Douglas M. Brock, Andrew A. White, Lauren Lipira, Patricia I. McCotter, Sarah Shannon, and Thomas H. Gallagher
Abstract
Purpose. The AHRQ-funded, 3-year demonstration project “Communication to Prevent and Respond to Medical Injury: A Washington State Collaborative,” sought to improve patient safety culture in eight health care organizations, with a focus on enhanced error disclosure practices. Establishing a robust culture of patient safety requires broad support from providers and staff. Yet, many organizations struggle to align attitudes and behaviors, in part because leaders often overestimate readiness for change. This study describes the development of the Organizational Change Scale (OCS), an instrument designed to assess organizational change in response to organization-wide interventions.
Methods. The 14-item OCS is grounded in the Kotter eight-stage model of organizational change and takes only a few minutes to complete. The instrument underwent expert review, pilot testing, and was ultimately administered to select providers, staff and leadership who were trained to support error disclosure at their health care organizations (disclosure coaches).
Results. A total of 251 participants across eight health care organizations attended disclosure coach training sessions; 79 (31.5 percent) completed the OCS. The OCS exhibited good internal consistency (α = 0.90) and was able to discriminate between programs. The highest organizational scale scores were seen for the first Kotter stage “Sense of Urgency,” and the lowest readiness was reflected by how organizations “Communicated the Vision” of patient safety to employees. Findings generally reflected ongoing organizational change but also evidence of improvement.
Conclusions. The OCS allows health care organizations to capture “snapshots” of readiness, from an organization’s first recognition that change is required to the establishment of policy reflecting successful adoption of new processes. It also holds promise for examining change across time. Rooted in theory, brief, and applicable to all health care employees, the OCS has a wide range of potential applicability.
Introduction
Health care organizations often struggle to implement and sustain programs targeting broad organizational culture and behavior change. Despite some high-level guidance,1 large-scale interventions focused on patient safety generally have not proven effective.2-4 When success does occur, the results are typically modest, difficult to sustain, and based on low quality study designs with little generalizability.5 Furthermore, health care leaders often find it challenging to predict their organizations’ chance of success.
Organizations go through a myriad of incremental shifts when seeking to transform the beliefs, actions, and policies that form their culture of patient safety. Inaccurate assessment of an organization’s readiness for change or progress through change may be one reason why culture change efforts fail. The literature thus far has principally focused on tools for measuring the success of specific interventions within a given context. These instruments are valuable for empirically guiding resource allocation and determining effectiveness in improving patient safety. For example, the widely used Agency for Healthcare Research and Quality (AHRQ) Hospital Survey on Patient Safety Culture (HSOPS)6 assesses perceptions of an organization’s state of patient safety and helps to identify areas for improvement. However, the HSOPS instrument does not assess the specific organizational factors that determine how, or if, change is occurring. Such tools that can examine readiness and organizational change are lacking. An ideal instrument would be based on current theory,7 brief, applicable across stakeholders, and settings, and easily interpreted.
John Kotter established a widely respected theoretical approach for understanding complex organizational change based on patterns found across industry and business settings.8-11 He described successful organizational change as a functional completion of a series of ordered phases. Progression through Kotter’s phases (Figure 1) occurs gradually and success can unfold across years or even decades. An organization’s successful completion of each phase is essential for overall success. AHRQ and the Department of Defense’s (DoD) have used Kotter’s model10,11 as a means to describe as a means to describe health care organizations’ efforts to establish a culture dedicated to the improvement of patient safety.
Figure 1. Kotter’s Phases of Organizational Change
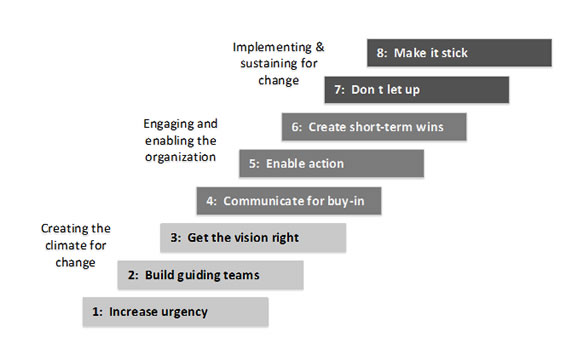
Adapted from: Kotter JP. Leading change: Why transformation efforts fail. Harv Bus Rev 1995; 73:59-67.
