Physician and Staff Engagement: Slide Presentation
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: AHRQ Safety Program for Mechanically Ventilated Patients
Physician and Staff Engagement
Slide 2: Learning Objectives
After this session, you will be able to—
- Identify the importance of staff and physician engagement.
- Apply the principles of motivation to engage staff and physicians.
- Identify activities which encourage physician engagement.
Slide 3: Leading Change1
"One of most common leadership mistakes is expecting technical solutions to solve adaptive problems."
—Heifetz, Leadership Without Easy Answers
1. Heifetz R. Leadership without easy answers. Cambridge, MA: Harvard University Press; 1994.
Slide 4: Technical and Adaptive Work
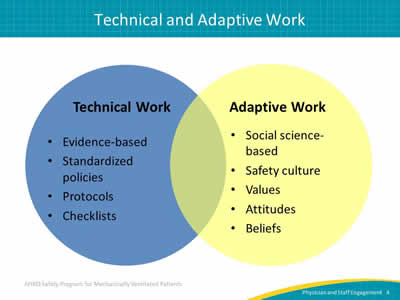
Image: Overlapping circles showing tenets of technical and adaptive work.
Technical Work:
- Evidence-based.
- Standardized policies.
- Protocols.
- Checklists.
Adaptive Work:
- Social science-based.
- Safety culture.
- Values.
- Attitudes.
- Beliefs.
Slide 5: What Would It Look Like If We…
- Enjoy great teamwork?
- Have a positive attitude?
- Attribute mistakes to the system rather than the provider?
- Encourage frontline staff to speak up about safety concerns?
- Engage the entire team?
Slide 6: Teamwork Disconnect2
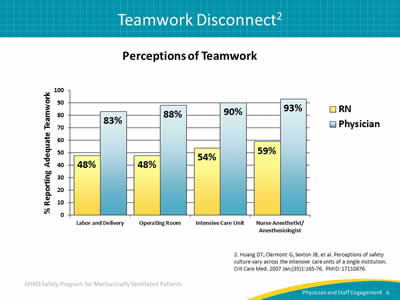
Perceptions of Teamwork
Image: Bar graph illustrating the different perceptions of teamwork between registered nurses and physicians, with physicians being almost twice as likely to report adequate teamwork as registered nurses.
2. Huang DT, Clermont G, Sexton JB, et al. Perceptions of safety culture vary across the intensive care units of a single institution. Crit Care Med 2007 Jan;(35)1:165-76. PMID: 17110876.
Slide 7: Why Does Safety Culture Matter?3-8
Safety culture is related to outcomes.
- Patient outcomes:
- Patient care experiences.
- Rates of infection and sepsis.
- Postoperative hemorrhages.
- Respiratory failure.
- Patient injury.
- Treatment errors.
- Clinician outcomes:
- Incident reporting.
- Burnout and turnover.
3. Huang DT, Clermont G, Kong L, et al. Intensive care unit safety culture and outcomes: a US multicenter study. Int J Qual Health Care 2010 Jun;22(3):151-61. PMID: 20382662.
4. Mardon RE, Khanna K, Sorra J, et al. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf 2010 Dec;6(4):226-32. PMID: 21099551.
5. MacDavitt K, Chou SS, Stone PW. Organizational climate and health care outcomes. Jt Comm J Qual Patient Saf 2007 Nov;33(11 Suppl):45-56. PMID: 18173165.
6. Singer S, Lin S, Falwell A, et al. Relationship of safety climate and safety performance in hospitals. Health Serv Res 2009 Apr;44(2 pt 1):399-421. PMID: 19178583.
7. Sorra JS, Dyer N. Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Serv Res 2010, 10:199. PMID: 20615247.
8. Weaver SJ, Salas E, King HM. Twelve best practices for team training evaluation in health care. Jt Comm J Qual Patient Saf 2011 Aug;37(8);341-9. PMID: 21874969.
Slide 8: Why Does Safety Culture Matter?8-11
- Safety culture influences the effectiveness of other safety and quality interventions:
- Can enhance or inhibit effects of other interventions.
- Safety culture can change through intervention:
- Best evidence so far for culture interventions that use multiple components.
