Preventing CAUTI in Special Populations: Focus on Procedure-Related Catheter Use
Slide presentation
Slide 1
Preventing CAUTI in Special Populations: Focus on Procedure-Related Catheter Use
David A. Pegues, MD
Professor of Medicine, Division of Infectious Diseases
Medical Director, Healthcare Epidemiology, Infection Prevention and Control
Hospital of the University of Pennsylvania
Gregory D. Kennedy, MD, PhD
Associate Professor
Vice Chairman of Quality
Associate Chief, Section of Colorectal Surgery
Division of General Surgery
University of Wisconsin School of Medicine
Images: Photos of the 2 presenters.
Slide 2
Learning Objectives
- Describe the indications for urinary catheter use in surgical settings
- Articulate the catheter management challenges in the surgical settings
- Recognize the value in using incentives to change behavior regarding catheter use
Slide 3
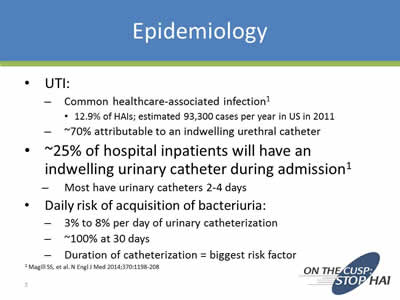
Epidemiology
- UTI:
- Common healthcare-associated infection1
- 12.9% of HAIs; estimated 93,300 cases per year in US in 2011
- ~70% attributable to an indwelling urethral catheter
- Common healthcare-associated infection1
- •~25% of hospital inpatients will have an indwelling urinary catheter during admission1
- Most have urinary catheters 2-4 days
- Daily risk of acquisition of bacteriuria:
- 3% to 8% per day of urinary catheterization
- ~100% at 30 days
- Duration of catheterization = biggest risk factor
1 Magill SS, et al. N Engl J Med 2014;370:1198-208
Slide 4
Polling Question 1
Does your facility currently perform surveillance for CAUTI on surgical units?
- Yes
- No
- No but we’ll have to in January 2015
SUTI + IUC = CAUTI
Slide 5
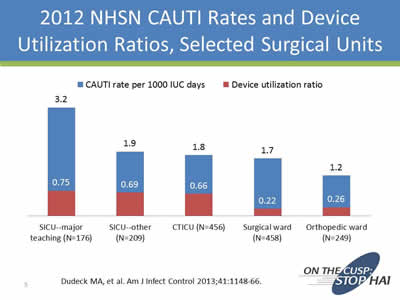
2012 NHSN CAUTI Rates and Device Utilization Ratios, Selected Surgical Units
Image: Bar chart showing CAUTI rates.
| CAUTI rate per 1000 IUC days | Device utilization ratio | |
|---|---|---|
| SICU-major teaching (N=176) | 3.2 | 0.75 |
| SICU-other (N=209) | 1.9 | 0.69 |
| CTICU (N=456) | 1.8 | 0.66 |
| Surgical ward (N=458) | 1.7 | 0.22 |
| Orthopedic ward (N=249) | 1.2 | 0.26 |
Dudeck MA, et al. Am J Infect Control 2013;41:1148-66
Slide 6
IUC Use in Other Procedure Areas
- Labor and Delivery (C-section)
- Electrophysiology/Cath lab
- Interventional Radiology (GU procedures)
- Ambulatory Surgical Centers
Slide 7
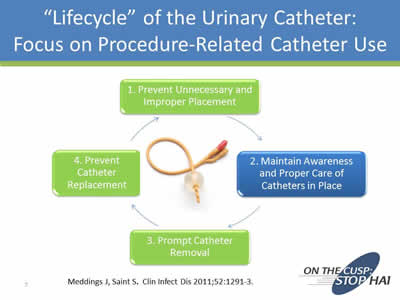
“Lifecycle” of the Urinary Catheter: Focus on Procedure-Related Catheter Use
Image: Circular chart showing the lifecycle of the catheter:
- Prevent Unnecessary and Improper Placement
- Maintain Awareness and Proper Care of Catheters in Place
- Prompt Catheter Removal
- Prevent Catheter Replacement
Meddings J, Saint S. Clin Infect Dis 2011;52:1291-3.
