Overview of the Comprehensive Unit-based Safety Program for Application to Mechanically Ventilated Patients: Facilitator Guide
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: Overview of the Comprehensive Unit-based Safety Program for Application to Mechanically Ventilated Patients
Say:
Today, we will be giving you an overview of the Comprehensive Unit-based Safety Program or CUSP, the Staff Safety Assessment or SSA, and the premortem exercise.
Slide 2: Learning Objectives
Say:
After this session, you will be able to explain the vision of CUSP teams, list the five steps of CUSP, describe the benefits of the SSA and be able to administer it, and conduct a premortem exercise with your team to proactively identify safety risks.
Slide 3: Comprehensive Unit-based Safety Program (CUSP)

Say:
We will begin with an overview of CUSP.
Slide 4: Why CUSP?
Say:
CUSP is an adaptive intervention that helps teams identify and learn from mistakes, improve safety culture, and improve teamwork. Putting a new procedure or process in place requires a change in priorities, beliefs, habits, and attitudes. CUSP is designed to improve safety culture and help teams learn from mistakes. Through the CUSP process, we come to value the wisdom of frontline staff and see how everyone who works on our units or in our clinical areas has some knowledge to add about how we can make care safer. Teams who engage in CUSP empower staff to be actively engaged in the safety improvements that take place on their units and in their clinical areas. We know CUSP has been linked with improvements in clinical outcomes and human resource outcomes, such as nurse staffing and turnover. And, finally, CUSP helps teams eliminate barriers between staff and senior leadership by making both active members of the CUSP team.
Slide 5: CUSP Vision
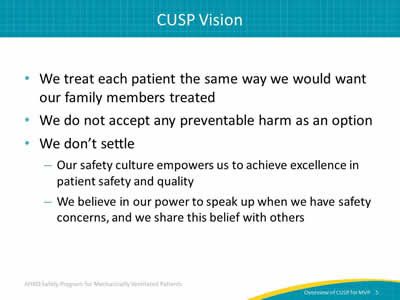
Say:
The vision of CUSP is that, by putting this team in place, we are saying that preventable harm is not an option. We are saying we need to ensure a safety culture that empowers us to achieve excellence in patient safety and quality. We are affirming that everyone in our clinical area has the power to speak up about safety concerns and should be listened to when they do share their concerns.
Slide 6: CUSP Vision
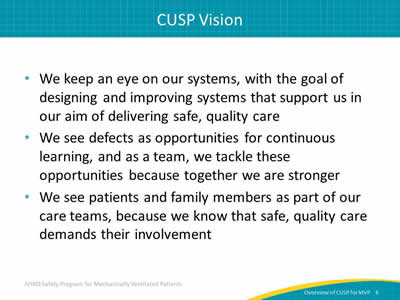
Say:
CUSP teams commit to developing system lenses that they can use to design and improve care. They adopt the attitude that defects have something to teach us about how care can be improved. They include patients and families as part of the care team and encourage them to speak up.
Slide 7: Steps of CUSP
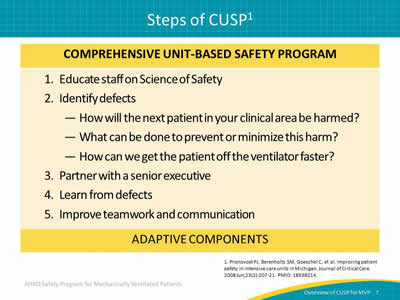
Say:
These are the steps of CUSP. It is a five-step process. The first step is educating staff on the Science of Safety. The second is identifying defects. The third step is partnering with a senior executive. In the fourth step, teams learn a process through which they can learn from the defects that occur in their clinical area. The fifth step is to improve teamwork and communication through the use of tools.
Slide 8: Steps of CUSP
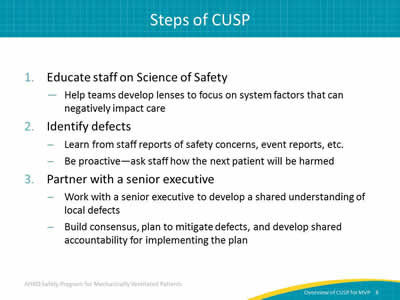
Say:
The first step of a CUSP program is to help teams develop lenses to focus on system factors that can negatively impact care. When we develop lenses that allow us to see those system factors and how they influence care, we can see the risks of patient harm that exist within our clinical area. The second step is to use our developing system lenses to identify areas for improvement in the unit using both retrospective and prospective approaches.
Ask:
What is a defect?
