James W. Pichert, Wendell W. Hoffman, David Danielson, Cindy Baldwin, Craig Uthe, Meghan Goldammer, Thomas F. Catron, Sue Garey, Jan Karrass, Peggy Westlake, Rhonda Ketterling, William O. Cooper, and Gerald B. Hickson
Abstract
Background. Patient complaints can help health care organizations identify physicians whose behaviors undermine a culture of safety and increase lawsuit risk. In 2010, the Sanford Health System (SHS) sought to plan and implement the Vanderbilt Center for Patient and Professional Advocacy’s (CPPA) Patient Advocacy Reporting System® (PARS®), which effectively addresses “high-risk” physicians identified via analysis of unsolicited patient complaints. More than 1,400 SHS-affiliated physicians provide care for a large patient volume outside major metropolitan areas, and SHS sought ways to enhance its culture of safety using the PARS tool and process for promoting professional self-regulation. This study describes planning for SHS’s PARS program launch and results of ongoing implementation through August 2016.
Methods. This retrospective, descriptive, planning and implementation project began with application of CPPA’s Project Bundle assessment tool, which directed development of key people, processes, and systems until PARS launch-readiness was achieved. SHS patient complaint databases were coded and analyzed to calculate a “Risk Score” for all affiliated physicians. SHS peer physicians were trained as "messengers" to share local and national PARS data comparisons with physicians whose Risk Scores exceeded intervention thresholds. Six rounds of annual interventions have been completed.
Results. Planning efforts resulted in a successful SHS PARS launch and ongoing implementation. The peer physician messengers have delivered PARS data with high fidelity to intervention elements over the past 6 years to 124 high risk physicians; 60 percent have improved, 7 percent have departed, and 33 percent are so far unimproved. Overall, recipients’ Risk Scores have declined 24 percent (p<.001). SHS’s return on investment in PARS exceeds $4 for every $1 spent.
Discussion. SHS and CPPA participated in a collaborative, comprehensive planning effort that has resulted in successful and sustained PARS implementation throughout SHS’s multi-State regional facilities. Lessons learned and limitations are discussed.
Conclusion. First, the Project Bundle offers health care leaders a useful pre-launch heuristic for identifying needs and addressing readiness of quality/safety and/or risk-prevention projects. Second, PARS works to reduce patient dissatisfaction and overall claims-related expenditures via interventions involving high-risk physicians in a large, geographically complex health care system.
Introduction
Patients and families are well positioned to help identify physicians whose behaviors undermine a culture of safety and increase lawsuit risk.1 If patient complaints—a proxy for malpractice claims—are reported, addressed via service recovery efforts, recorded, analyzed, aggregated, and used to provide feedback to the health care professionals involved, risk can be reduced.2-6 Specifically, research demonstrates a small proportion of physicians in any medical group are associated with disproportionate numbers of patient/family complaints.2,6-14 Research also demonstrates strong relationships between physicians’ unsolicited patient complaints, malpractice claims, and other risk management actions.7,8,15-18
Taking advantage of patients’ perspectives, the Vanderbilt Center for Patient and Professional Advocacy (CPPA) developed the evidence-based Patient Advocacy Reporting System® (PARS®) to: (1) promote professional accountability and self/group regulation; (2) optimize service recovery to address patient dissatisfaction; (3) identify physicians at increased risk for malpractice claims and effectively reduce their risk; (4) implement system-wide surveillance for behaviors that undermine a culture of safety, and (5) promote behavioral and practice/system changes that enhance a culture of safety.
