The Emergency Department & Catheter Insertions
Slide Presentation
Slide 1
The Emergency Department & Catheter Insertions
Mohamad Fakih, MD, MPH
St. John Hospital and Medical Center
Lisa Wolf, PhD, RN, CEN, FAEN
Emergency Nurses Association (ENA)
Jeremiah Schuur, MD, MHS, FACEP
Brigham and Women’s
Department of Emergency Medicine
Images: Photos of the three presenters.
Slide 2
Learning Objectives
- List 3 ways to improve compliance with the appropriate indications for urinary catheter placement in the emergency department
- Discuss strategies to improve compliance with proper technique for urinary catheter placement
- Summarize the ED physicians’ role in urinary catheter placement
Slide 3
Could this happen at your hospital? The Story of Mr. Smith (1)
- Mr. Smith is 82 year old and gets admitted because of mild congestive heart failure. In the Emergency Department, a urinary catheter is placed (although he can use the urinal), and he is transferred to the floor but could not sleep. He is prescribed a sleeping pill. He gets more restless, gets out of bed, trips on the catheter and falls. He is found to have a left hip fracture, and undergoes surgery. Post-operatively, the staff notes that his left leg is swollen and he is diagnosed with deep venous thrombosis. He is started on blood thinners.
Slide 4
Could this happen at your hospital? The Story of Mr. Smith (2)
- Because of his immobility, he develops a pressure ulcer on his sacrum. His physician removes the catheter, but now he is having urinary retention related to pain medications. The urinary catheter is placed again. The procedure results in hematuria with the difficulty in insertion and being on blood thinners. Few days later, he develops fever and his blood pressure drops. Blood cultures and urine cultures grow Escherichia coli and he is diagnosed with CAUTI and septicemia. After 6 weeks in the hospital and many complications, Mr. Smith is no longer the same.
Slide 5
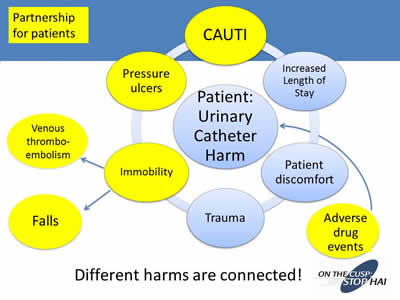
Different harms are connected!
Image: Depiction of how different harms are connected. Patient, with Urinary Catheter Harm is in the middle, with several issues surrounding it (i.e. immobility, CAUTI, pressure ulcers), that could lead to Falls and VTE.
Slide 6
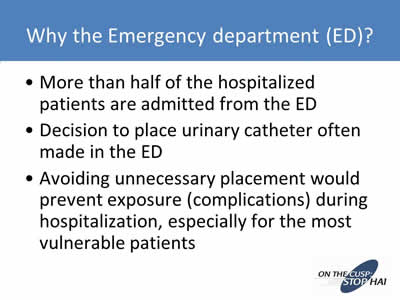
Why the Emergency Department (ED)?
- More than half of the hospitalized patients are admitted from the ED
- Decision to place urinary catheter often made in the ED
- Avoiding unnecessary placement would prevent exposure (complications) during hospitalization, especially for the most vulnerable patients
Slide 7
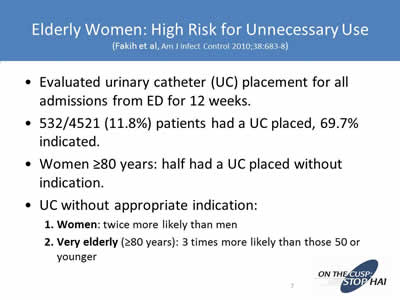
Elderly Women: High Risk for Unnecessary Use
(Fakih et al, Am J Infect Control 2010;38:683-8)
- Evaluated urinary catheter (UC) placement for all admissions from ED for 12 weeks.
- 532/4521 (11.8%) patients had a UC placed, 69.7% indicated.
- Women ≥80 years: half had a UC placed without indication.
- UC without appropriate indication:
- Women: twice more likely than men.
- Very elderly (≥80 years): 3 times more likely than those 50 or younger.