Slide 8
Why Use Urinary Catheters Perioperatively?
- Monitoring urine output during and after major surgery
- Guiding volume resuscitation
- Preventing risk of post-operative urinary retention
Slide 9
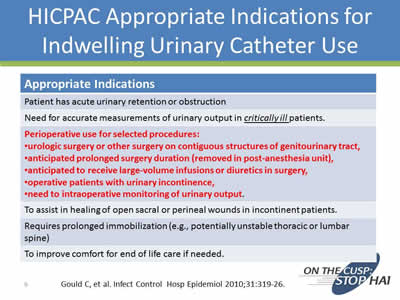
HICPAC Appropriate Indications for Indwelling Urinary Catheter Use
Appropriate Indications
Patient has acute urinary retention or obstruction
Need for accurate measurements of urinary output in critically ill patients.
Perioperative use for selected procedures:
- Urologic surgery or other surgery on contiguous structures of genitourinary tract,
- Anticipated prolonged surgery duration (removed in post-anesthesia unit),
- Anticipated to receive large-volume infusions or diuretics in surgery,
- Operative patients with urinary incontinence,
- Need to intraoperative monitoring of urinary output.
To assist in healing of open sacral or perineal wounds in incontinent patients.
Requires prolonged immobilization (e.g., potentially unstable thoracic or lumbar spine)
To improve comfort for end of life care if needed.
Gould C, et al. Infect Control Hosp Epidemiol 2010;31:319-26.
Slide 10
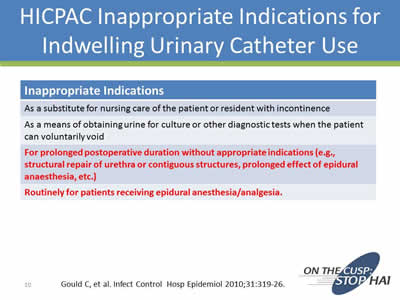
HICPAC Inappropriate Indications for Indwelling Urinary Catheter Use
Inappropriate Indications
As a substitute for nursing care of the patient or resident with incontinence
As a means of obtaining urine for culture or other diagnostic tests when the patient can voluntarily void
For prolonged postoperative duration without appropriate indications (e.g., structural repair of urethra or contiguous structures, prolonged effect of epidural anaesthesia, etc.)
Routinely for patients receiving epidural anesthesia/analgesia.
Gould C, et al. Infect Control Hosp Epidemiol 2010;31:319-26.
Slide 11
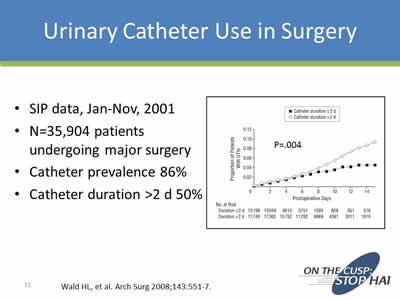
Urinary Catheter Use in Surgery
- SIP data, Jan-Nov, 2001
- N=35,904 patients undergoing major surgery
- Catheter prevalence 86%
- Catheter duration >2 d 50%
Wald HL, et al. Arch Surg 2008;143:551-7.
Image: Graph from paper referenced above with the results described.
Slide 12
Polling Question 2
What is your compliance with SCIP-Inf-9 process measure?
- <80%
- 80-89%
- 90-95%
- >95%
- What is SCIP-Inf-9?
Image on right of slide: the CMS logo.
