Measure performance rates for all levels were calculated using state Medicaid administrative claims data. QMETRIC collaborators at the New York Department of Health provided measure performance rates using their own Medicaid administrative claims data.
One difficulty with using state administrative claims is the delay in data availability. Michigan Medicaid claims data become available approximately 6 months following the end of the year. As such, 2020 data was not available at the time of this writing.
Michigan and New York Medicaid Program
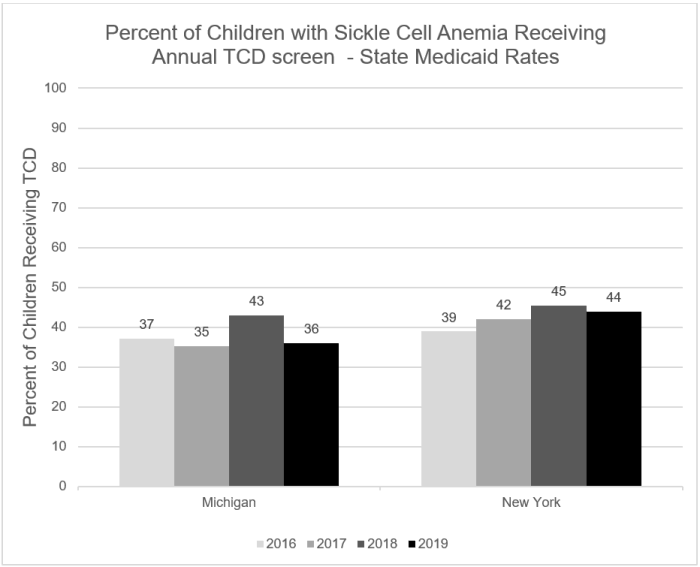
State Medicaid Rates
Both Michigan Medicaid and New York Medicaid performance rates improved slightly from 2016 through 2018, then decreased in 2019. Of note is the similarity in rates between the states over the four-year period.
Actions
The Michigan Medicaid Quality Improvement & Program Development Director and his team, in collaboration with the QMETRIC team, is establishing a pilot SCD Quality Improvement program. Through this unique and novel program, all Medicaid health plans with members having SCD within a specified region will be financially incentivized to improve measure performance for all SCD patients in the region. Incentives will be paid for improvement on a population-based (not plan-based) level. As such, plans will have to work together to achieve overall improvement in the region to receive the incentive payments. An SCD narrative report for health plans to use to report baseline SCA measure rates as well as current and future plans for improving care has been developed and is ready for implementation.
The State of New York is working separately from QMETRIC to address identified gaps in care.
Barriers
Baseline information was to be collected by the State from Michigan Medicaid health plans in the Spring, 2020. However, the COVID-19 pandemic necessarily created a reprioritization of this program. It is anticipated that the program will be piloted in the Summer, 2021.
Collaborating Medicaid Health Plans
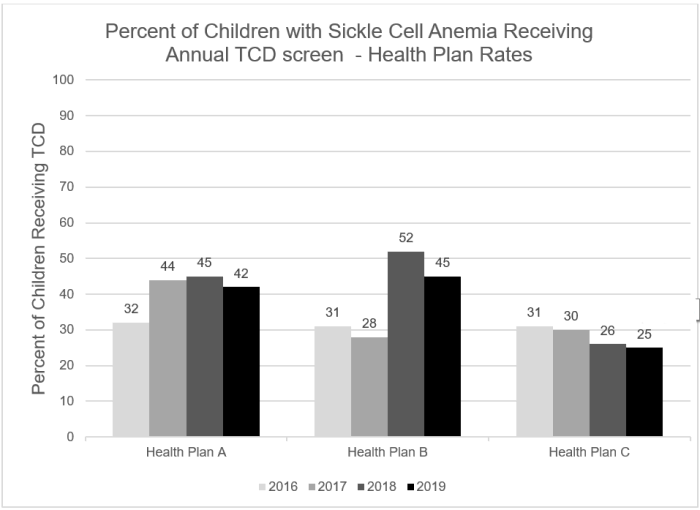
Rates
Similar to rates obtained at the State level, from 2016 through 2018, increases were seen in the performance rates for two collaborating health plans, Plan A and Plan B. Rates for all health plans decreased in 2019.