Kotter’s model for organizational change provides a theoretical framework for capturing an organization’s state of readiness for change, its adoption of new methods, and the impact of these methods on organizational culture. Using Kotter’s model, we developed the Organizational Change Scale (OCS). The OCS was designed to take only a few minutes to complete, to have broad application in health care settings, and to have longitudinal utility. In this paper, we first describe the development of the OCS. We then report on the preliminary use of this instrument in a multi-site, complex demonstration project designed to improve patient safety. Specifically, we administered the instrument to assess each participating organization’s readiness to change their culture of disclosure to patients and families following harmful medical errors. Interventions to improve skills around error disclosure constitute a good test of the OCS; successful interventions must navigate complex barriers, require routine monitoring and reporting, and will unfold across years.
Methods
The Intervention
The “Communication to Prevent and Respond to Medical Injury: A Washington State Collaborative” was a 3-year demonstration project funded by the AHRQ. Eight Washington State health care organizations (five hospitals and three multi-specialty provider groups) agreed to participate in a two-component intervention to enhance patient safety. The first component aimed to reduce medical errors by improving team communication through adoption of TeamSTEPPS®. TeamSTEPPS is a validated training program to reduce errors and improve health outcomes through improved communication within teams.
The second component of the intervention focused on a culture of transparency around error disclosure.12 Select providers, staff, and leadership were trained to be “disclosure coaches,” individuals who could respond to and support the needs of clinicians and patients following a medical error. Medical error was defined as the failure of a planned action to be completed or the use of a wrong plan to achieve an aim. Disclosure coaches strengthen clinician confidence and allow disclosure to occur in a timely fashion.13-16 In-person disclosure coach training sessions were conducted between March 19, 2012 and February 8, 2013, at all participating organizations. Training involved a mix of didactic and error disclosure simulation. A full description of the curriculum has been previously published.17
Participants
At each participating organization, disclosure coaches were selected by organizational leadership as well-respected individuals with excellent communication skills from varying professions and disciplines. At most organizations, this resulted in a mix of physicians, medical directors, nurse managers, risk managers, patient safety officers, and pharmacist managers. Total attendance at these eight sessions was 251 disclosure coach trainees (range 11-49 per institution). The activation of disclosure coaches varied between sites, depending on local protocols.
Instrument Development
The Organizational Change Scale (OCS) was developed to measure organizational change readiness at baseline and across time. Fourteen items were formed from existing descriptions of the key elements of each phase of the Kotter model (Table 1). Each of the items provides a Likert-style question with response options ranging from 1=strongly disagree to 5=strongly agree (Figure 2). An arithmetic average is calculated for the items composing each subscale. After development, items were then reviewed by demonstration project team investigators, each with significant expertise in program evaluation or psychometric design of scales. The first administration of the scale served as a pilot and did not raise any concerns for continuing to administer the scale. The instrument was designed to be used at multiple times during the demonstration project, supplementing other project instruments employed to explore the success of specific interventions. The University of Washington Internal Review Board (IRB) approved this study.
Table 1. Descriptive Statistics Aggregated Across Eight Hospitals
| Change Scale Category | n | Min | Max | mean | se | sd |
|---|---|---|---|---|---|---|
| Increase urgency | 78 | 1.0 | 5.0 | 4.09 | 0.12 | 1.05 |
| Build guiding teams | 79 | 1.0 | 5.0 | 3.87 | 0.09 | 0.77 |
| Get the vision right | 79 | 1.3 | 5.0 | 3.66 | 0.09 | 0.84 |
| Communicate for buy-in | 79 | 1.0 | 5.0 | 3.25 | 0.10 | 0.88 |
| Enable action | 79 | 1.0 | 5.0 | 3.58 | 0.09 | 0.84 |
| Create short-term wins | 77 | 2.0 | 5.0 | 3.78 | 0.09 | 0.77 |
| Don't let up | 79 | 1.5 | 5.0 | 3.58 | 0.09 | 0.79 |
| Make it stick | 78 | 1.0 | 5.0 | 3.68 | 0.10 | 0.85 |
Instrument Implementation
The OCS was administered as part of the second component of the demonstration project. We recruited all 251 trained disclosure coaches to complete the OSC via Web-based questionnaire. The survey was administered to participants an average of 40 weeks after the training session (range 3 to 75 weeks). The variation in administration time was due to the variation in training dates combined with a 5-month delay introduced by a revision to the IRB application.