Slide 13
- SCIP-Inf-9:
- Surgery patients whose urinary catheters were removed on the first or second day after surgery
- One of 12 clinical process of care measures (domain weight 20%) in FY15 Hospital Value-Based Purchasing (VBP) Program
- Current compliance rat– 97%; nearly “topped out”
- Exemptions:
- Patients who had a urological, gynecological or perineal procedure performed
- Patients who had physician/APN/PA documentation of a reason for not removing the urinary catheter postoperatively
https://data.medicare.gov/Hospital-Compare/Hospital-Process-of-Care-Measures-National-Average/2jjc-dc2m Accessed 6/25/14
Slide 14
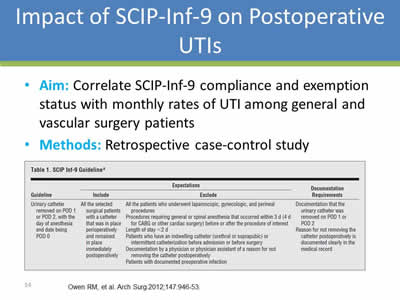
Impact of SCIP-Inf-9 on Postoperative UTIs
- Aim: Correlate SCIP-Inf-9 compliance and exemption status with monthly rates of UTI among general and vascular surgery patients
- Methods: Retrospective case-control study
Owen RM, et al. Arch Surg. 2012;147:946-53.
Image: Screen shot of Table 1. SCIP Inf-9 Guideline.
Slide 15
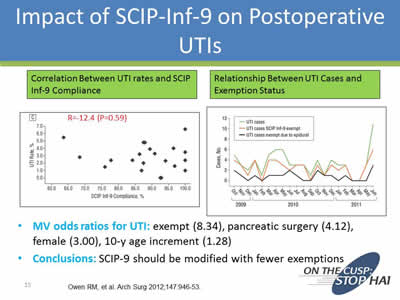
Impact of SCIP-Inf-9 on Postoperative UTIs
- MV odds ratios for UTI: exempt (8.34), pancreatic surgery (4.12), female (3.00), 10-y age increment (1.28)
- Conclusions: SCIP-9 should be modified with fewer exemptions
Owen RM, et al. Arch Surg. 2012;147:946-53.
Images: Screen shots of 2 graphs titled "Correlation Between UTI rates and SCIP Inf-9 Compliance" and "Relationship Between UTI Cases and Exemption Status".
Slide 16
Postoperative Urinary Retention (POUR)
- Incidence: varies widely:
- General surgery: ~3.8%
- Anorectal surgery: 10.7-84%
- Hernia repair: 1-52%
- Risk Factors:
- Preoperative—age >50 yo, male, BPH, previous pelvic surgery, neurological disease, medications
- Intraoperative—procedure, anesthesia
- Postoperative—Bladder volume >270mL in PACU, sedatives, analgesia (CEI, PCEA)
BPH= benign prostatic hypertrophy; CEI=continuous epidural infusion; PCEA = patient-controlled epidural analgesia
Slide 17
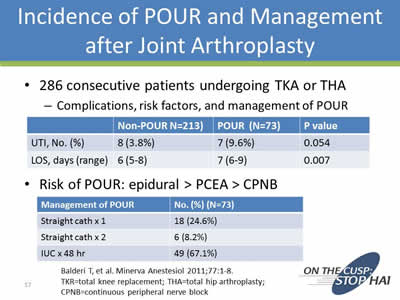
Incidence of POUR and Management after Joint Arthroplasty
- 286 consecutive patients undergoing TKA or THA:
- Complications, risk factors, and management of POUR
| Non-POUR (N=213) | POUR (N=73) | P value | |
|---|---|---|---|
| UTI, No. (%) | 8 (3.8%) | 7 (9.6%) | 0.054 |
| LOS, days (range) | 6 (5-8) | 7 (6-9) | 0.007 |
- Risk of POUR: epidural > PCEA > CPNB
| Management of POUR | No. (%) (N=73) |
|---|---|
| Straight cath x1 | 18 (24.6%) |
| Straight cath x2 | 6 (8.2%) |
| IUC x 48 hr | 49 (67.1%) |
Balderi T, et al. Minerva Anestesiol 2011;77:1-8.
