Infectious Complications Related to the Catheter Other Than CAUTI
Slide Presentation
Slide 1
Infectious Complications Related to the Catheter Other than CAUTI
Mohamad Fakih, MD, MPH
Medical Director, Infection Prevention and Control
St. John Hospital and Medical Center
Professor of Medicine
Wayne State University School of Medicine
Detroit, MI
Nasia Safdar, MD, PhD
Associate Professor, Infectious Disease Division
University of Wisconsin, Madison
Hospital Epidemiologist
University of Wisconsin Hospital and Clinics
Kathlyn Fletcher, MD, PhD
Associate Professor of Medicine
Medical College of Wisconsin and the Milwaukee VAMC
Associate Program Director, MCW Internal Medicine Residency
Images: Photos of the 3 presenters.
Slide 2
Learning Objectives
- Describe patients with urinary catheters as potential reservoirs for transmission of multidrug resistant organisms
- Discuss the impact of unnecessary antibiotic use in causing C. difficile infection
- Summarize the role of unit culture on prevention of CAUTI
Slide 3
Polling Question 1: Which of the following is more likely in patients with urinary catheters? (choose one)
- Patient developing symptomatic CAUTI
- Patient being given inappropriate antibiotics for asymptomatic bacteriuria
- Patient developing bacteremia from a urinary source
Slide 4
Patients with Urinary Catheters…
- Catheter associated bacteriuria often misdiagnosed as CAUTI (Cope, Clin Infect Dis 2009; 48:1182–8; Al-Qas Hanna Am J Infect Control 2013; 41: 1173-7)
- Clinicians administer antibiotics even to patients with history of Clostridium difficile infection (Shaughnessy, Infect Control Hosp Epidemiol 2013;34(2):109-116)
- Bacteremia related to urinary tract: <4% of patients with bacteriuria
Slide 5
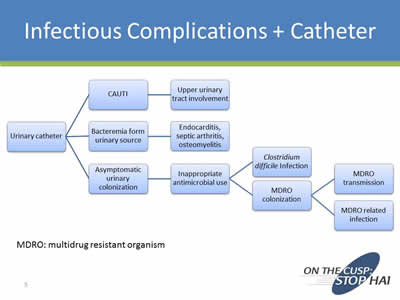
Infectious Complications + Catheter
Image: Flowchart showing possible complications from inserting a catheter.
Slide 6
Risk
- Patient with indwelling catheter and colonized urine:
- Healthcare worker exposes other patients
- Organisms contaminate environment and may survive for months
- Shared instruments (fomites) expose other patients
- Unnecessary antibiotics and their side effects, risks for MDRO, and Clostridium difficile
Solution: minimize catheter exposure, avoid unnecessary cultures, and promote appropriate antimicrobial use
Image: 2 large arrows on left side of slide. Top arrow points up and says Increased Risk. Bottom arrow points down and says Reduced Risk.
Slide 7
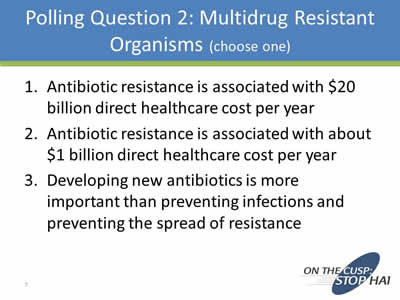
Polling Question 2: Multidrug Resistant Organisms (choose one)
- Antibiotic resistance is associated with $20 billion direct healthcare cost per year
- Antibiotic resistance is associated with about $1 billion direct healthcare cost per year
- Developing new antibiotics is more important than preventing infections and preventing the spread of resistance
Slide 8
4 Core Actions to Fight Deadly Infections
(CDC; Antibiotic Resistance Threats, 2013)
- Preventing infections and preventing the spread of resistance
- Tracking resistant bacteria
- Improving the use of today’s antibiotics
- Promoting the development of new antibiotics and developing new diagnostic tests for resistant bacteria
Slide 9
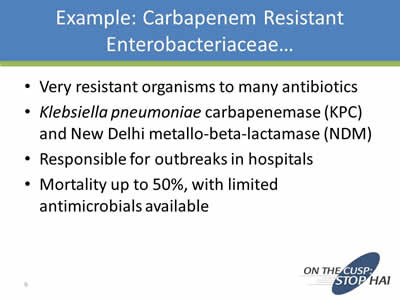
Example: Carbapenem Resistant Enterobacteriaceae…
- Very resistant organisms to many antibiotics
- Klebsiella pneumoniae carbapenemase (KPC) and New Delhi metallo-beta-lactamase (NDM)
- Responsible for outbreaks in hospitals
- Mortality up to 50%, with limited antimicrobials available
Slide 10
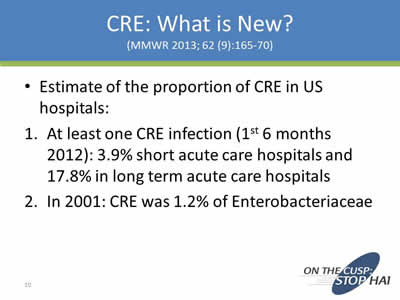
CRE: What is New?
