Daily Goals During Interdisciplinary Rounds: Facilitator Guide
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: Daily Goals During Interdisciplinary Rounds

Say:
In this session, we will discuss Daily Goals during interdisciplinary rounds.
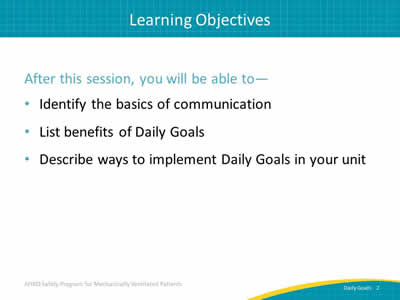
Slide 2: Learning Objectives
Say:
After this module, will be able to identify the basics of communication, list the benefits of Daily Goals, and describe ways to implement Daily Goals in your unit.
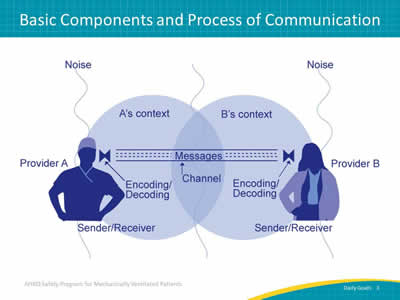
Slide 3: Basic Components and Process of Communication
Say:
This is an illustration of a simple line of communication in a clinical environment with competing, distracting sounds or noise. When considering the basic components and processes of communication, we need to discuss what is called "encoding" and "decoding" of messages. Through language, a message from one person to another is first “encoded” or changed into a sign or speech that is understandable. Once the message is received, it is then "decoded" or interpreted by the receiver through the act of listening. We have an intended message that we encode in our communications. Messages can be sent in various forms such as writing, speaking, or electronic messaging. Messages we encode and send to the person we are speaking with, writing to, or sending a message to electronically are not always decoded correctly or received in the way we intended. Competing or distracting sounds or noise can have an impact on communication and the decoding of messages.
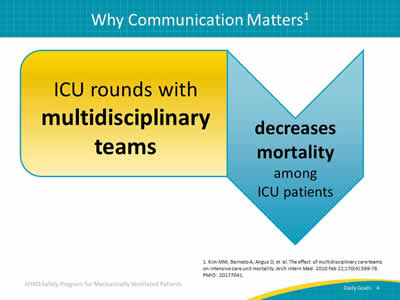
Slide 4: Why Communication Matters
Say:
Communication during intensive care unit (ICU) rounds with multidisciplinary teams has been shown to decrease mortality among ICU patients.
Slide 5: Why Communication Matters
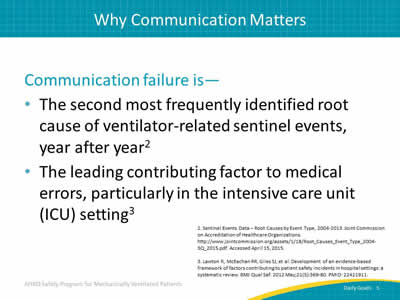
Say:
Year after year, studies show that communication failure is the second most frequently identified root cause of sentinel events. Communication failures are the leading contributing factor to medical errors, especially in the intensive care unit or ICU setting.
Slide 6: Why Communication Matters
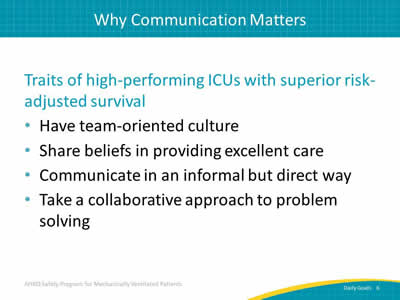
Say:
High-performing ICUs—or other clinical areas with superior risk-adjusted survival—reap the benefits of good communication. They have a good team-oriented culture and share their beliefs, strategies, and methods for providing excellent patient care. When teams collaborate and communicate well, often in an informal but direct way, patient harm is reduced. Finally, taking a collaborative approach to problem solving enhances communication and contributes to the improvement of patient care.
Slide 7: Barriers That Impact Communication

