Module 3: Best Practices in Fall Prevention—Slide Presentation
Slide 1: Best Practices in Fall Prevention
ADD Hospital Name Here
Module 3
Slide 2: Best Practices
- Best practices are those care processes—based on literature and expert opinion—that represent the best ways we currently know of preventing falls in the hospital.
AHRQ Patient Safety Network (PSNET)
https://psnet.ahrq.gov/
Image: Puzzle pieces are labeled “assess readiness,” “manage change,” “implement practices,” “best practices,” “measure,” “sustain,” and “tools.” The piece labeled “best practices” is highlighted in blue.
Slide 3: Module 3 Goals
- Identify and make decisions about:
- Which fall prevention practices to use.
- Which universal fall precautions to use.
- How a standardized assessment of fall risk factors should be conducted.
- How risk factors should be incorporated into care planning.
- How to assess and manage patients after a fall.
- How to incorporate these practices into a Fall Prevention Program.
Slide 4: Which Practices Should Be Used?
- Fall prevention practices are broken down into four separate activities:
- Universal fall precautions.
- Standardized assessment of fall risk factors.
- Care planning and interventions that address risk factors within an overall patient care plan.
- Analysis of post-fall procedures, including clinical review and huddles.
Slide 5: Tailoring Practices
The practices selected and used need to be tailored to your hospital and the type of patients and care flow on individual units.
Images: Three photographs show a medical provider holding the arm of upright patient, medical providers standing at a patient’s bedside, and a medical provider escorting a patient walking with IV pole.
Slide 6: Universal Fall Precautions
Slide 7: Universal Fall Precautions
- They apply to all patients.
- The purpose is to keep all patients safe.
- The choice of precautions varies by hospital.
- All staff who interact with patients should be trained on universal fall precautions.
Fall prevention becomes embedded into hospital safety culture.
Slide 8: Universal Fall Precautions
What are your hospital’s universal precautions?
Image: Photograph shows a patient lying in a hospital bed
Slide 9: Environmental Safety at the Bedside
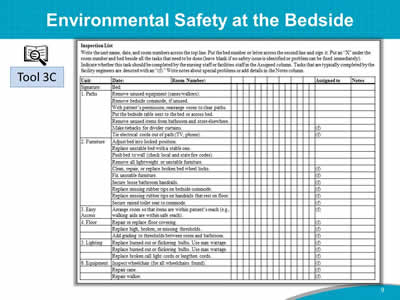
Images: A table is captioned Inspection List with the following instructions: "Write the unit name, date, and room numbers across the top line. Put the bed number or letter across the second line and sign it. Put an “X” under the room number and bed beside all the tasks that need to be done (leave blank if no safety issue is identified or problem can be fixed immediately). Indicate whether this task should be completed by the nursing staff or facilities staff in the Assigned column. Tasks that are typically completed by the facility engineers are denoted with an “(f).” Write notes about special problems or add details in the Notes column." An icon of a magnifying glass in front of open book identifies the table as Tool 3C.
Slide 10: Environmental Safety Hazard Report
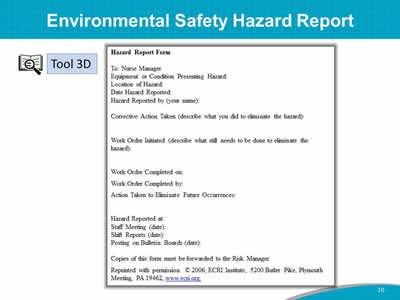
Images: A sample Environmental Safety Hazard Report is shown. An icon of a magnifying glass in front of open book identifies the report as Tool 3D.
Source: Reprinted with permission. © 2006, ECRI Institute, 5200 Butler Pike, Plymouth Meeting, PA 19462, www.ecri.org.
Slide 11: Purposeful Hourly Rounding

This is a strategy for fall precautions.
Image: Photograph shows a medical provider at a patient’s bedside
Slide 12: Scheduled Rounding Protocol
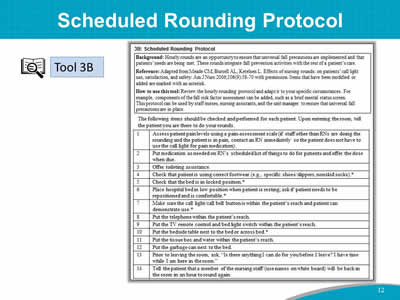
Images: A sample Scheduled Rounding Protocol is shown. An icon of a magnifying glass in front of open book identifies this as Tool 3B.