Slide 8
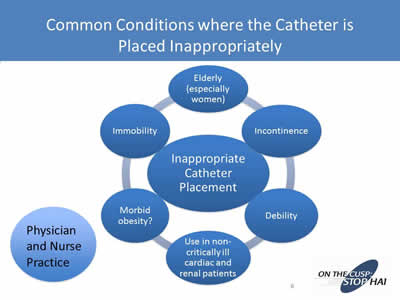
Common Conditions where the Catheter is Placed Inappropriately
Image: Diagram representing the relationship between inappropriate UC use and its common conditions. Physician and nurse practice influences this relationship greatly. Inappropriate conditions include: Elderly (especially women), Incontinence, Debility, Use in non-critically ill cardiac and renal patients, Morbid obesity and Immobility.
Slide 9
Effect of Establishing Institutional Guidelines in ED
(Fakih et al, Acad Emerg Med 2010; 17:337–340)
- Established institutional guidelines for UC placement in ED
- Compared the rate of placement before and after guidelines
- ED physician champion involved
- Minimal nursing education/ intervention
- Pre- and post-intervention: 3 months baseline, and 9 months intervention/ sustainability (sampled 5 days per quarter)
Slide 10

Physician Intervention ED
(Fakih et al, Acad Emerg Med, 2010; 17:337–340)
- UC utilization dropped significantly after starting the physician intervention from 14.9% pre-intervention to 10.6% post-intervention (p=0.002)
- Physicians ordered fewer UCs post-intervention 4.3% compared to pre-intervention 7.5% (p=0.002)
- Only 47.0% UCs initially placed in the ED had a physician order documented
- Post-intervention: more compliance with indications for catheters placed with physician order, no change for those without
Slide 11
Pilot Work: Ascension and Michigan Hospital Association
- More than 30 EDs involved
- Engaged both ED physicians and nurses
- Encouraged establishing institutional guidelines
- Looked at change in placement rate and appropriateness
Slide 12
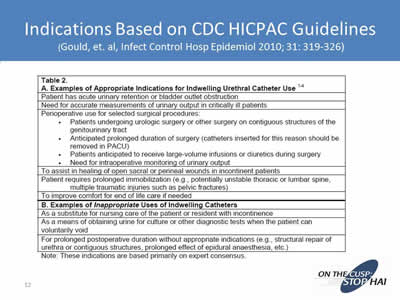
Indications Based on CDC HICPAC Guidelines
(Gould, et. al, Infect Control Hosp Epidemiol 2010; 31: 319-326)
Image: Screen shot from paper showing examples of appropriate and inappropriate indications for indwelling catheter use.
Slide 13
Pilot Work: 18 EDs in Ascension Health
- Results: less catheters placed, in some instances up to 50% drop, average about a third, and increased appropriateness of use
- Physician order documentation for placement increased
- More noticeable improvement in hospitals who started with a higher baseline use
Slide 14
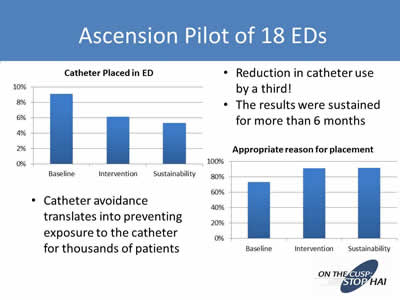
Ascension Pilot of 18 EDs
Image: Bar chart titled "Catheter Placed in ED". Baseline level is 9%; Intervention level is 6%, and Sustainability level is 5%.
- Catheter avoidance translates into preventing exposure to the catheter for thousands of patients.
Image: Bar chart titled: "Appropriate reason for plcement". Baseline level is 70%; Intervention level is 90%; and Sustainability level is 92%.
- Reduction in catheter use by a third!
- The results were sustained for more than 6 months
Slide 15
How to Improve Appropriate Urinary Catheter (UC) Use in the ED?
- Establish clear guidelines for UC insertion in the ED.
- Engage nurses (significant role in UC use).
- Engage physicians (significant role in UC use).
Slide 16
Nursing Considerations in the Emergency Department
Lisa Wolf, PhD, RN, CEN, FAEN
Image: Photo of Lisa Wolf.