CPPA currently partners with more than 140 hospitals nationally to implement PARS, resulting in a national comparative database of unsolicited patient complaints and shared operational best practices. CPPA continuously works with patient relations directors and representatives to achieve and maintain best practices in centralizing and increasing the recording of patient and family complaints for both immediate service recovery and pattern identification.6,19 CPPA codes, aggregates, and analyzes unsolicited patient complaint narratives recorded by patient relations staff. The data are used to calculate a Risk Score for all affiliated physicians. The Risk Score is based on a proprietary algorithm in which complaints about physicians filed in more recent years have greater impact than those from previous years. As a result of these efforts, CPPA creates evidence-based, actionable reports that include local and national peer comparisons from the PARS national database (described below), and extracts the text of relevant patient complaints.5-7,11-14,20
The PARS process of tiered interventions is depicted in Figure 1.2,3,21 PARS interventions are physician driven and have been implemented by trained peer physician "messengers" with excellent fidelity.3 High risk physicians—those whose PARS Risk Scores are associated with malpractice claims risk, generally those in the top 3-8 percent of a medical group’s members4—are recommended to be recipients of an Awareness Intervention. In these, a messenger physician colleague meets with a high-risk physician recipient to share PARS data (i.e., local and national comparisons, aggregated coded complaints, and full narratives). Most physicians take self‑corrective actions that address behavioral and systems issues that dissatisfy patients and are associated with risk.3
Figure 1. PARS Model of Tiered Interventions
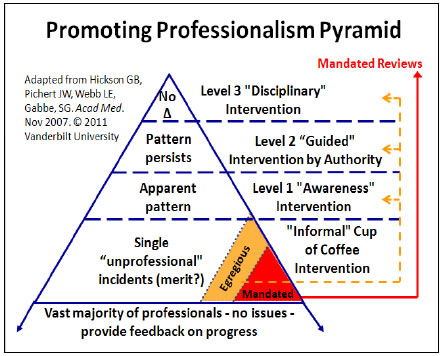
Source: Adapted from Hickson, Pichert, Webb, et al., 2007. Used with permission.
As a large, growing, geographically complex, multi-hospital, multi-outpatient-facility system, Sanford Health System (SHS) leadership sought tools and processes for continuing its tradition of promoting safety, quality, and risk reduction and doing so reliably. SHS expressed interest in PARS beginning in 2009 after learning CPPA had by that time supported several thousand initial and follow-up interventions nationally on physicians with high Risk Scores ("high risk" professionals) and that reductions in overall patient concerns and malpractice claims rates had resulted.3-6 SHS then applied for and was awarded an AHRQ planning grant in collaboration with CPPA.
Successful PARS planning and implementation deserve and require considerable thought and collaborative effort. Leadership of both SHS and CPPA were substantially involved in both the planning study and the move to implement PARS throughout SHS. Collaborative decisionmaking was guided by CPPA’s "Project Bundle" (Table 1), a heuristic for assessing an organization’s readiness to launch and implement PARS.2,22 The bundle includes three major categories—people, processes, and systems—and 10 subcategories. The tool simply but effectively reminds leaders and project initiators of essential elements that influence PARS success. Leaders, stakeholders, and other decisionmakers use professional judgment to reflect on each essential element’s capacity and ability to support PARS (or other safety, quality, or risk prevention projects). The bundle first helps identify project-critical elements deemed not sufficiently present or robust enough for program implementation. Those elements undergo development until launch readiness is mutually deemed sufficient to proceed. Perfection is not required, but willingness and commitment to improve current practices and sustain best practices are essential. The bundle also guides program planners’ and organizational leaders’ ongoing post-launch decisionmaking and development efforts when project goals are not being achieved.
Table 1. PARS-Specific Project Bundle: Characteristics of Organizations With Successful PARS Programs2
| People | 1. Leadership commitment to PARS. Leaders are prepared to address any and all professionals or other colleagues (regardless of seniority, rank, or financial considerations) whose behaviors appear to undermine a culture of safety. |
| 2. Project champion(s). These persons are trusted with key data and a commitment to confidentiality and have a history of persevering and inspiring others to overcome barriers to achieving aims. | |
| 3. An implementation team—a “messenger committee” of medical group members, patient relations representatives, legal and human resources experts, risk managers, physician and nursing leaders, and key administrators. Important team member characteristics include a reputation for trustworthiness and commitment to confidentiality; clinicians who are in practice or not far from it, willing to undergo training, able to communicate distressing information non-judgmentally, and are willing to hold accountable those unwilling or unable to make changes. | |
| Processes | 4. Clearly articulated organizational values and goals that align with PARS. |
| 5. Policies and procedures that address expectations for professional conduct and professional accountability. | |
| 6. A tiered model for interventions (Figure 1) when unsolicited patient and family complaints are aggregated over time. | |
| 7. Resources appropriate and sufficient to create (or improve) and sustain best practices in service recovery (e.g., patient relations staff, training, software for documenting and aggregating patient/family complaints). Also resources for professional assessment and wellness services, coaching/shadowing, practice redesign assistance, and other forms of support for high risk professionals. | |
| Systems | 8. Measurement tools, data and metrics for capturing, monitoring, reporting, and securely transferring data files to CPPA containing patient/family complaints, staff complaints, selected clinical metrics, affiliated physicians, and locations to assess risk. |
| 9. Processes for reviewing the data prepared by the CPPA PARS team, including individual points, trend lines, aggregated local comparisons, national comparisons. | |
| 10. Multi-level professional training for leaders and peer messengers about PARS science and politics for long-term implementation, management, and sustainability. |
The project had two major goals. The first was to assess SHS’s PARS readiness during a pre-launch planning and development phase. The second was to assess results of the PARS post-launch implementation phase, now in its sixth year. This paper will describe the pre-launch planning steps taken to increase the chances of PARS program success, changes in Risk Scores for recipients of PARS interventions, and evidence of return on investment for PARS program implementation. The methods employed during the pre-launch planning phase are presented and then followed by the methods used during the implementation phase. The results section is similarly organized. Key project bundle elements addressed during each phase are highlighted in each section.