(MMWR 2013; 62 (9):165-70)
- Estimate of the proportion of CRE in US hospitals:
- At least one CRE infection (1st 6 months 2012): 3.9% short acute care hospitals and 17.8% in long term acute care hospitals
- In 2001: CRE was 1.2% of Enterobacteriaceae
Slide 11
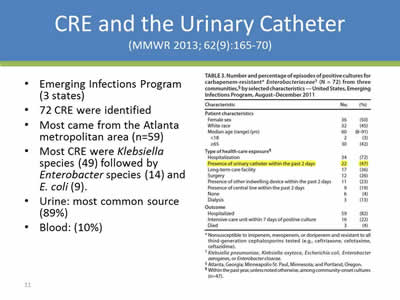
CRE and the Urinary Catheter
(MMWR 2013; 62(9):165-70)
- Emerging Infections Program (3 states)
- 72 CRE were identified
- Most came from the Atlanta metropolitan area (n=59)
- Most CRE were Klebsiella species (49) followed by Enterobacter species (14) and E. coli (9).
- Urine: most common source (89%)
- Blood: (10%)
Image: Screen shot of Table 3 from the journal article, titled Number and percentage of episodes of positive cultures for carbapenem-resistant Enterobacteriaceae (N=72) from three communities, by selected characteristics–United States, Emerging Infections Program, August-December 2011. The data field "Presence of urinary catheter within the past 2 days" is highlighted.
Slide 12
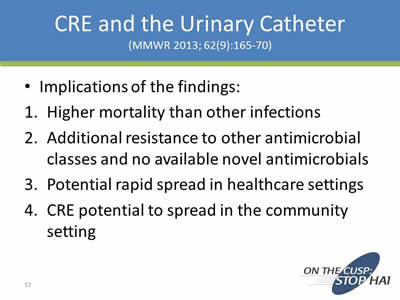
CRE and the Urinary Catheter
(MMWR 2013; 62(9):165-70
- Implications of the findings:
- Higher mortality than other infections
- Additional resistance to other antimicrobial classes and no available novel antimicrobials
- Potential rapid spread in healthcare settings
- CRE potential to spread in the community setting
Slide 13
LTACHs vs ICUs: Multidrug Resistance and CAUTI
(Chitnis, Infect Control Hosp Epidemiol 2012; 33(10):993-1000)
- National data on CAUTI in the ICUs vs. LTACHs
- Microbiology evaluated included resistance
- ICUs: most common 2 organisms E. coli and Candida sp; LTACHs: most common 2 organisms for CAUTI Klebsiella and Pseudomonas sp.
- LTACHs: more MDROs associated CAUTIs
Slide 14
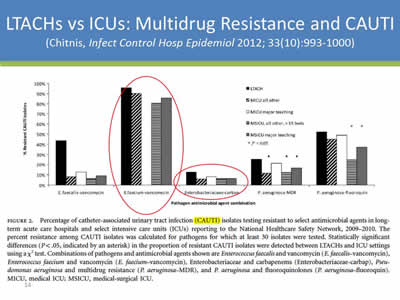
LTACHs vs ICUs: Multidrug Resistance and CAUTI
(Chitnis, Infect Control Hosp Epidemiol 2012; 33(10):993-1000)
Image: Screen shot of Figure 2 from the journal article. It is s bar chart showing percentage of CAUTI isolates testing resistant to multiple antibiotics. The graphs for E. faecium-vancomycin and Enterobacteriaceae-carbam are circled.
Slide 15
LTACHs vs ICUs: Multidrug Resistance and CAUTI
(Chitnis, Infect Control Hosp Epidemiol 2012; 33(10):993-1000)
- More VRE (faecalis) isolates were reported in LTACHs (44%) than in ICUs (7%–13%).
- LTACHs: higher proportion of multidrug resistant P. aeruginosa CAUTI isolates (25%) compared to acute care MICUs (12-16%).
- No significant difference in CRE CAUTI isolates between LTACHs and ICUs, but 42% of LTACHs reported a CRE CAUTI compared to ICUs (8%–21%).