Ask:
What are some barriers that impact effective communication?
Say:
One barrier is interruptions. When you are in a clinical environment, you are interrupted throughout the day with various requests, questions, and comments. "I need that order." "Where can I find that supply?" "May I borrow your pen?" These kinds of interruptions affect your thought and behavioral patterns. Think about how you might mitigate or minimize the amount of interruptions in your clinical setting.
Another barrier to communication is verbal abuse. Verbal abuse exists and should be pointed out or mentioned, as it makes listening much more difficult.
Fatigue is another element that impacts how well you are able to both encode and decode messages.
Excessive workloads with multiple priorities can impact our ability to focus and communicate effectively. Any change or transition in team members affects operational flow and how you communicate.
Finally, when you are given ambiguous orders or directions, such as "wean the patient," rather than specific instructions such as, "wean the oxygen level to X", the intended message may not be received. Recognize that these are barriers to good communication and should be mitigated as much as possible.
Slide 8: Communication Breakdowns Cause Sentinel Events
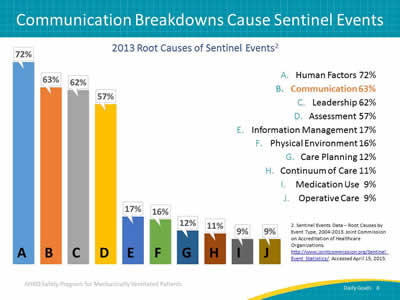
Say:
As mentioned earlier, ineffective communication is the second leading cause of sentinel events. Sixty-three percent of reported sentinel events are related to some form of communication failure. This is a recent development; communication was previously the number one cause of sentinel events. Currently, human factors that involve staffing levels, staffing skill mix, staff orientation, and things related to how humans interact with their environment, are considered the greatest contributing cause of sentinel events.
Slide 9: Benefits of Daily Goals
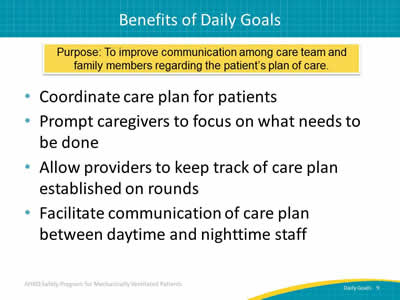
Say:
The purpose of Daily Goals is to improve communication among the care team and family members regarding the patient’s plan of care. It is both a tool and a process. The intention of a Daily Goals process is to have a coordinated care plan for the patients. It prompts the caregivers to focus on what needs to be done for the patient, while allowing the providers to keep track of the care plan during the rounding process. Defining your Daily Goals process will facilitate communication of the care plan for the patient between your a.m. and p.m. staffs. Conversations during transitions and handoffs will be more informed and accurate.
Slide 10: Daily Goals and Outcomes

Say:
From a study examining the effectiveness of communication during patient care rounds in the ICU by using a daily goals form, this graph shows an increase in residents’ and nurses’ understanding of Daily Goals per week. Over 6 weeks, the residents and the nurses developed a greater understanding of and appreciation for the Daily Goals and how to carry out orders to improve patient outcomes.
Slide 11: Daily Goals and Outcomes
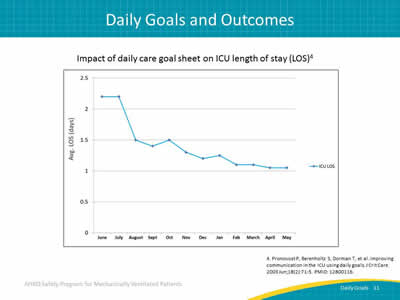
Say:
In addition, when residents and nurses understood and used the Daily Goal sheet over the course of 12 months, the average ICU length of stay or LOS decreased by more than a day.
Slide 12: Conventional Rounds

Say:
Communication defects are common during conventional rounds. They are too often provider-centered rather than patient-centered. In conventional rounds, "divergent" discussions or brainstorming is part of the rounding process, as opposed to convergent discussion where an explicit plan is developed. While brainstorming is important during rounds, developing an explicit daily plan of care for the patient is paramount. Asking the question "What are our daily goals of care for this patient today?" will provide opportunities to have some effective real-time feedback regarding the patient’s plan of care.
Slide 13: Rounds With Daily Goals
Say:
Integration of Daily Goals into the rounding process will help you create explicit goals for your patient’s plan of care. It will enable and enhance feedback among team members as they strive to maximize patient outcomes. Daily Goals will also standardize communication, which will result in the reduction of encoding and decoding errors. Creating independent checks or a "double-check system/real-time feedback" will help to ensure that all patients receive the evidence-based interventions necessary for the established plan of care. During the rounding process, develop convergent thinking with diverse input from various disciplines to achieve an explicit plan of care.
Slide 14: Daily Goals Improve Communication and Care