Actions
Although decreases were noted in 2019, increases in rates may be attributed, at least in part, to specific QMETRIC QI activities. The first QMETRIC SCD Expert Design (also referred to as the SCD Trailblazer) meeting occurred in December 2017.
A primary goal for this meeting was to increase the understanding among QMETRIC partners for the need for collaboration between care providers, health plans, and community organizations to ensure that each performs an effective role in the care for people living with SCD and their families. A Trailblazer small group call for care coordination and health plan relationship building took place in March 2018. In May 2018, regularly scheduled health plan huddles with the Q-METRIC QI team were established. QMETRIC then hosted another in-person Trailblazer meeting and follow-up call in June and July that focused specifically on health plan care management services. It is possible that the establishment of the Trailblazer group with in-person and virtual meetings were instrumental in improving rates in 2018 by encouraging health plans to focus some resources on children with SCD. It is also possible that Health Plan B had a greater proportion of its members in health system B (see below) and this could have accounted for its greater increase in performance.
In Oct. 2018, Health Plan A established an enhanced database for tracking its members with sickle cell disease and increased care management outreach services for these individuals. In early 2019, Health Plan B developed a sickle cell training program for members and providers. Other specific health plan activities included strengthening the outreach process, including additional calls to parents/providers, incorporating community health workers for door to door visits, educating health plan staff on SCD, and educate providers through provider network newsletters/meetings.
The QMETRIC team had hoped that with the focused efforts, 2019 rates for these two plans would further increase. However, as noted in the data, rates decreased in 2019.
Barriers
Health Plan C experienced staffing changes during 2018 which may have hampered an increased focus on this population and may have contributed to the lack of improvement. However, in 2019, this health plan hired an individual to specifically manage efforts for improving the care of its members with SCD.
Other barriers noted by collaborating health plans included high unable to reach rates and high member decline rate for care management services.
Collaborating Health Systems/Sickle Cell Clinics
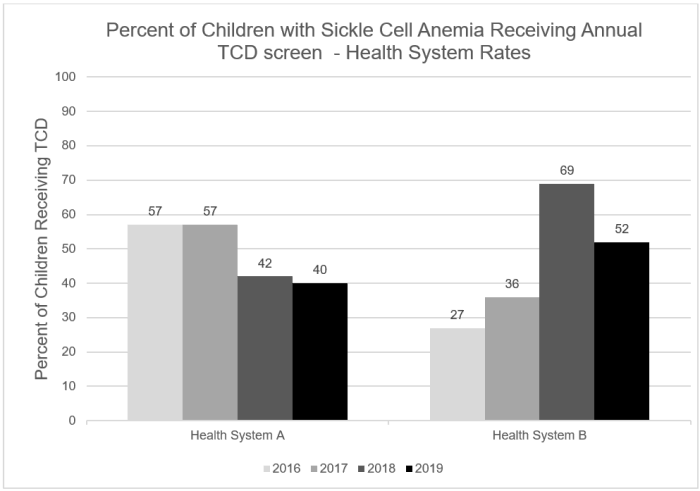
Rates
Over the four-year period, one of the two collaborating health systems demonstrated a significant increase in their performance rate, while the second health system rate declined. Again, one of the two collaborating health systems demonstrated a significant increase in their performance rate from 2016 through 2018, with a decline in 2019, while the second health system’s rate only declined during this period.
Actions
Health System B improved by 42% from 2016 through 2018. A likely contributing factor was that a new hematologist started working at this health system in November 2017. This individual was very committed to improving the care for individuals with SCD. In April 2018, baseline data for tracking TCDs on a master patient list was collected for a PDSA cycle. The PDSA ended in May, and the master patient list and tracking process was adopted. These two events likely are responsible for the significant increase in TCD screening in 2018. Reasons for the decline noted in 2019 are unknown.
Barriers
Health System A experienced staffing changes and shortages, specifically losing a key nursing position, which may have contributed to the lack of improvement at that site. Other identified barriers include difficulty in identifying patients that may be lost to follow-up and that are in need of an annual TCD screen, since it is possible that any given patient may have obtained care at another health system.