8. Weaver SJ, Salas E, King HM. Twelve best practices for team training evaluation in health care. Jt Comm J Qual Patient Saf 2011 Aug;37(8);341-9. PMID: 21874969.
9. Haynes AB, Weiser TG, Berry WR, et al. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf 2011 Jan;20(1):102-7. PMID: 21228082.
10. Morello RT, Lowthian JA, Barker AL, et al. Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf 2013 Jan;22(1):11-8. PMID: 22849965.
11. Van Noord I, de Bruijne MC, Twisk, JW. The relationship between patient safety culture and the implementation of organizational patient safety defenses at emergency departments. Int J Qual Health Care 2010 Jun;22(3):162-9. PMID: 20382661.
Slide 9: Staff Engagement Matters12
- "The way people feel at work profoundly influences how they perform."
- Only 30% of American employees feel engaged at work.
- Across varying industries, companies that have higher levels of staff engagement have fewer safety incidences and overall better outcomes.
12. Schwartz T, Porath C. Why You Hate Work. The New York Times, May 30, 2014. http://www.nytimes.com/2014/06/01/opinion/sunday/why-you-hate-work.html?_r=0. Accessed April 3, 2015.
Slide 10: Staff Engagement Matters12
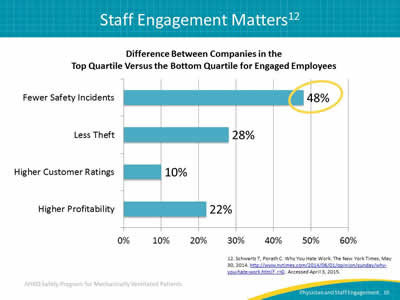
Difference Between Companies in the Top Quartile Versus the Bottom Quartile for Engaged Employees
Image: Bar graph highlighting how companies with highly engaged employees have 48 percent fewer safety incidents than companies with poorly engaged employees.
12. Schwartz T, Porath C. Why You Hate Work. The New York Times, May 30, 2014. http://www.nytimes.com/2014/06/01/opinion/sunday/why-you-hate-work.html?_r=0. Accessed April 3, 2015.
Slide 11: Engage
- Recognize that teamwork is a multidisciplinary partnership.
- Tailor message for different stakeholders:
- Answer "What’s in it for me?"
- Understand that people resist loss, not change.
- Try to surface and mitigate real AND perceived loss.
- Address concerns about physicians’ and nurses’ time.
Slide 12: Engage by Creating Trust
- Caring:
- Keep patients as the ultimate focus of safety efforts.
- Make harm visible with stories and data.
- Post baseline rates of compliance and/or infections.
- Competent:
- Show them the evidence.
- Share stories about when staff do the right thing.
- Example—When they use minimal sedation or ambulate patients.
- Use early wins to build support for the project.
Slide 13: Intrinsic Versus Extrinsic Motivation
- Focus on intrinsic versus extrinsic motivation:
- Extrinsic—financial, regulatory.
- Intrinsic—autonomy, mastery, purpose.
- Intrinsic motivators—inspire courage, promote resilience, foster respect, increase accountability.
- Extrinsic motivators—decrease creativity, encourage short cuts, foster short-term thinking, extinguish intrinsic motivation.
Slide 14: What Motivates Human Beings?13
Motivation 1.0—We need food, security, and sex.
Motivation 2.0—We respond to rewards and punishments.
Motivation 3.0—We have the drive to learn, create, and improve the world.
13. Pink D. Drive: The surprising truth about what motivates us. New York, NY: Riverhead Books; 2009.
Slide 15: What Motivates Human Beings?13
Autonomy—Control and choice over work:
- Task, time, team, technique.
- Accountability.
Mastery—Get better at what they do:
- Requires hard work and struggle.
- Requires engagement—goals, feedback, challenge and effort itself is rewarding.
Purpose—Be a part of something bigger.
13. Pink D. Drive: The surprising truth about what motivates us. New York, NY: Riverhead Books; 2009.
Slide 16: Try This
- Discover and reinforce common purpose.
- Identify a good physician and/or nurse champion:
- Motivated intrinsically.