Reference: Adapted from Meade CM, Bursell AL, Ketelsen L. Effects of nursing rounds: on patients’ call light use, satisfaction, and safety. Am J Nurs 2006;106(9):58-70 with permission.
Slide 13: Fall Prevention Is a 3-Step Process
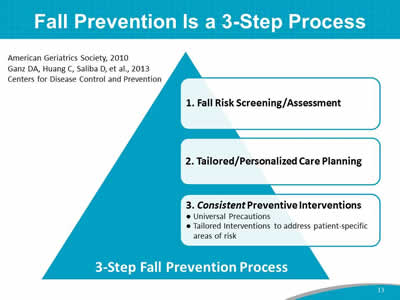
Image: A triangle represents the 3-Step Fall Prevention Process from top to bottom:
- Fall Risk Screening/Assessment.
- Tailored/Personalized Care Planning.
- Consistent Preventive Interventions:
- Universal Precautions.
- Tailored Interventions to address patient-specific areas of risk.
Source: American Geriatrics Society, 2010. Ganz DA, Huang C, Saliba D, et al., 2013. Centers for Disease Control and Prevention.
Slide 14: Fall Risk Assessment
Slide 15: Step 1: Fall Risk Screening/Assessment
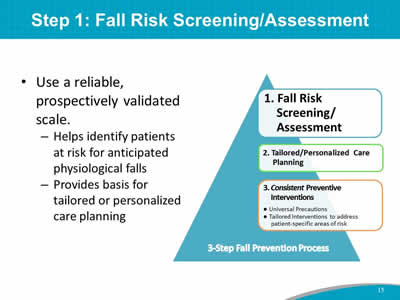
- Use a reliable, prospectively validated scale.
- Helps identify patients at risk for anticipated physiological falls.
- Provides basis for tailored or personalized care planning.
Image: A triangle represents the 3-Step Fall Prevention Process from top to bottom:
- Fall Risk Screening/Assessment.
- Tailored/Personalized Care Planning.
- Consistent Preventive Interventions:
- Universal Precautions.
- Tailored Interventions to address patient-specific areas of risk.
Slide 16: Standardized Assessment Tool
- Use a standard assessment tool throughout adult units.
- Add unit-level risk factors as needed.
- For example, on a geriatric psychiatry ward, orthostatic hypotension due to medications may be a fall risk factor.
- Refer to Tool 3F for evaluating orthostatic vital signs.
Image: Photograph shows a medical provider holding the arm of patient who sits at the edge of a bed with a mobility device
Slide 17: Key Factors To Assess for Fall Risk
- History of falls:
- All patients with a recent history of falls in the past 3 months should be considered at higher risk for future falls.
- Mobility problems and use of assistive devices:
- Patients who have problems with their gait, or who use a cane or walker, are more likely to fall.
Assess patients’ ability to use their assistive devices.
Image: Photograph shows a medical provider holding the arm of a patient walking with a mobility device.
Slide 18: Key Risk Factors for Falls
- Medications:
- Patients taking a large number of medications that could cause sedation, confusion, impaired balance, or orthostatic blood pressure changes are at higher risk for falls.
- Mental status:
- Patients with delirium, dementia, or psychosis may be agitated and confused, putting them at risk for falls.
Image: Photograph shows a patient taking medicine.
Slide 19: Key Risk Factors for Falls
- Continence:
- Patients who have urinary frequency, or who have frequent toileting needs, are at higher risk.
- Other risks:
- IV pole.
- Orthostatic hypotension.
- Oxygen tubing.
- Clutter in the patient’s room.
- Vision problems that cause patients to not see environmental hazards.
Slide 20: Role of Risk Factor Scores
- The most important use of an assessment tool is to identify fall risk factors for developing care plans.
- Excessive focus on a risk score is not recommended.
- In fact, research has shown that scores from fall risk prediction tools do not predict falls any better than a clinician’s judgment.
Image: An icon of a magnifying glass in front of open book refers to Page 36.
Slide 21: Fall Risk Assessment Tools
Tools to use:
- STRATIFY Scale.
- Morse Fall Scale.
- Medication Fall Risk Scale and Evaluation Tools.
- Delirium Evaluation Bundle.
Images: Icons of magnifying glasses in front of open books identify the tools listed above as Tool 3G, Tool 3H, Tool 3I, and Tool 3J, respectively.