Methods
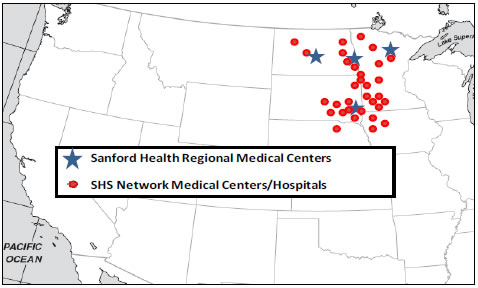
Setting. SHS is a relatively young system, formed in November 2009 via merger of mature regional systems with 100+ year histories centered in Sioux Falls, SD (hereafter "SHS South") and Fargo, ND (hereafter "SHS North") (Figure 2). SHS is one of the largest health systems in the Nation with 43 hospitals and nearly 250 clinics in nine States and three countries. SHS’s 27,000 employees include more than 1,400 physicians practicing in 80 specialty areas of medicine. SHS is committed to continuously raise its high standards for delivering compassionate, comforting care for patients, promising both patients and staff "a flawless experience that inspires."
Figure 2. Sanford Health Medical Center Sites in the North (Fargo, Bismarck) and South (Sioux Falls, Bemidji) Regions
Planning Phase. Evaluating "readiness" began with identifying and then addressing gaps in the project bundle elements. CPPA and SHS leaders continuously reviewed and, based on mutual experience and professional judgment, addressed the robustness of each bundle element via structured site visits, face-to-face meetings, frequent conference calls and email communications, training sessions, and discussions with all levels of SHS leadership and participants. The iterative nature of actions undertaken and length of time required to assure sufficient presence of each element prior to launching the PARS program are summarized in the Appendix Table, which indicates the people-specific, process-specific, and systems-specific methods and timeline. The methods used to address the various bundle elements are presented in the Appendix Table in order to illustrate how common program development and implementation challenges may be addressed, they reflect experiences similar to those employed by other organizations adopting PARS, they signal need for organizational commitment, and they are consistent with CPPA’s experience implementing a system for addressing co-worker concerns.22 These processes and activities resulted in the initial SHS PARS launch in late 2011.
Implementation Phase. As background, the Vanderbilt Center for Patient and Professional Advocacy (CPPA) currently works with more than 140 hospitals and medical groups (“participating health care organizations”) across 17 States to identify affiliated physicians who are associated with disproportionate levels of patient and family complaints relative to peers. CPPA maintains an electronic database containing securely transferred patient complaint and medical/surgical specialty data for more than 28,000 physicians with active practices who are credentialed at participating organizations.2-4 CPPA data analysis identifies physicians whose patient/family-reported complaints show them to be outliers from both their local peer groups and physicians from the other medical centers represented in the database.11-14 The Vanderbilt University Medical Center (VUMC) institutional review board approved a retrospective review of the patient complaint data from SHS and other participating health care organizations.
Complaint Data. Patient complaint data were obtained from the SHS North and South regions’ Offices of Patient Relations (“OPR”). The OPRs collected and recorded each patient or family complaint, identified the physician(s), if any, associated with alleged concerns, and created a narrative electronic report ("report") describing the issue(s). Reports were securely submitted to CPPA for entry into the PARS database for analysis. This study focused on complaints recorded between August 16, 2007 and August 15, 2016.
Coding System, Database, and Risk Scores. Trained research coders reviewed each SHS patient complaint report, identified distinct concerns embedded within them, and assigned each complaint a code. One report might contain several complaints (e.g., "doctor was very late for my appointment," "did not do a thorough exam," "did not let me know my test results"). All complaints were coded using a standardized system that sorted complaints into six categories: accessibility, billing, care and treatment, communication, concern for patient and family, and environmental. The system’s inter-rater and test-retest reliabilities have been previously established through related research.20 Coded data are used to calculate a Risk Score for all affiliated physicians. The Risk Score is based on a proprietary algorithm in which complaints about physicians filed in more recent years have greater impact than those from previous years.
