 42/wk | 12 Bolls/Box | 3.5 Boxes |
| Toilet tissue | 25 rolls/day | 175 rolls/wk | 175 Rolls | |
| Tongue depressors | 2 boxes/wk | 500/Box | 2 Boxes | |
| Tubex [TM] pre-filled syringe holders | 1 per staff member plus | 12/sub-unit | 50/Case | 0.25 Cases |
| Urinals | 50/wk | 50/Case | 1 Case | |
| Washcloths, disposable | 10/pt/day | 3500/Wk | 3500/Week | |
| Water, bottled 1 liter (for mixing ORT) | 1/patient | 200/wk | 200/Week | |
| Water container, 1 gallon potable | 125/wk | 125/Week | ||
| Drinking cups | ||||
| Diagnostic Supplies | ||||
| Glucometer | 1 per unit | Each | ||
| Glucometer test strips | 2 bottles/wk | 50 Strips/Viles | 2 Viles | |
| Probe covers for thermometers | 4 boxes/day | 28 boxes/wk | 20/Box | 28 Boxes |
| Protocol unit (or other brand), 02 sat monitor, thermometer, BP, HR | 4 per unit | Each | ||
| Protocol unit, disposable plastic BP covers | 200/day | 1400/wk | ||
| Single Use Shielded Lancets | 25/day | 175/wk | 1 Box | |
| Stethoscopes | 12/unit | Each | 12 | |
Table 8. Administrative Consumables for Level III Comprehensive ACF Medical Cache (50 Bed Unit)
| Item Description |
|---|
| Pens - Black ballpoint |
| Pens - Red ballpoint |
| Stapler |
| Staples |
| Tape |
| Tape dispenser |
| Paper clips |
| Paper punch (3- or 5-hole based on chart holders) |
| Chartholders/Clip boards |
| File Folders - letter size, variety of colors |
| Namebands for Identification and Allergies |
| Batteries - 9V |
| Batteries - AA |
| Batteries - C |
| Batteries - D |
| Clipboards |
| Chalk or white boards |
| Dry-erase markers |
| Chalk |
| Trashcans and liners |
| Flashlights |
| Plastic bags for patient valuables |
| Floor lamps |
| Table lamps |
| Lightbulbs |
| Plain paper |
| Filing cabinets - rolling |
| Black permanent markers |
| Yellow highlighter markers |
| Time cards |
| Generic sign-in, sign-out forms |
| Pre-printed admission Order forms |
| Blank physician order forms |
| Multidisciplinary progress notes |
| Nursing flowsheets |
| Admission history & physical forms (include area for Nrsg Hx) |
| Death certificates/Death packets |
Table 9. Oxygen and Respiratory-Related Equipment Considerations for Level III Comprehensive Medical Cache (50 Bed Unit)
| Item Description | Quantity |
|---|---|
| Bag-Valve-Mask w/adult and peds masks - adult 1600 ml reservoir | 1 |
| Cascade gauge for oxygen cylinders | 14 |
| Catheters, suction | 20 |
| Connector, 5 in 1 | 8 |
| Cylinder holders for E Cylinder oxygen tanks | 4 |
| Mask, oxygen - nonrebreather, pediatric | 10 |
| Mask, oxygen - nonrebreather, adult | 20 |
| Nasal cannula, adult | 40 |
| Nasal cannula, pediatric | 10 |
| Regulator, Oxygen (Flow meter) | 14 |
| Suction unit - Collection System | 2 |
| Suction unit - Portable | 1 |
| Suction unit Battery | 1 |
| Tank, Oxygen "E" cylinder (700 L O2) | 4 |
| Tank, Oxygen "H" cylinder (7000 L O2) | 10 |
| Tubing, oxygen - with connector | 40 |
| Tubing - suction, connector | 10 |
| Tubing, suction, 10F | 10 |
| Wrench, Oxygen tank | 2 |
| Yankaur Suction Catheter | 10 |
| Intubation equipment with oral airways/ET tubes; adult & peds | 1 set |
| Ventilators | 1 |
Section References:
- Rocky Mountain Regional Care Model for Bioterrorist Events: Locate Alternate Care Sites During an Emergency. December 2004. Agency for Healthcare Research and Quality, Rockville, MD. Available at https://archive.ahrq.gov/research/altsites.htm.
- Hick JL, Hanfling D, Burstein JL, DeAtely C, Barbisch D, Bogdan G, Cantrill S. Healthcare Facility and Community Strategies for Patient Care Surge Capacity. Ann Emerg Med 44:253-61;2004.
- Skidmore S, Wall W, Church J. Modular Emergency Medical System Concept of Operation for the Acute Care Center: Mass Casualty Strategy for a Biological Terror Incident, May 2003.