TKR=total knee replacement; THA=total hip arthroplasty; CPNB=continuous peripheral nerve block
Slide 18
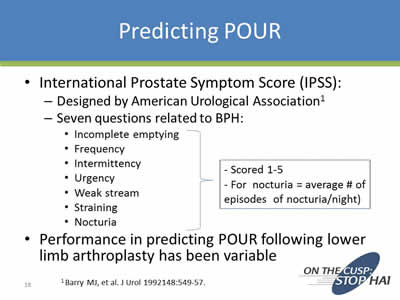
Predicting POUR
- International Prostate Symptom Score (IPSS):
- Designed by American Urological Association1
- Seven questions related to BPH (Scored 1-5. For nocturia = average # of episodes of nocturia/night):
- Incomplete emptying
- Frequency
- Intermittency
- Urgency
- Weak stream
- Straining
- Nocturia
- Performance in predicting POUR following lower limb arthroplasty has been variable
1 Barry MJ, et al. J Urol 1992148:549-57.
Slide 19
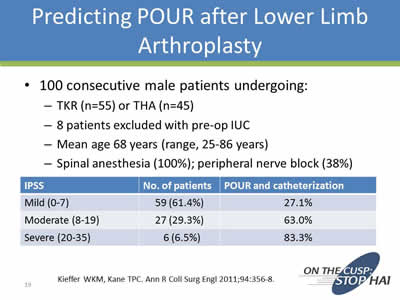
Predicting POUR after Lower Limb Arthroplasty
- 100 consecutive male patients undergoing:
- TKR (n=55) or THA (n=45)
- 8 patients excluded with pre-op IUC
- Mean age 68 years (range, 25-86 years)
- Spinal anesthesia (100%); peripheral nerve block (38%)
| IPSS | No. of patients | POUR and catheterization |
|---|---|---|
| Mild (0-7) | 59 (61.4%) | 27.1% |
| Moderate (8-19) | 27 (29.3% | 63.0% |
| Severe (20-35) | 6 (6.5%) | 83.3% |
Kieffer WKM, Kane TPC. Ann R Coll Surg Engl 2011;94:356-8.
Slide 20
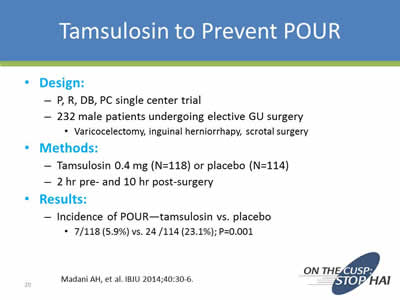
Tamsulosin to Prevent POUR
- Design:
- P, R, DB, PC single center trial
- 232 male patients undergoing elective GU surgery:
- Varicocelectomy, inguinal herniorrhapy, scrotal surgery
- Methods:
- Tamsulosin 0.4 mg (N=118) or placebo (N=114)
- 2 hr pre- and 10 hr post-surgery
- Results:
- Incidence of POUR—tamsulosin vs. placebo
- 7/118 (5.9%) vs. 24 /114 (23.1%); P=0.001
- Incidence of POUR—tamsulosin vs. placebo
Madani AH, et al. IBJU 2014;40:30-6.
Slide 21
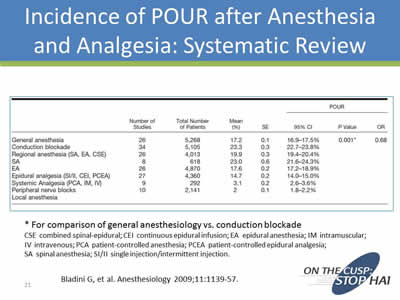
Incidence of POUR after Anesthesia and Analgesia: Systematic Review
Image: Screen shot of table showing incidences of POUR after anesthesia and analgesia from a number of studies.
*For comparison of general anesthesiology vs. conduction blockade
CSE combined spinal-epidural; CEI continuous epidural infusion; EA epidural anesthesia; IM intramuscular; IV intravenous; PCA patient-controlled anesthesia; PCEA patient-controlled epidural analgesia; SA spinal anesthesia; SI/II single injection/intermittent injection.
Bladini G, et al. Anesthesiology 2009;11:1139-57.
Slide 22
Polling Question 3
Do you know whether urinary catheters are routinely inserted in patients receiving epidural anesthesia at your facility?
- Yes, in all patients
- Yes, but only in selected patients
- Never
- Don’t know
Image: Photo of hands inserting a urinry catheter.