Figure 3 shows two organizations (Hospitals 1 and 2) and illustrates observed differences in cultural readiness and achievement of change. These two hospitals were selected to demonstrate patterns observed across hospitals. They are not meant to suggest the relative success of these institutions. For Hospital 1, “Sense of Urgency” is relatively high; but later change stages, such as “Enabling action” and “Making it stick” through policy shifts are not strongly present. Both of these factors are predicted later in an organization’s culture evolution. Hospital 2 illustrates an organizational pattern that has achieved relative success for the majority of the Kotter phases. This is also true for “Policy,” defined as one of the last phases to emerge.
Discussion
We have described the OCS as an instrument to measure the “state” of readiness for changing culture within health care organizations. We have used data collected as part of a large-scale demonstration project, providing preliminary support for use of the instrument.
Figure 2. Organizational Change Scale Instrument and Instructions
|
Organizational Change Scale items, grouped by their corresponding phase of organizational phase of change Increase Urgency:*
Build Guiding Teams:
Get the Vision Right:
Communication for Buy-In:
Enable Action:
Create Short-Term Wins:
Don't Let Up:
Make It Stick:
Instructions to participant: This instrument asks you to indicate how you feel about statements that describe your health care organization’s readiness and support for organizational change. For each of the following questions please respond on the provided scale from1= “Strongly Disagree” to 5= “Strongly Agree”. A “Not Applicable” response has also been provided. *Note: During implementation, the “Phase of change” headings as noted above were not part of the administered tool. |
Figure 3. Two Hospitals in Different Stages of Cultural Readiness and Achievement of Change
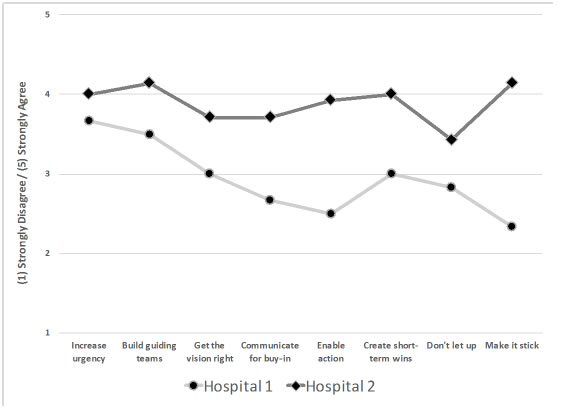
Three key themes emerged from our analyses of the OCS. First, organizations generally reported an urgent need for change, expressed significant concern that they could do better in meeting patient and organizational needs, and held interest in integrating efficient, effective, and sustainable programs to improve the culture of error disclosure. The OCS provides a theory-based profile of each organization’s dynamic state of change. Second, change is difficult. However, knowing which specific stages are showing success and which require additional support may guide individual organizations in focusing their attention and tailoring their change activities. Third, inspection of the profiles demonstrated that the OCS is sensitive across the range of Kotter’s stages of change.8-11 Some organizations exhibited patterns such as early recognition of urgency but having had little time or success in shifting the cultural of error disclosure. Some organizations exhibited patterns of more mature developmental shifts, with both early and later phases of Kotter’s model demonstrating success. The majority of organizations showed complex patterns suggesting it may not be optimal to think of each of Kotter’s phases as strictly building on previous phases. For example, positive policy changes might be demonstrated as a response to high-level shifts, while progress at lower phases is yet to be fully achieved.
Limitations
This study has limitations that must be taken into consideration when interpreting the reported results and in considering the OCS for future studies. First, each of the organizations described in this study agreed to participate in the demonstration project. Voluntary participation in a demonstration project may be correlated with an increased likelihood for promoting organizational change. Therefore, the results may not be generalizable to other organizations. Secondly, training implementation and data collection were challenging. Difficulties included obtaining support from leadership and securing time from participating clinicians to complete the OCS and other project activities. While the OCS took little time to complete, other aspects of the study data collection effort, including additional self-report questionnaires, may have been perceived as burdensome to the participants. These challenges may have contributed to a low response rate. For these reasons, further implementations of the OSC would contribute valuable validation evidence. Finally, the engagement of different organizations varied, and it proved difficult to obtain the necessary IRB approvals to administer surveys in a timely fashion. In the end, our instruments were administered at only a single point in time. Consequently, different amounts of time had elapsed between intervention and data collection at each organization.