Slide 17
Problem
- The emergency nurse at both the initial patient encounter and throughout the trajectory of care makes clinical decisions that affect patient safety, efficacy, efficiency and cost-effectiveness of care involving:
- Problem identification
- Acuity assignation
- Need for resources
- Patient advocacy
Image: Cartoon showing confused nurse holding a patient chart and a hypodermic needle.
Slide 18
Problem
- Clinical decision-making takes place in a social context.
- The attitudes and biases of each participant can affect the decision-making process.
- The overall culture of an emergency department can challenge or enhance good clinical decision-making.
Slide 19
Who is driving patient care in emergency settings?
- Nurses?
- Physicians?
- Hospitalists?
- Intensivists?
- Patients?
Slide 20

What’s different about ED nursing?
- Rapidly shifting priorities
- Quick turnover of patients
- Chaotic environment
- Potential for rapid deterioration of patients
- Range of ages/developmental stages
- Unclear diagnosis/etiology of symptoms
Slide 21
EDs as a unique setting
- Higher levels of autonomous practice
- Nurse-driven environment
- Use of protocols/care guidelines
- Collaborative practice
Slide 22
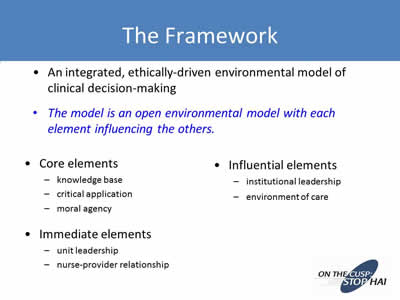
The Framework
- An integrated, ethically-driven environmental model of clinical decision-making.
- The model is an open environmental model with each element influencing the others.
- Core elements:
- Knowledge base
- Critical application
- Moral agency
- Immediate elements:
- Unit leadership
- Nurse-provider relationship
- Influential elements:
- Institutional leadership
- Environment of care
Slide 23
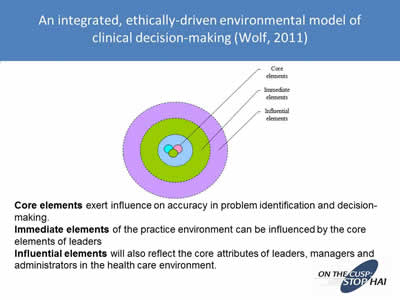
An integrated, ethically-driven environmental model of clinical decision-making (Wolf, 2011)
Core elements exert influence on accuracy in problem identification and decision-making.
Immediate elements of the practice environment can be influenced by the core elements of leaders.
Influential elements will also reflect the core attributes of leaders, managers and administrators in the health care environment.
Image: Ring with three concentric circles. The inner ring has a Venn diagram with three intersecting circles. The circles are labeled Core elements, Immediate elements, and Influential elements.
Slide 24
Elements of the individual
- Knowledge base – what does the provider know?
- Moral reasoning – what drives questioning and assessment?
- Drive to act – able to operationalize moral agency?
Slide 25
What are the elements in the environment?
- Environmental structure:
- Standards – what is expected of each level of provider?
- Communication – how does information and concern get transmitted between providers?
- Teamwork – are all providers working with the same agenda and goals?
- Autonomy of practice – who is able to make decisions about acuity and resources and under what circumstances?
Slide 26
Fostering excellence in clinical decision-making
- Needs to address all aspects of the model:
- Individual:
- Knowledge and critical application
- Moral agency
- Drive to act
- Environmental:
- Context in which decision making occurs and is acted upon:
- Unit level
- Institutional level
- Context in which decision making occurs and is acted upon:
- Individual:
Slide 27
Urinary Catheter Utilization
- About 15-25% of patients will have a urinary catheter placed during their hospitalization.
- Many are placed in:
- ICU
- ED
- OR
Slide 28
Reducing CAUTI
- Avoid use if no indication
- Remove as soon as possible
Slide 29
Why we think putting in a catheter is a good idea – but it’s not
- Facilitates I/O measurement.
- Keeps patients from having to get up to urinate, protecting them from injury.
- Protects skin in the incontinent patient.
- Saves time for the bedside nurse.
