| This chapter helps venous thromboembolism teams better understand their current environment and process for providing VTE prevention. The focus here is on identifying barriers to improvement and failures in the current process in order to address them. |
Every improvement effort faces obstacles—both barriers and failure modes. In this guide the term "barrier" is used to describe more general problems that pose challenges; the term "failure mode" is used to describe more specific steps that need to be addressed in the local process.
It is useful to acknowledge as many obstacles as possible from the start and be prepared to face them, rather than to feel ambushed and disillusioned by their negative influence on the improvement effort as it unfolds.
Identify Common Barriers to Improvement
Some barriers are generic. Every medical center faces competing priorities and, increasingly, improvement fatigue. Negative inertia and resistance to change often slow things down. And while medical staff in many hospitals embrace a culture of teamwork and standardization, this is by no means uniform. Appendix A includes talking points to help improvement teams overcome some of the general malaise and garner the crucial leadership support needed to move forward.
Translating complicated guidelines into everyday practice is difficult. It is often just as important to figure out what parts of the guidelines not to address as it is to identify the most important aspects to reinforce so as not to risk overwhelming staff with information and decision support they cannot use. Conflicting guidelines from medical specialty groups can make standardization difficult. Meanwhile, the evidence for or against prophylaxis in certain subpopulations shifts occasionally, and the role of new anticoagulants in prophylaxis continues to evolve.
The evidence is imperfect and not all venous thromboembolism (VTE) prophylaxis issues are black and white. Yet the improvement team must make some decisions about its institutional approach to VTE prevention to allow standardization and measurement against a common definition of best practice. The team will be faced with defining the term "appropriate prophylaxis" for almost every kind of patient imaginable, taking into account clot risk, bleeding risk, and leeway times around surgeries when cessation of prophylaxis is acceptable and often desirable. The team will also need to settle on a VTE risk assessment model even though no definitive evidence exists for superiority of one model over others.
Existing measures and standards can also slow progress as they compete for leadership attention, staff time, and resources. While the National Quality Forum, The Joint Commission, Surgical Care Improvement Project, and meaningful use criteria for electronic health records (EHRs) are all in place, these measures do not necessarily drive rapid improvement—and administrative leaders may focus on these measures to the extent that they steal attention and resources away from more meaningful and useful measures.
The EHR and computerized physician order entry environment, while holding great promise, does not necessarily always provide a safer or more efficient environment for order sets or informatics. In fact, improvement efforts often grind to a halt for several months around the "go live" date for these systems.
Identify Common Failure Modes
In addition to more general barriers, there are a number of weaknesses in the processes specific to VTE prevention (Figure 2.1).
One common failure mode is the lack of standardized protocols or order sets for VTE prevention. This equates to Level 1 on the Hierarchy of Reliability. This failure mode can be broken down further into (1) VTE risk assessment is not routine or standard; (2) bleeding risk assessment is not routine or standard; and/or (3) there are widely different impressions of when it is safe to start anticoagulation peri-procedure and post-trauma—and no agreement on appropriate leeway times.
Too many order sets is a variant of this failure mode worth special mention. While some customization of order sets is desirable to serve the needs of populations with particularly high bleeding risks or deep vein thrombosis (DVT) issues that do not fit the more general population, it is easy to allow so many order sets that standardization within and across services becomes unwieldy, unreliable, and difficult to maintain. While some service-specific order sets are desirable, having too many does not reflect a standardized approach and can compromise institutional performance.
Conducting a survey of all order sets in common use can be difficult. It is important to do so, however, on any journey toward better institutional quality—and the lessons learned can be applied to a host of other conditions.
Another common failure mode is when order sets and prompts that reference VTE prevention are in place but provide inadequate guidance. For example, simply listing options for prophylaxis does not provide adequate guidance. Similarly, order sets that provide detailed guidance that is bypassed (or not used) are of no use to providers. Mandatory hard stops to complete DVT risk assessment are often required to secure optimal prophylaxis rates; many hospitals, however, do not have these in place.1-3 Order sets with guidance in place and used—but used incorrectly—is yet another failure mode. This is a common scenario when the order set is too time consuming or difficult to use.
These failure modes encompass the top two sources of breakdown in the process in Figure 2.1. Overcoming these failures will land the team at Level 3 on the Hierarchy of Reliability, with a projected 75 percent rate of appropriate VTE prophylaxis.
Additional common failure modes can include:
- Patient gets placed on the right prophylaxis, but VTE/bleeding risk changes and an adjustment is not made.
- Prophylaxis gets missed or changed on transfer to a perioperative setting.