Slide 16
MDROs and CAUTI: NHSN 2009-10
(Sievert, Infect Control Hosp Epidemiol 2013; 34: 1-14)
- 2,039 hospitals
- CAUTI organisms: CRE klebsiella sp 12.5%, CRE E. coli 2.3%, VRE faecium 86%, fluoroquinolone resistant E. coli 67%
- 20% of facilities reported a CRE Klebsiella sp.
Slide 17
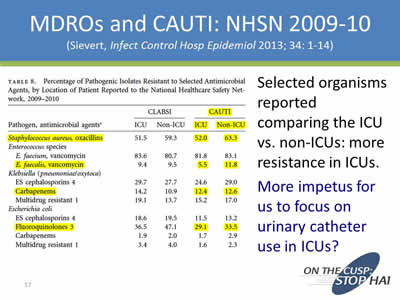
MDROs and CAUTI: NHSN 2009-10
(Sievert, Infect Control Hosp Epidemiol 2013; 34: 1-14)
Selected organisms reported comparing the ICU vs. non-ICUs: more resistance in ICUs.
More impetus for us to focus on urinary catheter use in ICUs?
Image: Screen shot of Table 8 from the journal article titled Percentage of Pathogenic Isolates Resistant to Selected Antimicrobial Agents, by Location of Patient Reported to the National Healthcare Safety Network, 2009-2010.
Slide 18
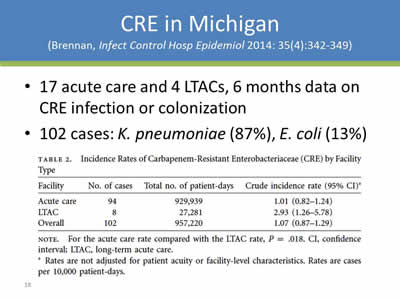
CRE in Michigan
(Brennan, Infect Control Hosp Epidemiol 2014: 35(4):342-349)
- 17 acute care and 4 LTACs, 6 months data on CRE infection or colonization
- 102 cases: K. pneumoniae (87%), E. coli (13%
Image: Screen shot of Table 2 from the journal article titled: Incidence Rates of Carbapenem-Resistant Enterobacteriaceae (CRE) by Facility Type.
Slide 19
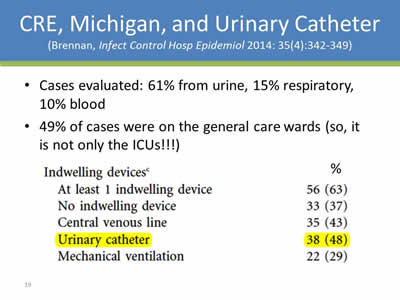
CRE, Michigan, and Urinary Catheter
(Brennan, Infect Control Hosp Epidemiol 2014: 35(4):342-349)
- Cases evaluated: 61% from urine, 15% respiratory, 10% blood
- 49% of cases were on the general care wards (so, it is not only the ICUs!!!)
| Indwelling devices | % |
|---|---|
| At least 1 indwelling device | 56 (63) |
| No indwelling device | 33 (37) |
| Central venous line | 35 (43) |
| Urinary catheter | 38 (48) |
| Mechanical ventilation | 22 (29) |
Slide 20
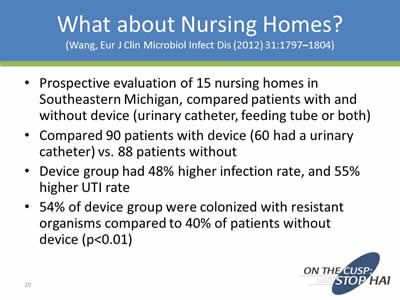
What about Nursing Homes?
(Wang, Eur J Clin Microbiol Infect Dis (2012) 31:1797–1804)
- Prospective evaluation of 15 nursing homes in Southeastern Michigan, compared patients with and without device (urinary catheter, feeding tube or both)
- Compared 90 patients with device (60 had a urinary catheter) vs. 88 patients without
- Device group had 48% higher infection rate, and 55% higher UTI rate
- 54% of device group were colonized with resistant organisms compared to 40% of patients without device (p<0.01)
Slide 21
What do we learn from the studies?
- Urinary catheter use is associated with isolation of MDROs
- This is seen at acute care hospital, LTACH, and nursing homes, in the ICU and non-ICU
- Reducing unnecessary urinary catheter use may help reduce MDRO colonization and consequently spread in the healthcare setting.