Intervention Process. The principle underlying the PARS process is that identifying unnecessary variations in professionals’ behavior/performance and support system reliability is necessary, but not sufficient to increase patient safety, reduce malpractice claims, improve reliability, and increase professional accountability. In addition, the organization must support a systematic approach to promoting change in behavior or performance through peer-driven (at least initially), evidence-based, tiered conversations (Figure 1).2,6,21,23
Figure 1 reflects that the majority of health care professionals exhibit exemplary behavior, perform consistently well, and need only be given appropriate recognition and feedback about progress toward goals. The Pyramid’s first intervention level suggests that when what appears to be a single slip or lapse occurs, all that may be needed is an informal, non-authority conversation between peers, what we call a “Cup of Coffee” conversation.24-25 Note, however, that single incidents involving alleged violations of law, regulation, or policy (e.g., sexual boundary violations, practicing impaired, harassment) are mandated to be immediately referred to appropriate leadership and/or offices, agencies, and/or law enforcement for evaluation and consideration of corrective/disciplinary action. Other serious breaches of normative behavior that impact the work environment may be considered sufficiently egregious that they should be urgently addressed by the individual’s authority figure/supervisor or institutional authority.
If a documented pattern of concerning behavior/performance appears to have emerged, the PARS process calls for a Level 1 “Awareness” intervention. Awareness interventions are designed to be confidential, nondirective, non-punitive, evidence-based conversations in which a peer professional (most often) delivers observations/data that the recipient’s behavior/performance appears to vary from group expectations. If the pattern persists despite two or three rounds of Awareness interventions, the next step in the process is a Level 2 “Guided Intervention by Authority.” These involve an individual up the recipient’s chain of command (e.g., Department Chair, Chief Medical Officer [CMO], Chief of Staff, or other) and development of a specific action plan. Consistent with bylaws or other governing documents, the organization’s disciplinary process and higher levels of administration are involved in rare Level 3 “Disciplinary” interventions.6,21,24,25
For peer-based comparisons involving patient complaints, CPPA used SHS patient complaint data to calculate a Risk Score for each SHS-affiliated physician. The Risk Score is based on a proprietary algorithm in which complaints about physicians filed in the most recent year have greater impact than those reported during the 3 previous years. The Risk Score is presented in PARS feedback materials created for each SHS physician whose score exceeds CPPA’s threshold for assessment and further analysis.3,4,6,17 Details about the PARS intervention process and supporting feedback materials have been published and discussed elsewhere.3,6
Results
First, results of the planning phase are described in terms of the three major Project Bundle elements (Table 1) used to direct development efforts during the planning phase. Then we present outcomes achieved to date during PARS implementation.
People. The first important result of the planning phase occurred when highest level SHS leadership, Physician Board of Governors, and Board of Trustees signaled their commitment to the project by providing endorsements and support for PARS as a proactive risk reduction strategy. Then, at the end of the planning period, SHS made a financial commitment as well, signing a multi-year PARS implementation contract. The four SHS-affiliated co-authors (WH, DD, CB and RK) served throughout the planning process and initial PARS implementation as project champions, providing essential institutional memory and access to other leaders. SHS’s North- and South-centered geography required regional PARS peer messenger committees, Co-Chairs, and administrative point persons so each could take regional ownership. A single individual (DD) with system-wide responsibilities was appointed as a co-chair on both committees to coordinate training; facilitate safe, secure document distribution; review data; promote system-wide consistency; and serve as a focal point for questions or issues that arose throughout the process. SHS’s Medical Director for Clinical Services (CU) now serves those roles as the Medical Director for Sanford PARS.
Process. SHS's published values, goals, and codes of professional conduct aligned with PARS principles. In addition, results of the planning phase included SHS’s leadership adoption of the CPPA intervention model (Figure 1) and receipt of training in its implementation. Legal issues were far less straightforward. Significant planning was devoted to addressing legal issues, including messenger committee structure, State-to-State variations in Peer Review laws and protections, language to be included on PARS work products, safety-related professional legal language, and procedures to be taken when Level 1 “Awareness” interventions did not reduce patient complaints. A novel aspect of this project was development of a secure system by which peer messengers could share awareness intervention data electronically with a high-risk colleague who worked at a significant distance from the messenger, not uncommon within SHS.