Say:
A defect is anything that can happen clinically or operationally that you do not want to have happen again. It is an unsafe condition. It could be a patient fall, a venous thromboembolism, a medication error, ventilator-associated pneumonia, or anything that can lead to preventable patient harm. We can learn from staff reports of safety concerns and event reporting, but we can also be proactive by asking staff how the next patient on our unit will be harmed.
The third step of CUSP involves partnering with a senior executive.
Ask:
Having leadership involvement in CUSP efforts is critical, but why?
Say:
Improvement efforts are a shared responsibility. When we include a senior executive as an active member of the CUSP team, we are helping to ensure that the team has access to resources to support its implementation efforts and that its efforts are aligned with the goals of the health care organization. It is vital that a senior executive is an active member of the CUSP team.
Slide 9: Steps of CUSP
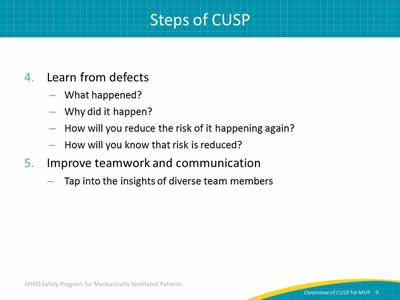
Say:
The fourth step of CUSP is learning from defects. It is not enough to identify defects; the learning from defects process asks four questions that help us understand and identify the factors that contribute to defect occurrence, and develop and implement interventions to reduce the risks of defect occurrence in the future.
So, what happened? It is not enough to simply understand what happened. It is also important to understand from the point of view of the people who were involved in the event—both staff and patients—what happened and what else was happening in the environment when the event occurred. First ask, how did the defect happen? By identifying how the defect happened, we get to the point where we can understand what system factors contributed to defect occurrence and why it happened. With this information, we are able to develop and implement interventions that help us to reduce the risk of future defect occurrence.
The next step is asking, what will you do to reduce the risk of this defect?
The final, very important step—which often gets overlooked—is, how do you know the risk was reduced? No matter what intervention we put in place, it is very important to go back and make sure—through observation and through some data collection—whether the intervention we implemented needs to be perhaps revised to achieve the results that we want to have.
The fifth and final step of CUSP is that, throughout the process, CUSP teams use teamwork tools to become stronger.
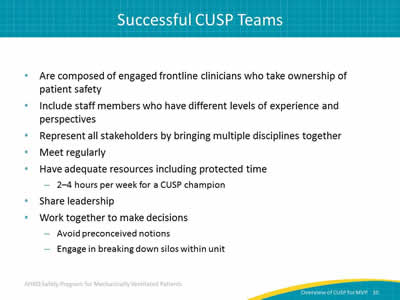
Slide 10: Successful CUSP Teams
Say:
When you build your CUSP team, it is important to develop a multidisciplinary team that includes a variety of frontline clinicians who take ownership of patient safety.
Ask:
Why is this important?
Say:
Staff members with differing levels of experience and perspectives are also necessary for a successful team. The varying disciplines, experience, and perspectives bring strength to our solutions. We know that successful CUSP teams meet regularly. CUSP teams need to have adequate resources, and this includes protected time. A CUSP champion should be allowed 2 to 4 hours a week of protected time. Successful CUSP teams share leadership; they don’t rely just on one person for every project or activity. They seek to engage people who have the knowledge, skills, and ability to lead the many components of change as you seek to improve care in your unit. They work together to make decisions. That means that they avoid preconceived notions about what the solutions are or about what the other members of the team bring to the table. And, they engage actively in breaking down silos within the unit, so that they come to see themselves as members of the team that is actively involved in providing the best care that they can for the patients admitted to their units.
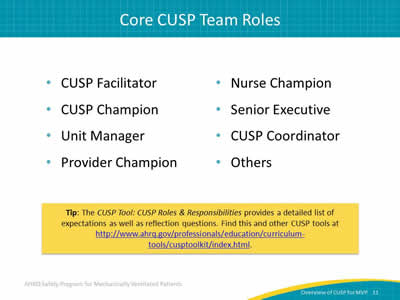
Slide 11: Core CUSP Team Roles
Ask:
What are the core roles needed for a successful CUSP team?
Say:
The CUSP facilitator supports others as they achieve exceptional performance. A CUSP champion is also crucial to the success of your team. This champion works to ensure that the vision of CUSP is translated into action and that all staff members are engaged. The CUSP champion helps educate, sets the agenda for your meetings, reviews project status, and maintains awareness of the resources that are needed and the barriers that are encountered by both the core team and frontline providers as they implement the work; they serve as a contact for staff questions and feedback. The CUSP champion should make sure everyone on your staff receives Science of Safety training. As you get new residents or new fellows, make sure that the new people who join your team complete Science of Safety training during their orientation so that everyone in your team, unit, or clinical area is on the same page with respect to CUSP and the Science of Safety.