Slide 30
Indications for catheterization
- Patient is critically ill and will require accurate output measurement
- Urinary retention/obstruction:
- Bladder scanner or bedside ultrasound first
- Immobilization needed for trauma or surgery
- Incontinent with open sacral/perineal wounds
- End of life/hospice
- Chronic or existing catheter use:
- Re-evaluate need and discuss with provider:
- HCPAC Guidelines
- Re-evaluate need and discuss with provider:
Slide 31
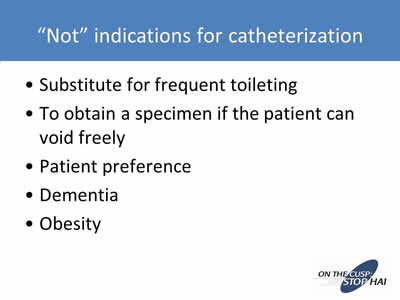
“Not” indications for catheterization
- Substitute for frequent toileting
- To obtain a specimen if the patient can void freely
- Patient preference
- Dementia
- Obesity
Slide 32
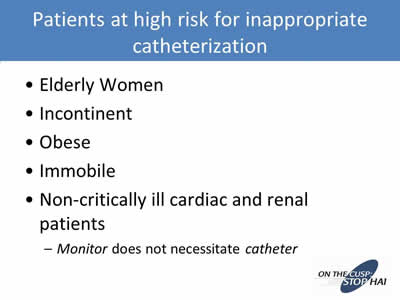
Patients at high risk for inappropriate catheterization
- Elderly Women
- Incontinent
- Obese
- Immobile
- Non-critically ill cardiac and renal patients:
- Monitor does not necessitate catheter
Slide 33
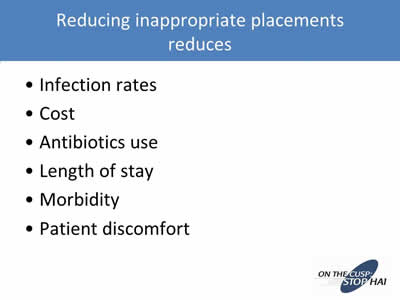
Reducing inappropriate placements reduces
- Infection rates
- Cost
- Antibiotics use
- Length of stay
- Morbidity
- Patient discomfort
Slide 34
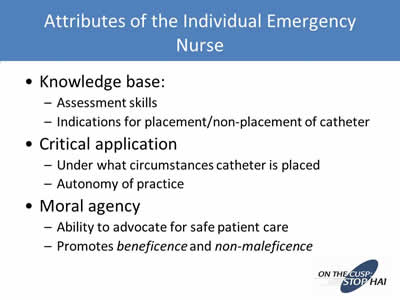
Attributes of the Individual Emergency Nurse
- Knowledge base:
- Assessment skills
- Indications for placement/non-placement of catheter
- Critical application:
- Under what circumstances catheter is placed
- Autonomy of practice
- Moral agency:
- Ability to advocate for safe patient care
- Promotes beneficence and non-maleficence
Slide 35
Putting systems in place
- Environmental: Context in which decision making occurs and is acted upon
- Unit Leadership:
- Must set standards of practice
- Must maintain ‘sunnum bonum’ for patients
- Must promote collaborative clinical decision-making and care
Slide 36
Nurse-Provider relationships and communication
- Central to decision-making and action
- Assess for mutual respect and autonomy of practice
- Institutional level – foster teamwork, autonomy and control over practice:
- Ethical standards drive practice
- Interdisciplinary training, governance, practice committees
Slide 37
Communication with Providers
- Clear understanding of indications
- Commitment to nonmaleficence (doing no harm)
- Patient focused care
Slide 38
Implications
- Environment:
- In settings with problematic decision-making or change process implementation, the attributes of the practice environment should be examined and managed as well as the skill level of individual nurses who practice in that environment:
- Administrative support
- Nurse-physician relationships
- Practice culture
- In settings with problematic decision-making or change process implementation, the attributes of the practice environment should be examined and managed as well as the skill level of individual nurses who practice in that environment:
Slide 39
The take home
- Clinical decision-making is not a matter of information in, decision out
- Elements that encompass both characteristics of the individual as well as the context in which the individual functions are crucial to fostering excellence in decision-making
Slide 40
The take home
- Commitment at the unit and institutional levels is required to support and facilitate excellence.
- Both physicians and nurses need to model ethically-driven, patient focused, collaborative care.
- The environment of care must change to afford behavioral change.