Systems. Another key planning phase result was achieved when SHS’s OPRs and Information Technology (IT) teams expressed willingness to support PARS. While the SHS North and South flagship hospitals had reliable systems and dedicated staff for patient advocacy, SHS’s small‑town locations were just beginning in 2010 the work of adopting a unified process for systematically receiving and addressing patient concerns about their health care experiences. Therefore, CPPA provided training, “Getting the Most from Your Patient Relations Department and Service Recovery Program”19 to all SHS North and South OPR staff, focusing on best practices in complaint reporting and service recovery. Meetings supplemented with email and phone communications with SHS database managers and IT support personnel resulted in smooth, secure data transfer. As a result of the PARS planning process, SHS patient advocates now enter all patient comments in electronic complaint capture software.
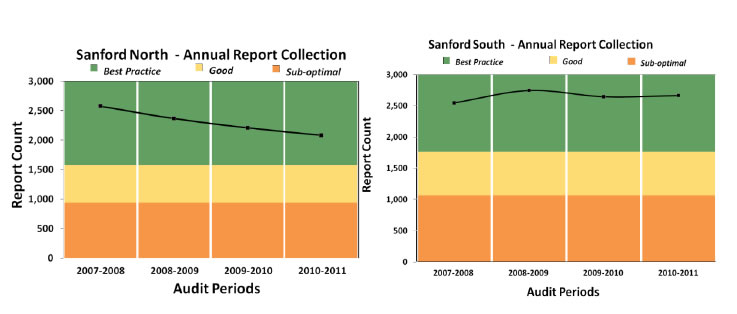
CPPA and SHS North and South OPR leaders collaborated on qualitative and quantitative assessments of complaint reports (e.g., includes clearly identifiable physicians, number of codable complaint(s), and needed attachments). One goal was an overall 80 percent rate of uniquely identified physicians associated with physician-related concerns (some patients simply do not recall which physician(s) they saw, and the physicians’ identities cannot be determined from a review of records). During the pre-launch planning period, SHS North had an 84 percent physician identification rate, and SHS South had a 77 percent rate, both of which were deemed sufficient for launching PARS. Each OPR has since achieved and exceeded the 80 percent goal. The second goal, to demonstrate sufficient complaint capture relative to organization size well in advance of PARS’ launch, was also achieved by 2011 during the planning phase project period (Figure 3). SHS complaint capture has continuously stayed well above each region’s Best Practice baseline through the 2016 intervention cycle.
Prior to being shared with high-risk physicians, PARS intervention data underwent multi-level reviews, including six quality checks by CPPA staff, faculty, and physicians, plus local reviews by SHS co-chairs and the assigned messenger physician.3,6 In order to move forward with an intervention, the co-chairs and messenger physicians must agree the data are sufficiently compelling that the high-risk colleague stands out from his or her peers. CPPA recommends and trains committee chairs not to pair messenger and recipient physicians with known conflicts of interest (e.g., direct competition for patients or resources), poor prior relationships, or a social relationship that makes the messenger role just too uncomfortable. Finally, 12 physicians from SHS South and 7 from SHS North completed CPPA’s PARS Messenger training, described elsewhere.3,6
Figure 3. Annual SHS Complaint Report Capture, June 2007–July 2011, plotted as a function of CPPA pre-PARS launch indicators of readiness
Patient Complaints and Risk Scores During the Implementation Phase. The first round of PARS Interventions occurred in both the North and South regions in October-November 2011. As of 2016 a total of 124 SHS physicians have received awareness interventions, including five currently receiving interventions guided by authority (Level 2 on the Promoting Professionalism Pyramid, Figure 1). Messengers’ fidelity to intervention elements exceeds 95 percent compliance. Overall, Risk Scores of physicians receiving interventions have declined 24 percent (p < 0.001). Sixty percent of the physicians have succeeded in substantially reducing their Risk Scores, 33 percent remain unimproved, and the rest (7 percent) have departed SHS (similar to physician turnover elsewhere). These results are similar to those achieved in other studies.3,5
SHS Return on Investment (ROI) in PARS. ROI evaluation compared SHS’s pre- and post‑PARS intervention paid claims and claims-related expenses. The analysis used dollars spent per insured physician pre- and post-PARS within the statute of limitations period, adjusting for time (CPI) and published statewide market experience.26,27 Based on CPPA research, 25 percent of any savings were attributed to PARS.4,6 The remainder was attributed to SHS’s other safety, quality, and risk prevention initiatives. PARS contract charges for the intervention period were then applied to calculate SHS’s system-wide ROI of 4 to 1. ROI remained positive when sensitivity analyses (e.g., 10 percent impact attributed to PARS) were conducted.