The provider champion is often a physician, but consider whether you need a champion (or champions) from other disciplines representing the frontline providers on your unit who are affected by or key to the changes being implemented. You may need to include champions on your team who are physical therapists or respiratory therapists—in addition to physician champions and nurse champions—who will help to guide your team through this work.
Identify physician and nurse champions who model leadership for the CUSP team and demonstrate a commitment to the program by actively participating in CUSP work. A physician champion might be the unit director, the chief medical officer, or a senior clinician who other clinicians admire and respect. A nurse champion could be the charge nurse, the nurse manager, or any staff nurse who is communicative and committed to improving your safety culture. Create an agreement that clearly identifies what is expected of the champions and provides a plan for regular reviews of their performance, as well as the performance of other team members.
The senior executive must be an active member of the CUSP team who meets with the team on a monthly basis. They partner with team members to help them achieve their goals by prioritizing safety initiatives, identifying resources, and reducing barriers that might prevent a team’s ability to succeed. The senior executive helps the team to understand the organization’s strategic goals and ensures that the work that the team is doing is aligned with those goals. They also connect the team to stakeholders, making those in administration and management aware of the efforts that the team is making to improve patient care. The senior executive can also serve as mentor or role model to other teams that are interested in forming a CUSP team and doing similar work.
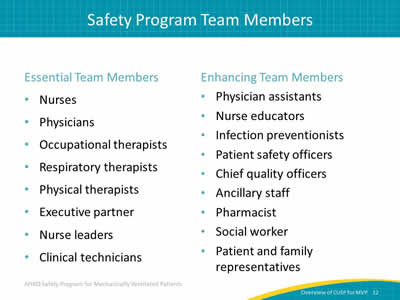
Slide 12: Safety Program Team Members
Ask:
Who else can we include?
Say:
These are some of the essential and enhancing members and roles that you should consider in your safety program to improve care for mechanically ventilated patients. The left column includes those roles that are essential for this type of project. The right column describes roles that include disciplines, knowledge, and experience that may greatly enhance team's success.
Slide 13: Strong CUSP Teams
Say:
Strong teams have a strong team orientation.
Ask:
What is a strong team orientation?
Say:
Strong teams believe they are a team and they function as a team. They recognize themselves and believe they have additional strength when they work together. They have a shared mental model of the team’s mission and they work together to achieve that mission. Finally, they build frameworks for team behaviors or norms, so that everyone on the team is aware of what the team’s goals are and how they will work together to ensure success.
Slide 14: Staff Safety Assessment (SSA)

Say:
Now, we will discuss the Staff Safety Assessment or SSA.
Slide 15: Principles of Science of Safety
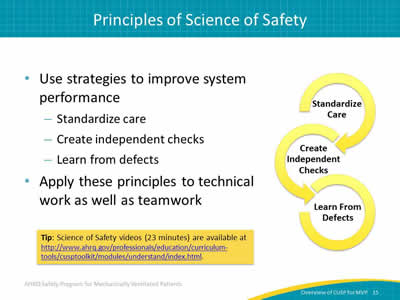
Say:
System performance can be improved by implementing the following strategies: standardize care wherever possible and wherever it makes scientific sense, create independent checks, and finally, learn from defects. These principles can be applied not only to technical work but teamwork as well. When engaging viewers during the Science of Safety video, think about safety events in your clinical area.
Ask:
What systems might have led to these events?
How can those principles of safe design be applied to prevent future events?
How can staff and others in your clinical area improve communication?
And, how can these concepts be applied?
Slide 16: Staff Safety Assessment
Say:
The Staff Safety Assessment taps into the wisdom and knowledge of frontline providers in the area and uses that knowledge to guide efforts to improve safety. By leveraging staff member knowledge, the Staff Safety Assessment allows teams to determine risks that have jeopardized or could jeopardize patient safety on a unit.
Ask:
Why is staff member knowledge so valuable?
Say:
Frontline staff members are the eyes and ears of patient safety and can list valid improvement opportunities and focus your safety program activities through use of the Staff Safety Assessment. The Staff Safety Assessment provides insight into potential solutions and leverages important frontline wisdom that you can use to guide patient safety efforts.