Slide 22: Morse Fall Scale
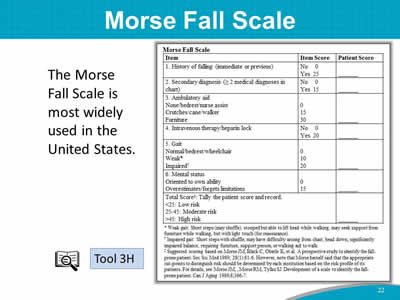
The Morse Fall Scale is most widely used in the United States.
Images: The Morse Fall Scale is shown. An icon of a magnifying glass in front of open book identifies this scale as Tool 3H.
Slide 23: Morse Fall Scale
- The Morse Fall Scale is made up of six subscales:
- History of falls.
- Secondary diagnosis.
- Ambulatory aid.
- IV/heparin lock.
- Gait.
- Mental status.
Slide 24: Case Study

- 45-year-old male with type 2 diabetes.
- Post-hip replacement.
- No recent history of falling.
- Difficulty walking due to hip pain.
- No ambulatory aid.
- No IV/heparin lock.
- Currently on pain medication, which makes him dizzy.
- Underestimates his limitations.
Slide 25: Case Study Risk Assessment
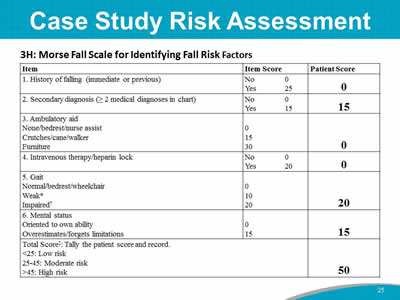
Images: The Morse Fall Scale is shown with sample patient scores.
Slide 26: Assessment of Risk Factors in Your Hospital
The questions for your Team to address are:
- Which tools will we use to assess fall risk in patients at our hospital?
- Do unit staff members understand why they are assessing fall risk factors?
Discussion:
- Which standardized fall risk assessment tool will you use?
Slide 27: Care Planning

Slide 28: Step 2: Tailored/Personalized Care Planning
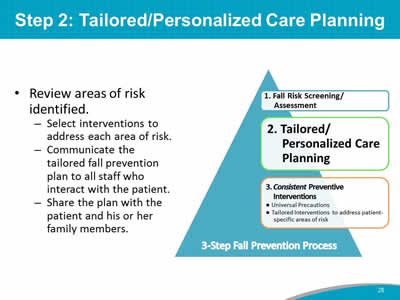
- Review areas of risk identified.
- Select interventions to address each area of risk.
- Communicate the tailored fall prevention plan to all staff who interact with the patient.
- Share the plan with the patient and his or her family members.
Image: A triangle represents the 3-Step Fall Prevention Process from top to bottom:
- Fall Risk Screening/Assessment.
- Tailored/Personalized Care Planning.
- Consistent Preventive Interventions:
- Universal Precautions.
- Tailored Interventions to address patient-specific areas of risk.
Slide 29: Fall Prevention Care Planning
- It is not enough to know which patients have risk factors for falls.
- Care planning guides staff on how to prevent falls.
- Care planning is a process whereby the patient’s risk information is translated into an Action Plan, ensuring continuity of care.
Image: Paper labeled “fall risk.”
Slide 30: Practice Insight
Care Plan Documentation
Image: Icon of binoculars.
Slide 31: Step 3: Consistent Preventive Interventions
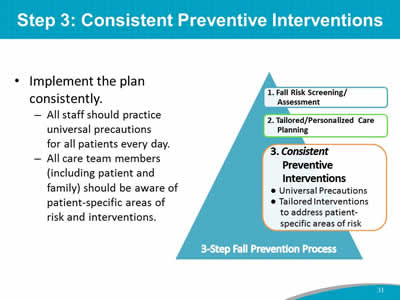
- Implement the plan consistently.
- All staff should practice universal precautions for all patients every day.
- All care team members (including patient and family) should be aware of patient-specific areas of risk and interventions.
Image: A triangle represents the 3-Step Fall Prevention Process from top to bottom:
- Fall Risk Screening/Assessment.
- Tailored/Personalized Care Planning.
- Consistent Preventive Interventions:
- Universal Precautions.
- Tailored Interventions to address patient-specific areas of risk.