Conclusion
The Organizational Change Scale (OCS) holds promise for health care organization stakeholders (e.g., leadership, insurers) as a means to provide a “snapshot” of the state of an organization. The instrument may also be of value to assess cultural change across time. The instrument’s ease of use and limited time requirements support its use in surveying employees broadly across organizations or narrowly within organizational units or to specific populations such as key leaders or organizational “change agents.”
Acknowledgments
Support for this work came from the Agency for Healthcare Research and Quality (Grant HS19531). The funder had no role in the design, conduct, or reporting of the study. We acknowledge and thank Benjamin Dunlap and Emily Brulotte for their contributions to coordination of data collection.
Author Affiliations
Douglas M. Brock, PhD, Associate Professor, Department of Family Medicine and MEDEX Northwest, University of Washington School of Medicine. Andrew A. White, MD, Associate Professor of Medicine, Interim Director of Hospital Medicine Programs, Division of General Internal Medicine, University of Washington School of Medicine. Lauren Lipira, MSW, PhD Candidate, Department of Health Services, University of Washington School of Public Health. Patricia I. McCotter, RN, JD, CPHRM, CPC, Former Director, Patient Safety Innovations and Provider Support, Physicians Insurance A Mutual Company/Experix. Sarah Shannon, PhD, Professor of Nursing, Senior Associate Dean for Academic Affairs, Oregon Health Sciences University School of Nursing. Thomas H. Gallagher, MD, Professor of Medicine, Associate Chair, Department of Medicine and Department of Bioethics & Humanities, University of Washington School of Medicine.
Address correspondence to: Douglas M. Brock, PhD, University of Washington, 4311 11th Avenue, NE, Suite 200, Box 354980, Seattle, WA 98195; email: dmbrock@uw.edu.
References
1. Salas E, Almeida SA, Salisbury M, et al. What are the critical success factors for team training in health care? Jt Comm J Qual Patient Saf 2009;35(8):398-405.
2. Flodgren G, Eccles MP, Shepperd S, et al. An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database Syst Rev 2011; (7):CD009255.
3. Parmelli E, Flodgren G, Schaafsma ME, et al. The effectiveness of strategies to change organisational culture to improve healthcare performance. Cochrane Database Syst Rev 2011; (1):CD008315.
4. Parmelli E, Flodgren G, Beyer F, et al. The effectiveness of strategies to change organisational culture to improve healthcare performance: a systematic review. Implement Sci 2011; 6:33.
5. Weaver SJ, Lubomksi LH, Wilson RF, et al. Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med 2013; 158(5 Pt 2):369-74.
6. Blegen MA, Gearhart S, O'Brien R, et al. AHRQ's hospital survey on patient safety culture: psychometric analyses. J Patient Saf 2009; 5(3):139-44.
7. Davidoff F, Dixon-Woods M, Leviton L, et al. Demystifying theory and its use in improvement. BMJ Qual Saf 2015; 24(3):228-38.
8. Kotter JP, Schlesinger LA. Choosing strategies for change. Harv Bus Rev 1979; 57(2):106-14.
9. Kotter JP. Leading change: why tranformation efforts fail. Harv Bus Rev 1995; 73:59-67.
10. Kotter J. Leading Change. Boston, MA: Harvard Business School Press; 1996.
11. Kotter J, Rathberger H. Our iceberg is melting: Changing and succeeding under adverse conditions. New York, NY: St. Martin's Press; 2005.
12. Etchegaray JM, Gallagher TH, Bell SK, et al. Error disclosure: A new domain for safety culture assessment. BMJ Qual Saf 2012 Jul; 21(7):594-9.
13. Gallagher TH, Waterman AD, Ebers AG, et al. Patients' and physicians' attitudes regarding the disclosure of medical errors. JAMA 2003; 289(8):1001-7.
14. Loren DJ, Garbutt J, Dunagan WC, et al. Risk managers, physicians, and disclosure of harmful medical errors. Jt Comm J Qual Patient Saf 2010; 36(3):101-8.
15. Gallagher TH, Garbutt JM, Waterman AD, et al. Choosing your words carefully: how physicians would disclose harmful medical errors to patients. Arch Intern Med 2006; 166(15):1585-93.
16. Gallagher TH, Waterman AD, Garbutt JM, et al. U.S. and Canadian physicians' attitudes and experiences regarding disclosing errors to patients. Arch Intern Med 2006; 166(15):1605-11.
17. White A, Brock D, McCotter P, et al. Implementing an error disclosure coaching model: a multicenter case study. J Healthc Risk Manag 2017 Jan; 36(3):34-45.