Slide 41
ED Physician Champions for CAUTI
Jeremiah D. Schuur MD, MHS, FACEP
Image: Photo of Dr. Schuur
Slide 42
Objectives
- Review ED physicians’ role in urinary catheter placement
- Identify strategies for improving appropriateness
- Review role of physician champion in CAUTI project
Slide 43
Physician Role in Urinary Catheter Placement
- All urinary catheters require an order…
- Yet, the decision to place a catheter is not the ED ordering provider’s alone:
- ED nurse
- Patient & Family
- Consultant (e.g. Trauma)
- Admitting service (e.g. Cardiology)
Slide 44
ED Workflow and Culture & Urinary Catheter Placement
- ED workflow requires physicians and nurses to work in parallel
- Nurses often assess a patient and consider a catheter before the ordering provider
- Patterns of ED catheter use have developed over time and reflect local practice patterns
- It will take teamwork from physicians, nurses and others to reduce catheter use
Slide 45
Role of ED Physician Champion to Reduce CAUTI
- Promote reduction of catheter use by championing appropriateness
- Encourage interdisciplinary conversation around catheter use
- Engage with other services around patterns of catheter use
Slide 46
Improving Appropriateness
- Review appropriate indications for catheters with medical staff:
- CDC/HICPIC Guidelines
- Pathway
- Implement appropriateness criteria in workflow:
- Ordering process: Computer physician order entry or Paper order sets
- Pathway
- Give feedback to medical staff on catheter appropriateness
Slide 47
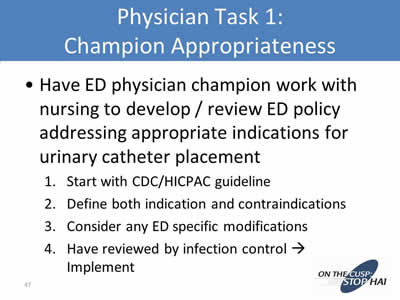
Physician Task 1: Champion Appropriateness
- Have ED physician champion work with nursing to develop / review ED policy addressing appropriate indications for urinary catheter placement:
- Start with CDC/HICPAC guideline
- Define both indication and contraindications
- Consider any ED specific modifications
- Have reviewed by infection control → Implement
Slide 48
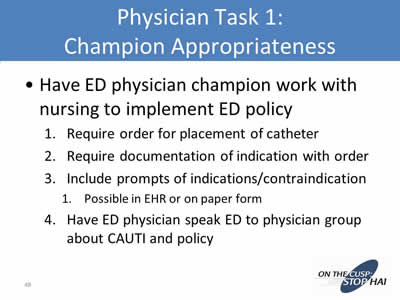
Physician Task 1: Champion Appropriateness
- Have ED physician champion work with nursing to implement ED policy:
- Require order for placement of catheter
- Require documentation of indication with order
- Include prompts of indications/contraindication:
- Possible in EHR or on paper form
- Have ED physician speak ED to physician group about CAUTI and policy
Slide 49
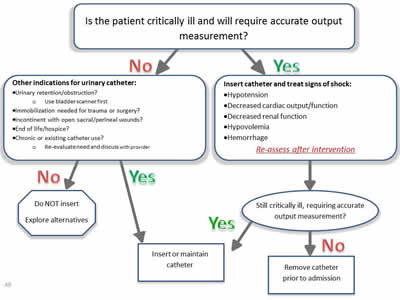
Image: Flowchart showing an evidence-based algorithm for use of urinary catheters in the emergency department is as follows. First ask whether the patient is critically ill and will require accurate output measurement. If not, then ask whether other indications for a urinary catheter exist.
- Is there urinary retention or obstruction? (If so, use a bladder scanner first.)
- Is immobilization needed for trauma or surgery?
- Is the patient incontinent with open sacral or perineal wounds?
- Is the patient in end-of-life or hospice care?
- Is there chronic or existing catheter use? (If so, re-evaluate need and discuss this with the care provider.)
If none of these indications exist, DO NOT insert a catheter, and explore alternatives. If at least one of these indications does exist, then insert or maintain the catheter.