Slide 23
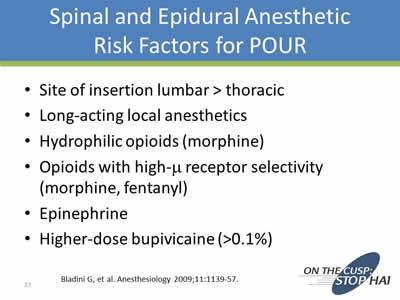
Spinal and Epidural Anesthetic Risk Factors for POUR
- Site of insertion lumbar > thoracic
- Long-acting local anesthetics
- Hydrophilic opioids (morphine)
- Opioids with high-m receptor selectivity (morphine, fentanyl)
- Epinephrine
- Higher-dose bupivicaine (>0.1%)
Bladini G, et al. Anesthesiology 2009;11:1139-57.
Slide 24
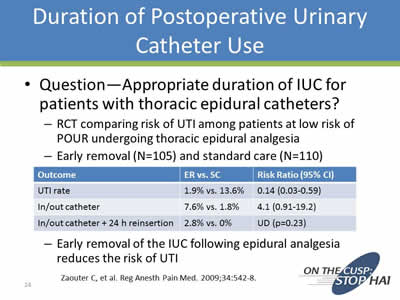
Duration of Postoperative Urinary Catheter Use
- Question—Appropriate duration of IUC for patients with thoracic epidural catheters?
- RCT comparing risk of UTI among patients at low risk of POUR undergoing thoracic epidural analgesia
- Early removal (N=105) and standard care (N=110)
- Early removal of the IUC following epidural analgesia reduces the risk of UTI
| Outcome | ER vs. SC | Risk Ratio (95% CI) |
|---|---|---|
| UTI rate | 1.9% vs. 13.6% | 0.14 (0.03-0.59) |
| In/out catheter | 7.6% vs. 1.8% | 4.1 (0.91-19.2) |
| In/out catheter +24h reinsertion | 2.8% vs. 0% | UD (p=0.23) |
Zaouter C, et al. Reg Anesth Pain Med. 2009;34:542-8.
Slide 25
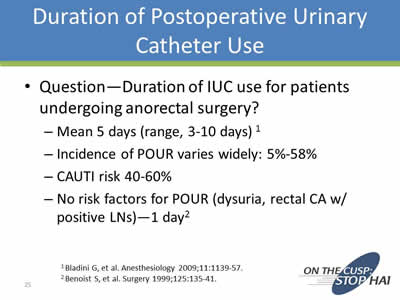
Duration of Postoperative Urinary Catheter Use
- Question—Duration of IUC use for patients undergoing anorectal surgery?
1Bladini G, et al. Anesthesiology 2009;11:1139-57.
2Benoist S, et al. Surgery 1999;125:135-41.
Slide 26
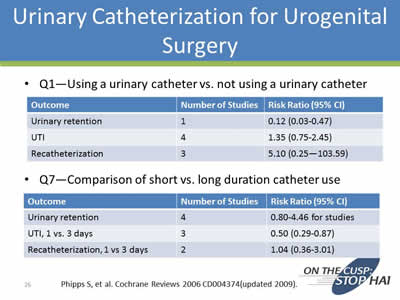
Urinary Catheterization for Urogenital Surgery
- Q1—Using a urinary catheter vs. not using a urinary catheter
| Outcome | Number of Studies | Risk Ratio (95% CI) |
|---|---|---|
| Urinary retention | 1 | 0.12 (0.03-0.47) |
| UTI | 4 | 1.35 (0.75-2.45) |
| Recatheterization | 3 | 5.10 (0.25-103.59) |
- Q7—Comparison of short vs. long duration catheter use
| Outcome | Number of Studies | Risk Ratio (95% CI) |
|---|---|---|
| Urinary retention | 4 | 0.80-4.46 for studies |
| UTI, 1 vs. 3 days | 3 | 0.50 (0.29-0.87) |
| Recatheterization, 1 vs. 3 days | 2 | 1.04 (0.36-3.01) |
Phipps S, et al. Cochrane Reviews 2006 CD004374 (updated 2009).