Slide 22
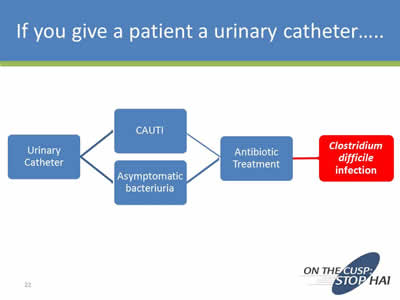
If you give a patient a urinary catheter....
Image: Flowchart starting with Urinary Catheter and branching to CAUTI and Asymptomatic bacteriuria, which both lead to Antibiotic Treatment and finally to Clostridium difficile infection.
Slide 23

Image: Screen shot of an Archives of Internal Medicine article on a hospital outbreak of Clostridium difficile.
Slide 24
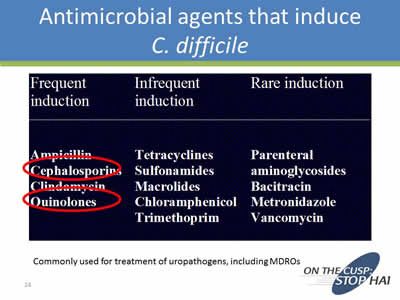
Antimicrobial agents that induce C. difficile
Frequent induction: Ampicillin, Cephalosporin, Clindamycin, and Quinolones
Infrequent induction: Tetracyclines, Sulfonamides, Macrolides, Chloramphenicol, and Trimethoprim
Rare induction: Parenteral aminoglycosides, Bacitracin, Metronidazole, and Vancomycin
Commonly used for treatment of uropathogens, including MDROs
Slide 25
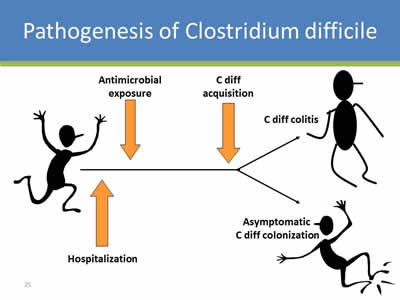
Pathogenesis of Clostridium difficile
Cartoon showing three figures. First figure is being hospitalized, and getting antimicrobial exposure. The second figure gets C diff colitis, and the third figure gets asymptomatic C diff colonization.
Slide 26
Outcomes of C. difficile Infection
- The overall colectomy rate is 8.7 per 1000 CDI cases (Kasper et al Infect Control Hosp Epidemiol. 2012 May;33(5):470-6)
- The estimated number of deaths attributed to CDI, based on multiple cause-of-death mortality data, increased from 3,000 deaths per year during 1999–2000 to 14,000 during 2006–2007. Over 90% of deaths occur in patients over the age of 65 years. (Hall et al Clin Infect Dis. 2012 Jul;55(2):216-23)
Slide 27
Outcomes of CDI
Using 2008 data, CDI may have resulted in $4.8 billion in excess costs in US acute-care facilities (Dubberke et al Clin Infect Dis. 2012 Aug;55 Suppl 2:S88-92)
- Recurrence Rates range from 20-30% for first recurrence
- Increased length of stay with CDI
- Need for ICU care if severely ill
- May need urinary catheter……
Slide 28
Antibiotic Stewardship
ANTIBIOTIC USE AND CLOSTRIDIUM DIFFICILE
We have met the enemy and he is us
Walt Kelly
Slide 29
Inappropriate Antibiotic Use and C. difficile Infection
- 126 consecutive patients with CDI.
- In 93 (73.8%) episodes, at least 1 preceding course of antibiotics was inappropriate. (Am J Infect Control. 2013 Nov;41(11):1116-8.
- Decreasing inappropriate use should lead to reductions in CDI.
Slide 30
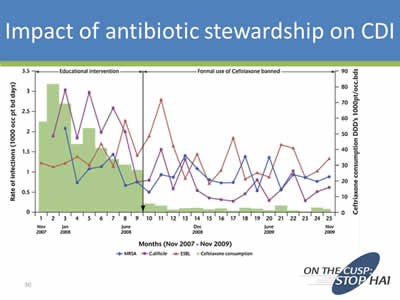
Impact of Antibiotic Stewardship on CDI
Image: Screen shot of a line chart showing decrease in CDI from November 2007-November 2009 after program is instituted.
Slide 31
How Culture Plays a Role in CAUTI Prevention
Kathlyn E. Fletcher, MD MA
Associate Professor of Internal Medicine
Medical College of Wisconsin
Milwaukee VAMC
Slide 32
What We Know From Previous Work
- Qualitative studies by Krein (2013) and Harrod (2013) provide a conceptual model to test
Slide 33
Barriers to Appropriate Use
- Lack of MD and RN engagement:
- MD disinterest
- RN not recognizing the potential severity (“loosely coupled errors?”)