Discussion
This article presents a study of the planning process leading to successful initiation and ongoing implementation of the Vanderbilt CPPA PARS program in the Sanford Health System. Steps taken to increase the probability of PARS program success revolved around attention to key elements of a Project Bundle. These steps proved effective: Risk Scores declined for the majority of PARS intervention recipients, and the program’s positive ROI supports PARS’ sustainability.
The planners learned important lessons worth consideration before health care leaders launch PARS or other safety, quality, or risk prevention initiatives. The most important lessons are organized around the Project Bundle’s three major elements.
People-Related Lessons. Project planning and implementation required commitment of both titled leadership (e.g., CMOs, Department Chairs) and influential physicians whose opinions shape what really happens “on the ground.” These leaders must be willing to have the PARS process address every physician who appears to have a pattern of concerning behavior/performance, regardless of status or stature. Messenger committee members must be willing to deliver PARS data in a timely fashion, and all involved must be willing to give high risk professionals opportunities to self-correct in the earliest stages of intervention.
Process-Related Lessons. Organizational values must deem patients to be valuable health care team members. Partnership with Legal Affairs and Human Resources is essential to help craft and implement committees, policies, and procedures that provide peer review protections and fully align PARS within (and make PARS integral to) the organization. The organization must be willing to consistently and reliably implement the model of tiered interventions. Finally, the organization must be committed to employ the right number of Patient Relations Representatives and to invest in training in best practices for service recovery and documentation of patient/family complaints.
Systems-Related Lessons. Partnership with the Patient Relations teams and their database managers is essential, first for promoting institutional efforts to have a common, system-wide database. Patient Relations leaders need to receive regular feedback regarding best practices in complaint capture and narrative records so that high standards are sustained. Training for peer messengers must include practice delivering peer-comparative data and responding to recipients’ comments, questions, concerns, and emotions. In addition, there must be multi-level, regularly scheduled sharing of PARS progress and aggregated data to keep all levels of leadership aware of and up to date on the program to promote long-term implementation and sustainability.
Limitations. This study has limitations. First, SHS has unique characteristics as a large, multi‑State, multi-facility, predominantly rural health care provider, so generalizability is unknown. Nevertheless, one reason this study was conducted was to assess and demonstrate PARS’ viability in just such a system. SHS, like all PARS partner sites, was self-selected and thus is motivated to provide high quality patient experiences and mitigate risk exposure and thus is motivated to capture complaints and record service recovery activities.19 Second, we did not measure potential confounding physician characteristics (e.g., years in practice, clinical volume), aspects of the practice environment (e.g., local physician group characteristics) or patient characteristics (demographics, payer, and case mix) that may be associated with patient complaints and lawsuit risk.
The literature rightly directs much attention to systems issues but less to individual professional accountability. This study focused on use of the PARS tool for analysis of individual physicians’ relative risk. We acknowledge that promoting safety also requires attention to systems failures and team functioning. We would argue that all three—self- and group-regulation, support systems, and teamwork—are must-haves for a strong patient safety culture. While this study highlighted individual accountability, if PARS data reveal multiple high-risk members of a division, department, or location in a large system, that group’s risk may not be a function of the individual; it may instead signal systems and/or team issues. For example, patient complaints about surgeons’ communication and respectfulness have been shown to be related to surgical complications, which may indicate that similar behaviors toward colleagues may negatively impact high-complaint surgeons’ team functioning.28,29
Conclusion
This project resulted in the successful launch, implementation, and sustainability of the CPPA PARS program at SHS after the conclusion of the planning grant. The project demonstrated how in 1 year, a large multi-State health care system became prepared to implement an intervention process that promotes professional self-governance, fosters a fair and just culture of safety and kindness, and reduces avoidable lawsuit risk. By sustaining the PARS program, SHS has:
- A process for supporting fair, constructive, peer-delivered, evidence-based, peer-comparative self- and group regulation.
- Ongoing training for cohorts of "messengers."
- A tiered approach to addressing unnecessary variation in other domains.
- Consistent data monitoring that is applied to both rural and metropolitan sites.
- Reduced patient complaints about most physicians identified as high risk.
- A positive return on investment.
The results of this work have at least six implications. Our first conclusion is that the plan to assess, develop, and implement SHS’s PARS-related infrastructure could serve as a model for other large, multi-site institutions. Second, the Project Bundle tool provides leaders a useful heuristic for identifying and addressing pre-launch needs of other potential quality, safety, and/or risk prevention projects. Third, by attending to the Project Bundle’s elements, the SHS champions succeeded in demonstrating that potential pre-launch issues due to SHS’s size and complexity could be addressed and overcome, thus making the case for ongoing PARS program funding. SHS PARS implementation is now in its 6th year past the AHRQ-funded planning period and continues. Fourth, results on individual physicians receiving PARS interventions are positive and consistent with results achieved elsewhere, and fifth, the experience shows that a positive return on investment in PARS can be achieved in a geographically widespread health care system.