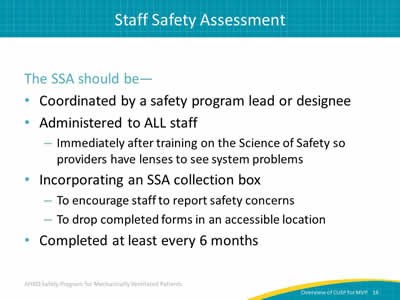
Slide 17: Staff Safety Assessment
Say:
The Staff Safety Assessment asks three questions of the frontline staff: How will your next ventilated patient be harmed, what can be done to prevent or minimize this harm, and how can we get the patient off the ventilator faster? By asking these simple questions, you release the wisdom and knowledge the frontline staff has concerning the risks that exist within their clinical area and about how those risks can be prevented. This assessment tool does not ask how an individual provider might harm a patient, but rather, it seeks to identify threats in the clinical area that can result in harm to your ventilated patients.
Slide 18: Staff Safety Assessment
Say:
A safety program lead or a designee should coordinate the SSA. It should be administered to all staff. Introduce the Staff Safety Assessment immediately following the Science of Safety training, while your team is together and engaged. Having completed the Science of Safety training, providers will have begun to develop those system lenses which are alert to potential patient harms in the work area. You might consider establishing a collection box where staff can submit completed Staff Safety Assessments in an accessible location with anonymity. We recommend completing it at least every 6 months. Some clinical areas use an ongoing process in which forms are readily available so that staff members can complete the Staff Safety Assessment whenever they have something to report.
Slide 19: SSA: Next Steps
Say:
Some ideal times to present the Science of Safety video to administer the SSA to your staff may be during medical staff grand rounds, orientation for new staff, regularly scheduled staff meetings, special educator sessions, or lunch sessions. Make it as convenient to your staff as possible by making the video available in the break room or on the hospital intranet.
Slide 20: Training Steps and Tools

Say:
What are some tools we can use to facilitate the next steps in safety training? The 23-minute Science of Safety video is one tool you can use to educate the team of Science of Safety. There is a Science of Safety training attendance sheet you can use as a tool to record the staff that completes training. The SSA is used to administer the assessment itself. This learning module can be referenced when sharing the collated results of the SSA with your team members.
Slide 21: Interpreting SSA Results
Say:
The defects identified during the assessment should be prioritized using the following criteria: the likelihood of the defect harming the patient, the severity of harm the defect causes, the frequency of the defect occurring, and the likelihood of preventing that defect during daily work.
Slide 22: Key Takeaways
Ask:
What are the key takeaways from the materials covered so far?
Say:
The main concepts to bring with you on your quality improvement journey are—
- Patient safety efforts extend beyond the use of checklists.
- CUSP teams integrate adaptive work and principles of safe design into daily activities.
- The Staff Safety Assessment is a valuable tool that can be used to tap the wisdom and insights of your frontline staff to get a realistic view of potential dangers in your unit.
Slide 23: Premortem Exercise

Say:
We will now discuss the premortem exercise.
Slide 24: Preparing to Lead
Say:
In a postmortem, an autopsy is performed to learn why a patient died. While it may be helpful to those interested in the results, it does not help the central figure in the medical drama—the patient. A postmortem is important, but a premortem exercise helps prevent the losses from occurring. The premortem exercise is used to identify potential barriers and vulnerabilities to the program success before they occur. This exercise builds intuition about and sensitivity to future problems.
Slide 25: Premortem Exercise
Say:
The first step of the premortem exercise is to imagine that you are two years into the future and, despite all your best efforts, your initiative has failed catastrophically. Maybe no one in your team is engaged or maybe no one has ever heard of the project and patient care has not improved. Ask yourself in this first step, what does your worst-case scenario look like?
Slide 26: Premortem Exercise
Say:
In step two, consider what could have caused the project to fail. As a group, consider all the reasons you think the failure occurred. Some examples might be that you are not able to find an engaged senior executive willing to participate or perhaps there are too many competing priorities. Each member of the team suggests a reason the initiative failed which can then be written out on a board that everyone can see.
Slide 27: Premortem Exercise
Say:
Once the potential reasons for failure have been identified, prioritize the list and address the top two or three concerns. Now, ask: what specific actions can you take to avoid or manage these concerns?
Slide 28: Premortem Exercise
Say:
The last step is to review the list of things that might have caused your project to fail, and periodically review this list throughout the program. Resensitize yourself to the kinds of things that you anticipate and any problems that keep emerging.
Ask:
Why do we do this?
Say:
This process raises awareness and helps the team anticipate reasons for failure and try to mitigate them before they impact your success.
Slide 29: Premortem Exercise
Say:
This is a summary of the steps to work through as you conduct your premortem. First, consider 2 years from now and ask what the worst-case scenario could look like. Second, brainstorm with the team to determine factors which may have caused the failure of your project. Third, identify some specific actions you could take to avoid those factors and finally, review what you’ve learned and use those findings to proactively anticipate potential problems.
Slide 30: Questions?
Slide 31: References