Slide 27
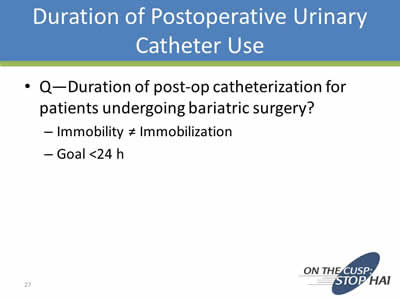
Duration of Postoperative Urinary Catheter Use
- Q—Duration of post-op catheterization for patients undergoing bariatric surgery?
- Immobility ≠ Immobilization
- Goal <24 h
Slide 28
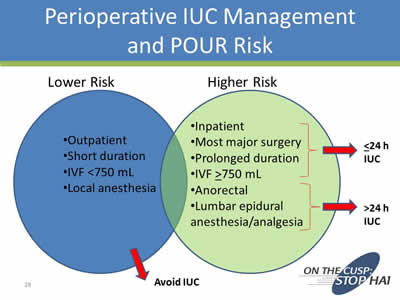
Perioperative IUC Management and POUR Risk
Image: Chart showing Lower and Higher Risk categories.
Lower Risk
- Outpatient
- Short duration
- IVF <750 mL
- Local anesthesia
Leads to avoiding IUC.
Higher Risk
- <24h IUC:
- Inpatient
- Most major surgery
- Prolonged duration
- IVF >750 mL
- >24h IUC
- Anorectal
- Lumbar epidural anesthesia/analgesia
Slide 29
Polling Question 4
Do providers at your facility utilize a post-removal protocol to manage post-operative urinary retention among surgical patients?
- Yes
- .No
- No, but we are considering it
- What is a post-removal protocol?
Slide 30
Recommended Intervention
- Develop a protocol for management of postoperative urinary retention, including nurse-directed use of intermittent catheterization and use of bladder scanners
Lo E et al. Infect Control Hosp Epidemiol. 2014;35:464-79.
Slide 31
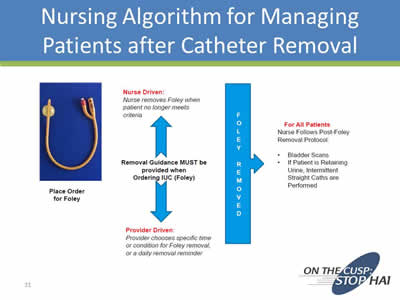
Nursing Algorithm for Managing Patients after Catheter Removal
Image: Diagram of a nursing algorithm for managing patients.
Slide 32
Summary—1
- Reduce procedure-related urinary catheter use by:
- Limiting indications to selected procedures and patients at increased risk of POUR
- Limiting duration—order sets and nurse-driven removal protocol
- Limiting reinsertion—post-removal protocol with bladder scanning
Slide 33
Implementing a Program: Hurdles Cleared and Lessons Learned
Gregory D. Kennedy, MD, PhD
Associate Professor
Vice Chairman of Quality
Associate Chief, Section of Colorectal Surgery
Division of General Surgery
University of Wisconsin School of Medicine
Slide 34
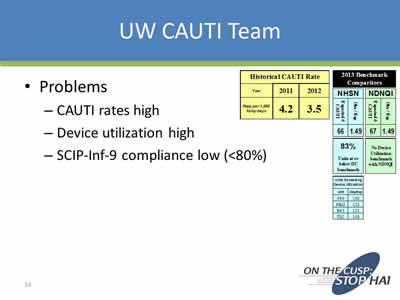
UW CAUTI Team
- Problems:
- CAUTI rates high
- Device utilization high
- SCIP-Inf-9 compliance low (<80%)
Images: Screen shots of several small tables on CAUTI measures.
Slide 35
Approach
- Multidisciplinary team:
- MD team leader
- RN team leader
- Executive team leader
- Unit RNS
- Clinical nurse specialist
- Infection control specialist
Slide 36
CAUTI Framework
- Insertion:
- Would require standard approach
- Use CLABSI work as blueprint
- Maintenance:
- Paucity of data on how to manage catheter once in place
- Removal:
- Low-lying fruit. Starting point!