Slide 32: Case Study – Engage Patient/Family
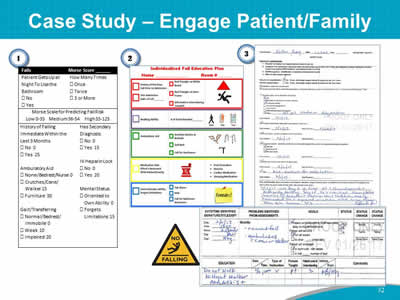
Images: 1. A sample patient checklist including Morse Scale scores for predicting fall risk. 2. Individualized Fall Education Plan. 3. Safety Plan, pages 1 and 2, and a “No falling” warning sign.
Slide 33: Sample Care Plan
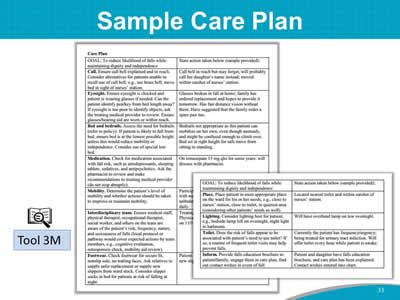
Images: Two pages of a Sample Care Plan are shown. An icon of a magnifying glass in front of open book identifies this as Tool 3M.
Slide 34: Care Plan Development
- An individualized care plan is developed for patients with any of the following:
- Patient has risk factors for falling (found on risk assessment form).
- Patient has fallen since admission.
- Patient’s attempts to walk alone result in unsteady/unsafe movements.
- Patients or relatives are anxious about falls.
Slide 35: Hospital Fall Prevention Care Plan – Comparison With Tool 3M
- Is the stated goal the same between the two plans?
- Are you happy with your stated goal?
- If not, how would you change it?
- Are the categories to be addressed in the care plan the same between your plan and Tool 3M?
- If not, would you consider adding any categories to your hospital’s plan?
- What other changes could be made to your hospital’s care plan?
Discussion:
- Do you need to revise or update your hospital’s care plan? If so, how?
Slide 36: Document and Communicate
- Use medical records and patient care worksheet documentation of risk factors.
- Communicate patient’s risk factors orally at shift change and medical rounds.
Image: Photograph shows medical providers using computers and papers for documentation.
Slide 37: Document and Communicate
- Safety huddles (safety briefing).
Image: Photograph shows medical providers holding a meeting. An icon of a magnifying glass in front of open book refers to Page 44.
Slide 38: Practice Insight
- Convene safety huddles at every shift change.
- Identify who fell and communicate prevention strategies.
- Identify top 3 patients at risk for falling on next shift.
Image: Photograph shows medical providers holding a meeting in a hospital corridor. Icon of binoculars.
Slide 39: Post-Fall Assessment
Slide 40: Assess and Manage Patients After a Fall
- Post-fall clinical review is a structured way to collect information after a fall.
- Carefully assess patients for any injuries in a systematic way. Document your findings in the medical record, and report the incident.
Image: Photograph shows a medical provider holding a patient's wrist with both hands.
Slide 41: Post-Fall Huddle: Essential Components
- A brief staff gathering, interdisciplinary when possible, that immediately follows a fall event.
- Convenes within 15 minutes of the fall event.
- Led by clinician(s) responsible for patient/resident during the fall event.
- Involves the patient/resident whenever possible in the environment where the patient/resident fell.
- Requires group discussion to learn what happened.
- Uses discovery to determine the root cause/immediate cause of the fall (why the patient/resident fell).
Slide 42: Outcomes of Post-Fall Huddles
- Specify root cause (proximal cause).
- Specify type of fall.
- Identify actions to prevent recurrence.
- Change plan of care.
- Involve patient/family in learning about the fall occurrence.
- Prevent repeat falls.
Slide 43: Decision Tree for Types of Falls
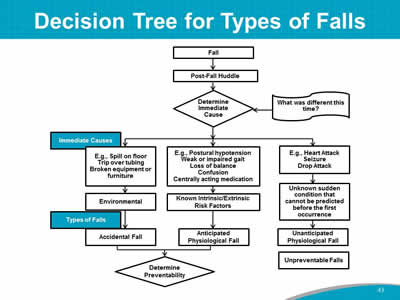
Image: A flow chart depicts a decision tree for types of falls.
Slide 44: Analysis of Huddles Shows Trends
- Preventable falls related to toileting:
- Notification.
- Observation.
- Falls related to environmental causes:
- Doorways.
- Shower stalls.
- Long bedspreads.
