The Problem of Pressure Ulcers
Each year, more than 2.5 million people in the United States develop pressure ulcers. These skin lesions bring pain, associated risk for serious infection, and increased health care utilization. Moreover, the Centers for Medicare & Medicaid (CMS) no longer provides additional reimbursement to hospitals to care for a patient who has acquired a pressure ulcer while under the hospital's care. Thus, pressure ulcer prevention presents an important challenge in acute care hospitals. A number of best practices have been shown to be effective in reducing the occurrence of pressure ulcers, but these practices are not used systematically in all hospitals.
The Challenges of Pressure Ulcer Prevention
Pressure ulcer prevention requires an interdisciplinary approach to care. Some parts of pressure ulcer prevention care are highly routinized, but care must also be tailored to the specific risk profile of each patient. No individual clinician working alone, regardless of how talented, can prevent all pressure ulcers from developing. Rather, pressure ulcer prevention requires activities among many individuals, including the multiple disciplines and multiple teams involved in developing and implementing the care plan. To accomplish this coordination, high-quality prevention requires an organizational culture and operational practices that promote teamwork and communication, as well as individual expertise. Therefore, improvement in pressure ulcer prevention calls for a system focus to make needed changes.
Toolkit Designed for Multiple Audiences
The aim of this toolkit is to assist hospital staff in implementing effective pressure ulcer prevention practices. The toolkit was developed under a contract with the Agency for Healthcare Research and Quality through the ACTION program (Accelerating Change and Transformation in Organizations and Networks), with additional support from the Health Services Research and Development Service of the Department of Veterans Affairs. It was created by a core team with expertise in pressure ulcers and organizational change at the Boston University School of Public Health. An expert advisory panel and quality improvement teams at six participating medical centers provided input.
The toolkit's content draws on literature on best practices in pressure ulcer prevention and includes both validated and newly developed tools. The toolkit was tested in the six participating medical centers. Their feedback influenced this final version and their experiences are reflected in many of the examples provided.
The toolkit is designed for multiple uses. The core document is an implementation guide organized under six major questions intended to be used primarily by the Implementation Team charged with leading the effort to plan and put the new prevention strategies into practice. Because the guide is too long to be read by everyone, the toolkit includes one-page pressure ulcer prevention implementation highlights to introduce the project to other key players, such as hospital senior management and unit nurse managers. This highlights tool can be found at the beginning of section 7 (Tool 0A, Introductory Executive Summary for Stakeholders).
The full guide also includes links to tools and resources found in the Tools and Resources section of the toolkit, on the Web, or in the literature. The tools and resources are designed to be used by different audiences and for different purposes, as indicated in the guide.
Implementation Guide Organized To Direct Hospitals Through the Change Process
To implement a successful initiative to improve pressure ulcer prevention on a sustained basis, your organization will need to address six questions:
- Are we ready for this change?
- How will we manage change?
- What are the best practices in pressure ulcer prevention that we want to use?
- How should those practices be organized in our hospital?
- How do we measure our pressure ulcer rates and practices?
- How do we sustain the redesigned prevention practices?
Sections of the Guide
These questions make up the major sections of the implementation guide. Each of these major questions is in turn organized by a series of more detailed questions to guide the Implementation Team through the improvement process, as summarized below in "What To Find in Each Section." Each section begins with a brief explanation of why the question is relevant and important to the change process or to pressure ulcer prevention. Each section concludes with action steps and specific resources to support the actions needed to address the questions.
Printer-friendly versions of all these tools and resources are compiled in section 7. Some resources are intended for the Implementation Team to use during the planning and system change process. Others are designed as educational materials or clinical tools to be used by unit staff as they implement the new strategies and use them on an ongoing routine basis. Sections also include references or links to more detailed resources for those who want to explore an issue in more detail.