- Correct prophylaxis is ordered but not administered (or the patient refuses treatment).
- Patient is not mobilized optimally.
- Preventable risk factors (e.g., central line) are not optimally managed.
- Prophylaxis is stopped at discharge even though the patient has indications for extended duration prophylaxis.
This list is not all inclusive, and an implementation team may well find more problems with the process of providing effective DVT prophylaxis to the inpatient population. This list does, however, cover the most pervasive problems; addressing them effectively should lead to very high rates of appropriate DVT prophylaxis.
Diagram Care Delivery To Identify Failure Modes
To create its interventions, the team will need to diagram care delivery. This may be viewed as a series of intermediate steps that lead to a clinical endpoint. Diagramming helps members to understand these interrelated steps and to identify where failures—or missed chances to prevent hospital-associated VTE (HA-VTE)—occur. These opportunities exist from the moment the patient is admitted and recur daily.
To help the team focus its time on the most high-yield interventions, it is extremely helpful to identify the most frequent sources of missed chances to prevent HA-VTE. By doing this type of analysis, the team can identify rate-limiting steps and recognize which steps can serve as metrics for preventing HA-VTE.
What the team learns from drawing and discussing a map of the current process can be surprising. The team may identify wasted or duplicated efforts, lack of consensus on the current process, hidden complexities, and opportunities to streamline or simplify the process.
Figure 2.1 is an example of a diagram of steps in care delivery for preventing HA-VTE, along with the most common areas of process failure.
Figure 2.1: Process Map of VTE Prophylaxis With Common Areas of Failure
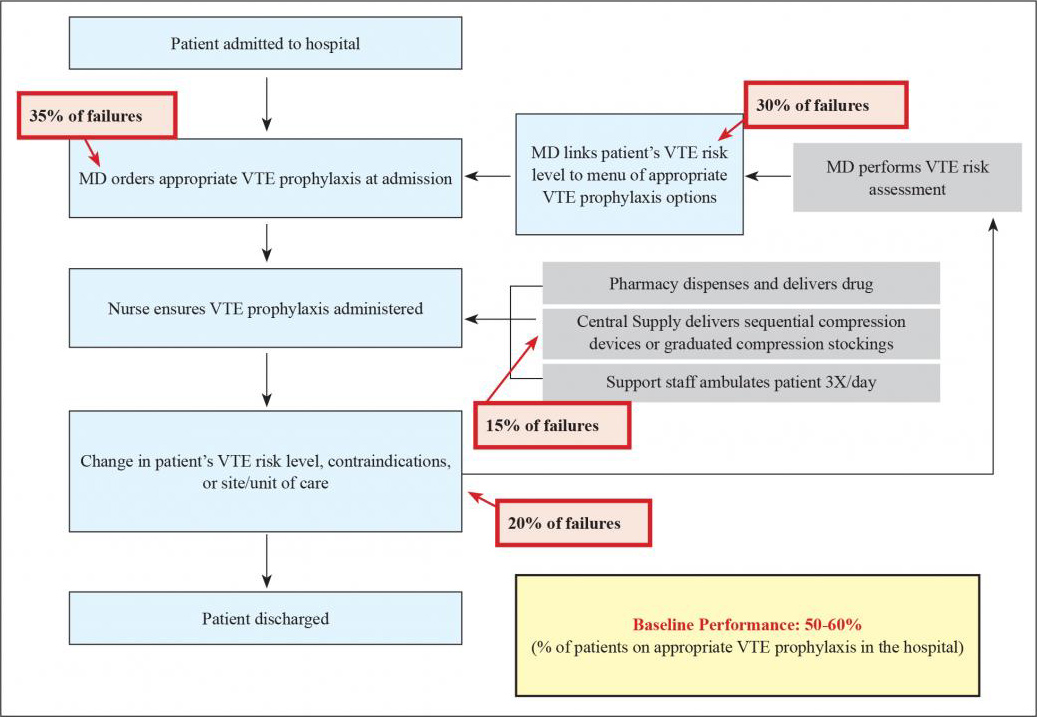
As a starting point in its analysis, the team should estimate how reliably each step occurs at its institution. For those steps that occur less than 100 percent of the time, the team will want to identify things that go wrong. This can reveal steps in the current process that are so obviously unreliable that they become the natural focus of interventions. Interventions can then be designed to address these failure modes and their underlying causes. The team should make an attempt at this point to prioritize these failure modes and to put some effort into delving into the root causes of why they occur.
The bulk of this guide addresses these barriers and is designed to help improvement teams navigate them and put in place effective protocols and processes to prevent VTE events.