Say:
Standardizing communication with the use of Daily Goals will reduce encoding and decoding errors. Through the encouragement of diverse and independent input from the frontline staff, perceptions of hierarchy will be diminished. A multidisciplinary approach will help create that explicit plan and will simultaneously improve team cohesion and communication. Creating redundancy with real-time feedback will help ensure that all patients receive the evidence-based therapies.
Slide 15: Using Daily Goals
Say:
The Daily Goals process is not just a checklist but a means to improve communication among team members regarding the patient’s plan of care. It is important to use explicit language during your discussions on Daily Goals. For example, it is not enough to say, "Wean the patient" but to also say how or to what level to wean the patient. Ask the important questions you need to have answered in order to help the patient progress. "What needs to be done to get the patient off the ventilator? What are our goals for the patient today?" The daily goals checklist should be completed for each patient during rounds. Supply real-time feedback by having the nurse read back the goals. This will help to ensure agreement among team members. Modify or tailor the checklist to better suit your unit’s needs.
Slide 16: Evidence Favoring Daily Goals
Say:
In 2003, Johns Hopkins Hospital doctors Peter Pronovost and Sean Berenholtz experienced firsthand the effectiveness of using Daily Goals in the ICU. The study showed that when the Daily Goals checklist was implemented, communication was significantly improved. Because the Daily Goals for the patient were clearly defined, it also decreased the number of questions that physicians received through pages in the middle of the night.
Slide 17: Evidence Favoring Daily Goals
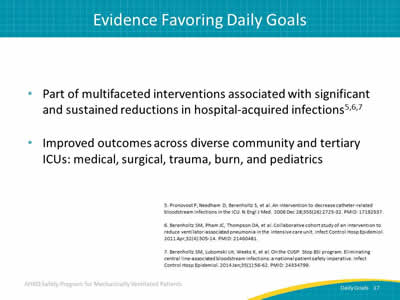
Say:
There is a preponderance of evidence that supports the benefits and use of a Daily Goals process. Using Daily Goals with multifaceted interventions was associated with significant and sustained reductions in hospital-acquired infections. Studies also showed an improvement in ICU length of stay, provider communication, understanding of patient care goals, and compliance with ventilator-associated pneumonia or VAP. The Daily Goals checklist has improved outcomes in the medical, surgical, trauma, burn, and pediatric ICUs and also aids in the transition of patients from one unit or clinical area to another.
Slide 18: Evidence Favoring Daily Goals
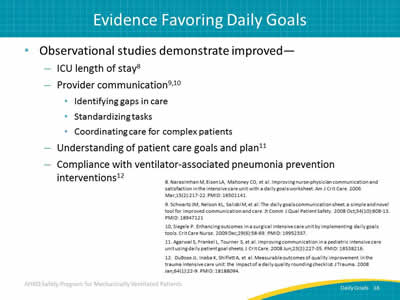
Say:
Observational studies have also shown that implementing a Daily Goals process results in improvements in ICU length of stay, provider communication, understanding of patient care goals, and compliance with interventions for preventing ventilator-associated pneumonia or VAP.
Slide 19: What Is Next? Preparing for Daily Goals

Say:
Multiple steps should be taken before creating your Daily Goals checklist. First, assess the current state of rounds on your unit. Look at samples of Daily Goals rounding tools that other units have used. Educate your providers by having them read the Daily Goals fast facts. Once you have taken these initial three steps, you can then present the idea to your ICU team. Be sure to obtain support from an ICU physician to champion the effort. Draft a Daily Goals checklist suitable to your unit and then pilot the tool during rounds to solicit early feedback. Having obtained feedback from multiple disciplines, you can then finalize your Daily Goals rounding tool.
Slide 20: What Is the State of Rounds on Your Unit?
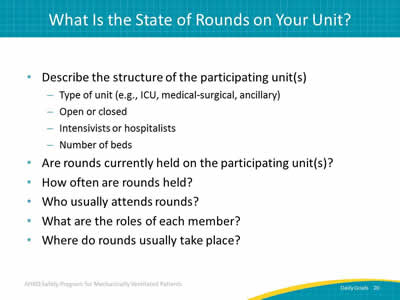
Say:
Describe the structure or the type of unit you have.
Ask:
What type of unit do you have, and is it opened or closed?
Do you have intensivists or hospitalists?
How many beds are on your unit?
Are your rounds currently held on your unit and how frequently are they held?
Say:
Ask the who, what, and where questions pertaining to your individual unit’s rounds.
Slide 21: What Is the State of Rounds on Your Unit?
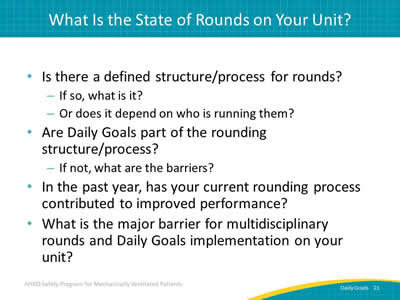
Say:
It is also important to consider your currently defined structure for rounds.
Ask:
What is the process and does it vary depending on who is running the rounds?
Are daily goals a part of your rounding process?
In the past year, has your current rounding practice contributed to improved performance?
If Daily Goals are not part of the rounding process, what is the barrier to having multidisciplinary rounds and implementing Daily Goals on your unit?
Say:
Asking these questions will help you determine the state of your current processes for rounding and can ignite ideas on what can be done to improve them by promoting multidisciplinary communication and teamwork.
Slide 22: References
Slide 23: References
Slide 24: References