- Workload issues leading to work-arounds
- Weighing risk of catheters v. other issues (i.e. falls)
- Patient/family request:
- Especially incontinence
- ED practice:
- Convenience in ED
- Perception that floor nurses wanted them
Slide 34
Facilitators to Appropriate Use
- MD and RN engagement:
- Nurse champions
- Patient request:
- Education
- ED practice:
- Engaging ED leadership
- Education
- Monitoring
Slide 35
Our Qualitative Study
- Goal: To understand unit-level culture around CAUTI prevention
- Interviews and observations at 4 institutions:
- 2 units per site
- Nurses, physicians, hospital leadership
- Qualitative analysis of the transcripts
- These are interim results
Slide 36
Physician Barriers
- Buy-in is sporadic
“Some people see it and some people don’t. The people who actually see it, you know, are more prone to doing the thing. The people who don't, you know, just think it is a burden.”
–Unit medical director
Slide 37
Physician Barriers
- Knowledge or problem and financial consequences
“I think certain ones feel it's very important and I think other ones will once they realize how it affects the general welfare of the patient plus reporting and plus not getting paid for infections anymore. So I think there's not enough knowledge base on their part of how this is going to affect the bottom line financially as well as, you know, the patient.”
–Infection control professional
Slide 38
Physician Barriers
- Time for checklists
- Interest in checklists versus other things
Slide 39
Nurse Barriers
- Similar to MD barriers in terms of enthusiasm
“So there are mixed feelings. You know, the people who see the value in it actually are very very enthusiastic about it. The people who think it is burdensome because it's another thing for them to do are not really enthusiastic. There are mixed feelings about it actually.”
–Unit medical director
Slide 40
Nurse Barriers
- Workflow issues
- Risk of Foley v. other risks
“I think they always agree with, you know, best practices. I just think sometimes workflow or, you know, if you have a patient who yes they can void but every time the patient uses the urinal they make a big mess, we're not worried about the patient's skin. That's another issue with incontinence in this environment, you know, the benefits versus the risks of placing the Foley catheter. Yeah, they probably want to go ahead and place that Foley catheter. Maybe we can try that condom catheter or something else first. I think those are, I guess I kind of mentioned that before, but I think those are the day-to-day clinical practice frustrations where it's sometimes hard to do the right thing.”
–RN
Slide 41
Nurses and Physician Barriers
- Especially in the ICU, the belief in the need for close monitoring of I’s and O’s
“Most of our patients are critically ill so we do need the Foley so we can measure output, you know, have very accurate I & Os for patients. But we do try to remove them as quickly as possible.”
-Nurse educator
“Response to lessons learned: “I'd give more attention to the ICUs. I would say that again, well, we are very justified, you know, most of the time in having Foley catheters. We do truly need them. I think sometimes we give ourselves a free pass when maybe we didn't deserve it and, you know, maybe we should spend a little more time in that practice environment to see if we can decrease the number of actual Foleys that we have and still be able to achieve good, you know, accurate intake and output. It's challenging but, you know, there may be opportunities there.”
–RN
Slide 42
Patient and Family Barriers
- Not a substantial contributor in our study
Slide 43
Administrative Barriers
- Measurement and reporting
- In response to what lessons have you learned…
“Do you have all day? Just -- it's not as simple as it seems especially when you have a computerized record and you have so many different factors involved and so many different people involved in making decisions and what is important and not important and how to roll it out. And then also just the documentation of it. You know, you want it measured but they're not agreeing in how to document it or how to measure it.”
–Infection control professional
Slide 44
Administrative Barriers
- Dedicated, sustained attention to the issue
“So that's the other hardship. And having to dedicate people underneath to be able to follow through on it. It can't be just infection of the team doing it. It has to be on every floor. It has to be an active involvement. So you actually need champions on the unit level.”
–Infection control professional
Slide 45
Effective Strategies
- Feedback the data:
- Keep it simple (e.g. days since last CAUTI)
- Keep it consistent
- Reward good performance
- Enthusiasm and support from the top down (hospital administration) and the bottom up (unit-level champions)
- Sustained focus so it’s not lost amongst competing priorities
Slide 46
Summary
- Thus far, our data supports the models proposed by Krein and Harrod:
- Physician barriers lessened, but still present
- Nurse barriers are similar
- Patient barriers are lessening
- Identified new administrative barriers (reporting issues)
- Sustained effort with simple message may be an important key
Slide 47
Thank you!
Questions?
Slide 48
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”