- Lunch and other breaks or shift handoff.
- Days of the week (barbershop/activities).
Slide 45: Post-Fall Assessment, Clinical Review
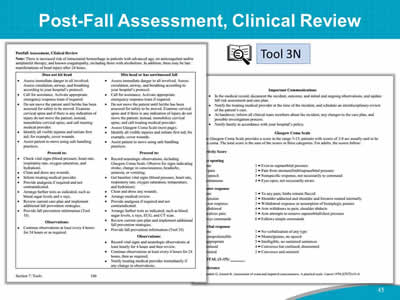
Images: Two screenshots show a sample post-fall assessment cliinical review. An icon of a magnifying glass in front of open book identifies this as Tool 3N.
Slide 46: Root Cause Analysis
- After an injurious fall, collect data to reconstruct the event and determine the causes of and contributing factors to the fall.
- Analysis of the data collection may help prevent the next fall in this patient or future patients.
- The analysis captures information from the patient, staff, and other witnesses about the fall.
- Refer to Tool 3O: Post-Fall Assessment for Root Cause Analysis.
Slide 47: Incorporate Best Practices
- Research evidence suggests that your program is more likely to succeed when it addresses multiple components:
- Risk factor assessment.
- Universal precautions.
- Care planning.
- Post-fall assessment.
- Some units (e.g., Rehab, Neurology, Pediatrics) may need customization.
Slide 48: Hospital Unit Fall Prevention Examples
- Geri-psych unit.
- Medical unit.
- Neurology and/or post-neurosurgical units.
- Inpatient rehab.
Image: Photograph shows a medical provider using gait belt on patient sitting on a bed. An icon of a magnifying glass in front of open book refers to Page 50.
Slide 49: Action Plan
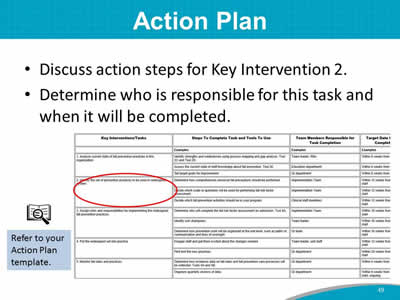
- Discuss action steps for Key Intervention 2.
- Determine who is responsible for this task and when it will be completed.
Images: A sample Action Plan is shown with Key Intervention 2 circled in red. An icon of a magnifying glass in front of open book sits above the text "Refer to your Action Plan template."
Slide 50: Summary
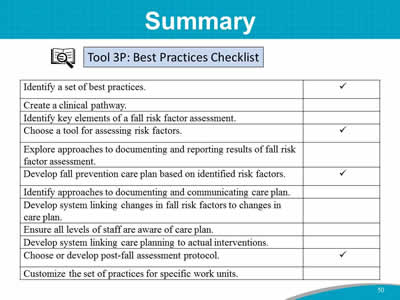
Image: A sample Best Practices checklist is shown in table form. The checklist items are:
- Identify a set of best practices.
- Create a clinical pathway.
- Identify ket elements of a fall risk factor assessment.
- Choose a tool for assessing risk factors.
- Explore approaches to documenting and reporting results of fall risk factor assessment.
- Develop fall prevention care plan based on identified risk factors.
- Identify approaches to documenting and communicating care plan.
- Develop system linking changes in fall risk factors to changes in care plan.
- Ensure all levels of staff are aware of care plan.
- Develop system linking care planning to actual interventions.
- Choose or develop post-fall assessment protocol.
- Customize the set of practices for specific work units.
An icon of a magnifying glass in front of open book identifies the checklist as Tool 3P.
Slide 51: References
- American Geriatrics Society. 2010 AGS/BGS Clinical Practice Guideline: Prevention of Falls in Older Persons. http://www.americangeriatrics.org/files/documents/health_care_pros/Falls.Summary.Guide.pdf. Accessed June 16, 2017.
- Centers for Disease Control and Prevention. STEADI - Older Adult Fall Prevention. http://www.cdc.gov/steadi/materials.html. Accessed June 16, 2017.
- Ganz DA, Huang C, Saliba D, et al. Preventing falls in hospitals: a toolkit for improving quality of care. Rockville, MD: Agency for Healthcare Research and Quality; January 2013. AHRQ Publication No. 13-0015-EF. http://www.ahrq.gov/sites/default/files/publications/files/fallpxtoolkit.pdf. Accessed June 16, 2017.