Finally, these findings have potential national significance. As U.S. medical centers continue to combine into major systems, the need for plans for promoting system-wide consistency in professionalism and professional self-regulation will expand. SHS and CPPA learned a great deal from this project, and we conclude that the experience can generalize to other dynamic health care systems, so long as the necessary people, processes, and systems are in place.
Acknowledgments
The planning phase of this project was supported by grant number HS19571 from the Agency for Healthcare Research and Quality. The authors gratefully acknowledge the SHS messengers, patient relations representatives, information technology team, risk managers, legal affairs department, grants officers, and administrators, and the many CPPA team members who participated throughout.
Author Affiliations
James W. Pichert, PhD, Professor of Medical Education and Administration, Center for Patient and Professional Advocacy (CPPA), CPPA Co-Founder, Vanderbilt University Medical Center and School of Medicine, Nashville, TN. Wendell W. Hoffman, MD, FACP, at the time of the planning project: Patient Safety Officer, Sanford Health, Sioux Falls Region, Sioux Falls, SD. David Danielson, JD, CPA, Assistant Professor, University of Nebraska Medical Center, Department of Ophthalmology and Visual Science, Department Administrator and Operations Director, Truhlsen Eye Institute, Nebraska Medicine, Omaha, NE (at the time of the planning project, Senior Vice President, Clinical Risk Management, Sanford Health System, Sioux Falls, SD). Cindy Baldwin, RN, MS, CNP, Executive Director, Clinical Risk and Regulatory Services, Sanford Health, Sioux Falls, SD. Craig J. Uthe, MD, AAFP, ASAM, Physician Director of Clinic Services, Executive Director of Leadership Development & Physician Well Being, Sanford PARS Medical Director, Sanford Health, Sioux Falls, SD. Meghan Goldammer, JD, RN, Senior Vice President Nursing and Clinical Services, Sanford Health Corporate Administration, Sanford Health, Sioux Falls, SD. Thomas F. Catron, PhD, CPPA Associate Director, Vanderbilt University Medical Center, Nashville, TN. Sue Garey, BA, CPPA Program Manager, Vanderbilt University Medical Center, Nashville, TN. Jan Karrass, MBA, PhD, CPPA Data/Research Manager, Vanderbilt University Medical Center, Nashville, TN. Margaret (Peggy) W. Westlake, MLS, at the time of the planning project: CPPA Research Coordinator, Vanderbilt University Medical Center, Nashville, TN. Rhonda Ketterling, MD, at the time of the planning project: Chief Medical Officer, Sanford Health Fargo Region, Fargo, ND. William O. Cooper, MD, MPH, CPPA Director, Associate Dean for Faculty Affairs, Vanderbilt University Medical Center, Nashville, TN. Gerald B. Hickson, MD, Sr. Vice President for Quality, Safety and Risk Prevention, Vanderbilt University Medical Center and School of Medicine, Nashville, TN.
Address correspondence to: James Pichert, PhD, Vanderbilt University Medical Center, 2135 Blakemore Avenue, Nashville, TN 37212; email Jim.Pichert@vanderbit.edu.
References
1. Pichert JW, Hickson GB. Patients as observers and reporters in support of systems and patient safety. In Barach PR, et al, eds. Pediatric and Congenital Cardiac Care, Vol. 2: Quality Improvement and Patient Safety. London: Springer-Verlag; 2015, pp. 165-84.
2. Hickson GB, Moore IN, Pichert JW, et al. Balancing systems and individual accountability in a safety culture. In: Berman S, ed. From Front Office to Front Line: Essential Issues for Healthcare Leaders. 2nd ed. Oakbrook Terrace, IL: Joint Commission Resources; 2012: pp. 1-36.
3. Pichert JW, Moore IN, Karrass J, et al. An intervention model that promotes accountability: peer messengers and patient/family complaints. Jt Comm J Qual Patient Saf 2013; 39:435-46.
4. Moore IN, Pichert JW, Hickson GB, et al. Rethinking peer review: detecting and addressing medical malpractice claims risk. Vanderbilt Law Rev 2006; 59:1175-1206.
