Leadership commitment is an important component of CE sustainability. Leadership support is facilitated by alignment and integration. This support starts with executive leadership but is necessary at all levels, including clinical and nonclinical leaders. A recent systematic review of the barriers and facilitators influencing the sustainability of hospital-based interventions by Cowie, et al., found that leadership buy-in was the second most cited facilitator for program sustainability after clearly accountable roles.4 Leaders can be motivated by data-driven decision making to achieve system goals.20
Ways To Support Centers of Excellence
To support CEs, leaders can:17,21
- Collate resources to further the mission.
- Set top-down expectations.
- Facilitate bottom-up engagement to provide accountability.
- Steer CEs through organizational structures and processes.
- Guide overarching initiative directions.
- Maintain urgency for aligned goals as complexities grow.
- Clarify expectations and resolve issues.
Leaders can also deploy social capital to motivate and inspire the workforce and fellow leaders to join an initiative as champions. CEs must include leaders in their work so they can independently articulate how a CE’s mission aligns with their institution’s mission. This articulation of the CE’s mission is important because it occurs in settings where executives discuss priorities to which CE leaders are not privy. Therefore, engaging leaders early and often is a key driver of CE sustainability. Leadership buy-in and support are essential for continuous, sustainable improvement, and CEs can collaborate with leaders as executive sponsors to drive quality and safety improvement.21
Clinical leaders do not need to be at the executive level to drive change. The clinical champion approach to implementation strategy suggests partnering with division chiefs, diagnosticians, nurse managers, and other leaders to mitigate barriers and achieve alignment when implementing efforts to enhance healthcare quality and safety. These clinical champions can address barriers at the provider level to create behavior change.22
CEs can collaborate with clinical champions to integrate their efforts to widen their impact. Peer mentorship between clinical champions can build intentionality and organizational capacity to sustain change within a health system. These efforts can make the practices of quality and safety endemic to care delivery systems and further integrate CEs to promote CE sustainability. Having powerful clinical leaders as partners is vital to supporting a culture of quality and safety across the system.
Finally, CEs should prioritize the design and development of sustainability plans that include business continuity and attrition mitigation. Succession plans for CE leadership ensure that the momentum built is not lost with changes in key positions. Formalized systems for organizational learning ensure that individual knowledge can be translated into institutional knowledge, making CEs more resilient to changes in personnel.23,24 Sustainable CEs are built by more than just a lead investigator and their research team; they are integrated into their institution and resilient to personnel and operational changes.
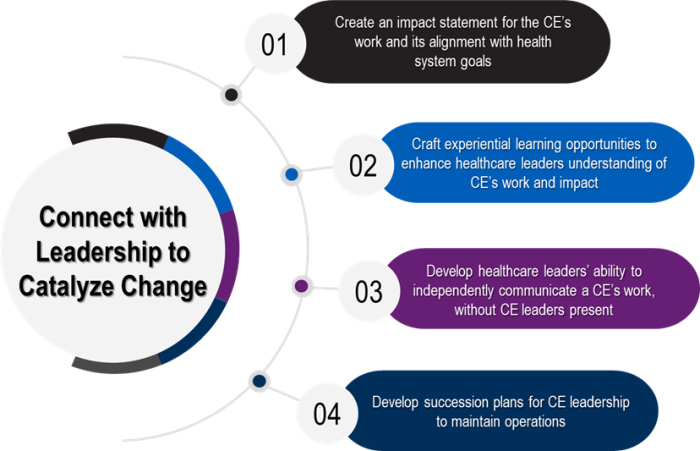
Exhibit 4. Four actions to connect with leadership to catalyze change
Guiding Questions for Leadership Support for CE Operations
- How would an institution’s executive leadership describe a CE’s mission and quality and safety initiatives? What impactful stories do they have to tell about a CE’s work?
- How could executive leadership be briefed on the CE’s work that impacts the institution’s mission?
- What succession plan exists for a change in personnel at the leadership level within the CE?
Experiential Learning for Leadership Engagement: NYC Health + Hospitals
Simulation is now an integral component of training for clinicians, broadly adopted by medical education programs.25 Komal Bajaj, M.D., M.S.-H.P.Ed., recounted the story of promoting simulation application and use to executive leadership in an effort to secure sustained resources for the simulation program. Dr. Bajaj is Chief Quality Officer at NYC Health + Hospitals/Jacobi/NCB and Clinical Director of Simulation. In one scenario, Dr. Bajaj and the team invited the CEO into a simulation exercise focused on de-escalation of a violent patient so that they could see firsthand how important the program was for training staff on complex clinical situations.
Experiencing this violent patient simulation gave the CEO new insights into how simulations equip clinicians with tactical skills to effectively address difficult situations and potential applications for simulation across the organization. Beyond a successful immersive meeting, this effort gave the CEO a storytelling opportunity to communicate the value of simulation as an innovative and integral part of clinical training at their institution.