- Courageous.
- Resilient.
- Respected.
- Communicator.
- Ask! People get involved when asked.
- Offer "lead" title, unit reputation, opportunity to present to leadership, highlight in local publications.
Slide 17: Fostering Physician Engagement
High engagement can be achieved by asking physicians in your hospital or unit to take part in the following activities—
- Serve as a clinical role model for evidence-based practices.
- Educate physicians about project goals and progress.
- Solicit other physicians to participate.
- Confirm staff reviews infection control reports of ventilator-associated event (VAE) rates monthly.
- Contribute to each VAE investigation.
- Partner with hospital leadership to track objective outcomes:
- Average duration of mechanical ventilation.
- Acute care length of stay.
Slide 18: Checklist for Engaged Physicians
- Confirm all physicians receive reports of current data:
- VAE rates and number of patients that develop a VAE.
- Performance on process measures.
- Objective outcome measures.
- Ensure your intensive care unit (ICU) has an overarching protocolized approach to daily ICU patient management including—
- Pairing spontaneous breathing trials with spontaneous awakening trials.
- Using 2013 Pain, Agitation, and Delirium Guidelines.
- Using noninvasive ventilation when appropriate.
- Using subglottic secretion drainage endotracheal tubes for patients likely to remain intubated more than 72 hours.
Slide 19: Engagement of the CUSP Physician Champion
- Evaluate results of the staff safety survey with quality improvement team:
- How can we get patients off the ventilator faster?
- Attend monthly executive partnership meetings.
- Foster organizational learning and actively participate in learning from defects process.
- Develop/adapt a patient-specific daily goals checklist for interdisciplinary rounds.
- Serve as a role model for Comprehensive Unit-based Safety Program (CUSP) efforts and implement tools to improve teamwork and communication.
Slide 20: Questions?
Image: A series of colored hanging tags with question marks on them.
Slide 21: References
1. Heifetz R. Leadership without easy answers. Cambridge, MA: Harvard University Press; 1994.
2. Huang DT, Clermont G, Sexton JB, et al. Perceptions of safety culture vary across the intensive care units of a single institution. Crit Care Med 2007 Jan;(35)1:165-76. PMID: 17110876.
3. Huang DT, Clermont G, Kong L, et al. Intensive care unit safety culture and outcomes: a US multicenter study. Int J Qual Health Care 2010 Jun;22(3):151-61. PMID: 20382662.
4. Mardon RE, Khanna K, Sorra J, et al. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf 2010 Dec;6(4):226-32. PMID: 21099551.
5. MacDavitt K, Chou SS, Stone PW. Organizational climate and health care outcomes. Jt Comm J Qual Patient Saf 2007 Nov;33(11 Suppl):45-56. PMID: 18173165.
Slide 22: References
6. Singer S, Lin S, Falwell A, et al. Relationship of safety climate and safety performance in hospitals. Health Serv Res 2009 Apr;44(2 pt 1):399-421. PMID: 19178583.
7. Sorra JS, Dyer N. Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Serv Res 2010, 10:199. PMID: 20615247.
8. Weaver SJ, Salas E, King HM. Twelve best practices for team training evaluation in health care. Jt Comm J Qual Patient Saf 2011 Aug;37(8);341-9. PMID: 21874969.
9. Haynes AB, Weiser TG, Berry WR, et al. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf 2011 Jan;20(1):102-7. PMID: 21228082.
Slide 23: References
10. Morello RT, Lowthian JA, Barker AL, et al. Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf 2013 Jan;22(1):11-8. PMID: 22849965.
11. Van Noord I, de Bruijne MC, Twisk, JW. The relationship between patient safety culture and the implementation of organizational patient safety defenses at emergency departments. Int J Qual Health Care 2010 Jun;22(3):162-9. PMID: 20382661.
12. Schwartz T, Porath C. Why You Hate Work. The New York Times, May 30, 2014. http://www.nytimes.com/2014/06/01/opinion/sunday/why-you-hate-work.html?_r=0. Accessed April 3, 2015.
13. Pink D. Drive: The surprising truth about what motivates us. New York, NY: Riverhead Books; 2009.