Tailoring the Guide to Your Organization
While the implementation guide is designed to cover the full improvement process from deciding to make changes to monitoring sustainability, some sections may be more relevant than others if your organization has already begun the improvement process. Sections 1 and 2 are intended to guide you through an assessment of your readiness to change and plan your processes to change. Section 2 includes a tool to help you develop an action plan that will reflect the steps you need to take and a preliminary timeline for accomplishing them.
All the steps outlined here are important, but hospitals may have their own approaches in tailoring the toolkit to their needs. The guide can be used as a reference document with sections consulted selectively as needed. To aid you in finding the pieces you need, the questions that guide the full process are listed in "What To Find in Each Section" and the location of subjects can be found in the Key Subject Index.
Because the changes needed are usually complex, most organizations take at least a year to develop and incorporate the new pressure ulcer prevention practices. Some take longer as early accomplishments uncover the need and opportunity for further improvements. It will be important to balance the need to proceed thoughtfully with the need to move quickly enough to show progress and maintain momentum.
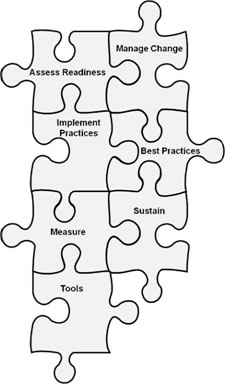
Improvement as Puzzle Pieces
It is important to recognize that the path through the guide is not a single sequence of steps. Instead, the sections can be better viewed as interlocking pieces of a puzzle, for two reasons. The components of improvement are not linear and independent: one piece may depend on another and work will need to move back and forth between them. Just as people approach puzzles differently, with some starting with the outside border and others starting in the center, both strategies can end with a completed puzzle.
We represent this view of the guide as a puzzle with the image below. To orient readers as you move through the guide, we repeat this image at the beginning of each section with the content of the section highlighted. In addition, throughout the guide, we explicitly cross-reference subsections where assessments, decisions, or tools in one area will contribute to deliberations or actions in another.
Throughout this toolkit, additional helpful materials are identified as follows:
| Action and Resource Symbols | |
|---|---|
|
|
Denotes action steps |
 |
Denotes a tool for this action in Tools and Resources |
 |
Denotes a linked tool or other resource for this action |
 |
Denotes practice insights |
 |
Denotes additional background material for those interested in pursuing this area in more detail |
What To Find in Each Section
1. Are we ready for this change?
1.1 Do organizational members understand why change is needed?
1.2 Is there urgency to change?
1.3 Does senior administrative leadership support this initiative?
1.4 Who will take ownership of this effort?
1.5 What kinds of resources are needed?
1.6 What if we are not ready?
1.7 Checklist for assessing readiness for change
2. How will we manage change?
2.1 How can we set up the Implementation Team for success?
2.2 What needs to change and how do we need to redesign it?
2.3 How should goals and plans for change be developed?
2.4 Checklist for managing change
3. What are the best practices in pressure ulcer prevention that we want to use?
3.1 What bundle of best practices do we use?
3.2 How should a comprehensive skin assessment be conducted?
3.3 How should a standardized pressure ulcer risk assessment be conducted?
3.4 How should pressure ulcer care planning based on identified risk be used?
3.5 What items should be in our bundle?
3.6 What additional resources are available to identify best practices for pressure ulcer prevention?
3.7 Checklist for best practices
4. How do we implement best practices in our organization?
4.1 What roles and responsibilities will staff have in preventing pressure ulcers?
4.2 What pressure ulcer practices go beyond the unit?
4.3 How do we put the new practices into operation?
4.4 Checklist for implementing best practices
5. How do we measure our pressure ulcer rates and practices?
5.1 Measuring pressure ulcer rates
5.2 Measuring key processes of care
5.3 Checklist for measuring progress
6. How do we sustain the redesigned prevention practices?
6.1 Who will be responsible for sustaining active pressure ulcer prevention efforts on an ongoing basis?
6.2 What types of ongoing organizational support do we need to keep the new practices in place?
6.3 How can we reinforce the desired results?
6.4 Summary and plan for moving forward
7. Tools and Resources