5. Pichert JW, Hickson GB, Moore IN. Using patient complaints to promote patient safety: The Patient Advocacy Reporting System (PARS). In: Henriksen K, Battles JB, Keyes MA, et al., eds. Advances in Patient Safety: New Directions and Alternative Approaches. Bethesda, MD: Agency for Healthcare Research and Quality; 2008; Vol. 2, pp. 421-30.
6. Hickson GB, Pichert JW. Identifying and addressing physicians at high risk for medical malpractice claims. In: Youngberg B, ed. The Patient Safety Handbook, 2nd ed. Burlington, MA: Jones & Bartlett Learning. 2012; pp. 347–68.
7. Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA 2002; 287:2951-7.
8. Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk in a regional healthcare center. So Med J 2007; 100(8):791-6.
9. Hickson GB, Clayton EW, Githens PB, et al. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA 1992; 267:1359-63.
10. Hickson GB, Clayton EW, Entman SS, et al. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA 1994; 272(20):1583–7.
11. Stimson CJ, Pichert JW, Moore IN, et al. Medical malpractice claims risk in urology: an empirical analysis of patient complaint data. J Urol 2010; 183(5):1971-6.
12. Mukherjee K, Pichert JW, Cornett MB, et al. All trauma surgeons are not created equal: Asymmetric distribution of malpractice claims risk. J Trauma 2010 Sep; 69(3):549-54.
13 Kohanim S, Sternberg P Jr, Karrass J, et al. Unsolicited patient complaints in ophthalmology: An empirical analysis from a large national database. Ophthalmology 2016 Feb; 123(2):234-41.
14. Stimson CJ, et al. Academic urologic surgeons have greater exposure to risk management activity compared to community urologic surgeons: An empirical analysis of patient complaint data. Urology Practice, in press.
15. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med 2005; 118:1126-33.
16. Fullam F, Garman AN, Johnson TJ, et al. The use of patient satisfaction surveys and alternative coding procedures to predict malpractice risk. Med Care 2009; 47(5):553-9.
17. Cydulka RK, Tamayo-Sarver J, Gage A, et al. Association of patient satisfaction with complaints and risk management among emergency physicians. J Emerg Med 2011; 41: 405-11.
18. Levtzion-Korach O, Frankel A, Alcalai H, et al.: Integrating incident data from five reporting systems to assess patient safety: making sense of the elephant. Jt Comm J Qual Patient Saf 2010; 36:402-10.
19. Hayden AC, Pichert JW, Fawcett J, et al. Best practices for basic and advanced skills in service recovery: A case study of a re-admitted patient. Jt Comm J Qual Patient Saf 2010; 36(7):310–8.
20. Hickson GB, Pichert JW, Federspiel CF, et al. Development of an early identification and response model of malpractice prevention. Law and Contemporary Problems 1997; 60(1–2):7–29.
21. Hickson GB, Pichert, JW, Webb LE, et al. A complementary approach to promoting professionalism: Identifying, measuring, and addressing unprofessional behaviors. Acad Med 2007 Nov; 82(11):1040-8.
22. Webb LE, Dmochowski RR, Moore IN, et al. Using coworker observations to promote accountability for disrespectful and unsafe behaviors by physicians and advanced practice professionals, Jt Comm J Qual Patient Saf 2016 Apr; 42(4):149-64.
23. Talbot TR, Johnson JG, Fergus C, et al. Sustained improvement in hand hygiene adherence: Utilizing shared accountability and financial incentives. Infect Control Hosp Epidemiol 2013 Nov; 34(11):1129‑36.
24. Reiter CE, Hickson GB, Pichert JW. Addressing behavior and performance issues that threaten quality and patient safety: What your attorneys want you to know. Prog Pediatr Cardio 2012; 33(1):37–45.
25. Pichert JW, Johns JA, Hickson GB. Professionalism in support of pediatric cardio-thoracic surgery: A case of a bright young surgeon. Prog Pediatr Cardio 2011; 32(2):89–96.
26. Aon/ASHRM. 2014 Hospital and Physician Professional Liability: Benchmark Analysis. Chicago: Aon Risk Solutions; October 2015.
27. National Practitioner Data Bank. 2012 Annual Report. Washington, DC: Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions, Division of Practitioner Data Banks; February 2014. Accessed January 31, 2017.
28. Catron TF, Guillamondequi OD, Karrass J, et al. Patient complaints and adverse surgical outcomes. Am J Med Qual 2016; 31(5):415–22.
xxix. Murff HJ, France DJ, Blackford J, et al. Relationship between patient complaints and surgical complications. Qual Saf Health Care 2006; 15:13-6.