If the patient is critically ill and will require accurate output measurement, then insert a urinary catheter and treat signs of shock, such as hypotension, decreased cardiac output/function, decreased renal function, hypovolemia, or hemorrhage. Then, re-assess after intervention. If the patient is still critically ill, requiring accurate output measurement, then place or maintain the urinary catheter. If not, then remove the catheter prior to admission.
Slide 50
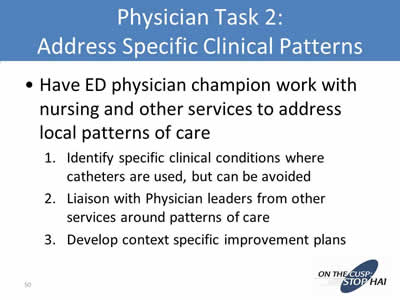
Physician Task 2: Address Specific Clinical Patterns
- Have ED physician champion work with nursing and other services to address local patterns of care:
- Identify specific clinical conditions where catheters are used, but can be avoided
- Liaison with Physician leaders from other services around patterns of care
- Develop context specific improvement plans
Slide 51
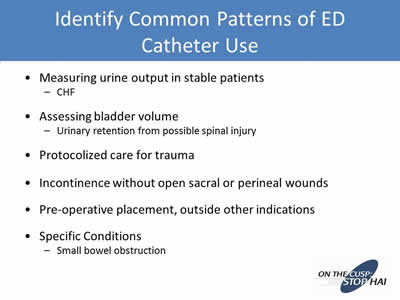
Identify Common Patterns of ED Catheter Use
- Measuring urine output in stable patients
- CHF
- Assessing bladder volume:
- Urinary retention from possible spinal injury
- Protocolized care for trauma
- Incontinence without open sacral or perineal wounds
- Pre-operative placement, outside other indications
- Specific Conditions:
- Small bowel obstruction
Slide 52
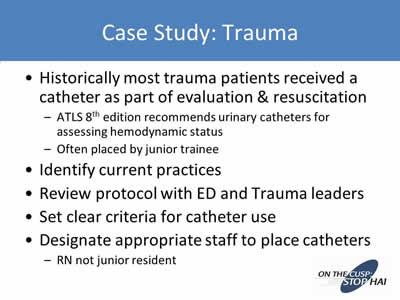
Case Study: Trauma
- Historically most trauma patients received a catheter as part of evaluation & resuscitation:
- ATLS 8th edition recommends urinary catheters for assessing hemodynamic status
- Often placed by junior trainee
- Identify current practices
- Review protocol with ED and Trauma leaders
- Set clear criteria for catheter use
- Designate appropriate staff to place catheters
- RN not junior resident
Slide 53
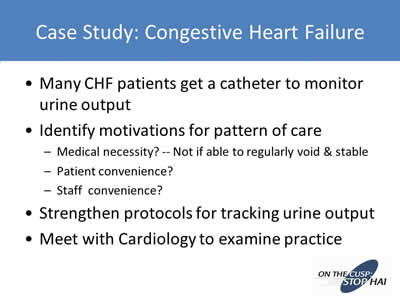
Case Study: Congestive Heart Failure
- Many CHF patients get a catheter to monitor urine output
- Identify motivations for pattern of care:
- Medical necessity? -- Not if able to regularly void & stable
- Patient convenience?
- Staff convenience?
- Strengthen protocols for tracking urine output
- Meet with Cardiology to examine practice
Slide 54
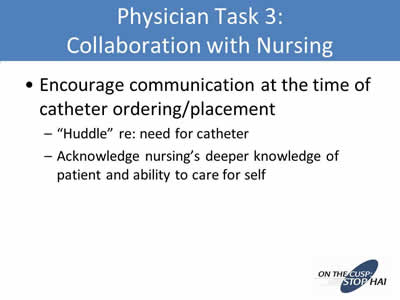
Physician Task 3: Collaboration with Nursing
- Encourage communication at the time of catheter ordering/placement:
- Huddle” re: need for catheter
- Acknowledge nursing’s deeper knowledge of patient and ability to care for self
Slide 55
Ongoing Physician Champion Roles
- Share data on catheter use with medical staff:
- Break out by physician if possible
- Circulate descriptive summaries of any CAUTI cases that are attributed to ED placement
- Communicate with other medical services about specific patterns of care
Slide 56
Thank you!
Questions?
Slide 57
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”