Slide 37
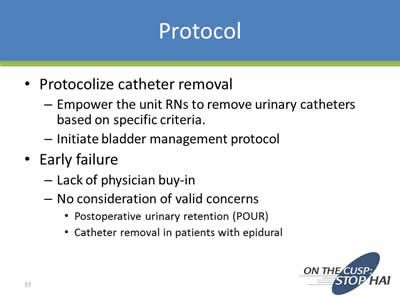
Protocol
- Protocolize catheter removal:
- Empower the unit RNs to remove urinary catheters based on specific criteria.
- Initiate bladder management protocol
- Early failure:
- Lack of physician buy-in
- No consideration of valid concerns:
- Postoperative urinary retention (POUR)
- Catheter removal in patients with epidural
Slide 38
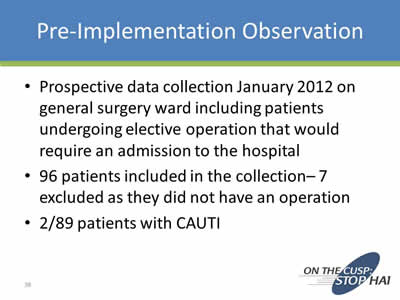
Pre-Implementation Observation
- Prospective data collection January 2012 on general surgery ward including patients undergoing elective operation that would require an admission to the hospital
- 96 patients included in the collection– 7 excluded as they did not have an operation
- 2/89 patients with CAUTI
Slide 39
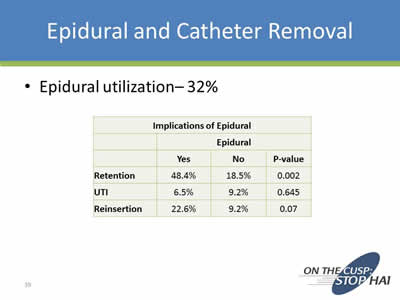
Epidural and Catheter Removal
- Epidural utilization– 32%
Implications of Epidural
| Epidural | |||
|---|---|---|---|
| Yes | No | P value | |
| Retention | 48.4% | 18.5% | 0.002 |
| UTI | 6.5% | 9.2% | 0.645 |
| Reinsertion | 22.6% | 9.2% | 0.07 |
Slide 40
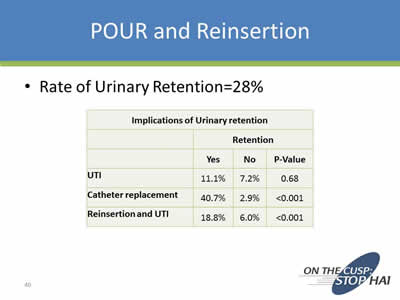
POUR and Reinsertion
- Rate of Urinary Retention=28%
Implications of Urinary Retention
| Retention | |||
|---|---|---|---|
| Yes | No | P value | |
| UTI | 11.1% | 7.2% | 068 |
| Catheter replacement | 40.7% | 2.9% | <0.001 |
| Reinsertion and UTI | 18.8% | 6.0% | <0.001 |
Slide 41

Outcomes of Collection
- Fed data back to anesthesia on rates of retention with epidural.
- Data back to faculty to relieve some concerns regarding POUR (overwhelming sense was that POUR was >75%).
Slide 42
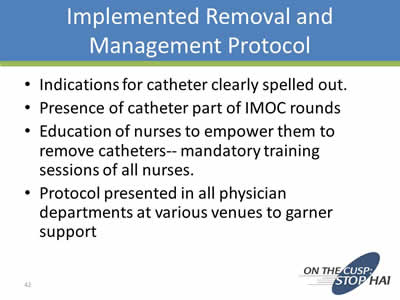
Implemented Removal and Management Protocol
- Indications for catheter clearly spelled out.
- Presence of catheter part of IMOC rounds
- Education of nurses to empower them to remove catheters-- mandatory training sessions of all nurses.
- .Protocol presented in all physician departments at various venues to garner support
Slide 43
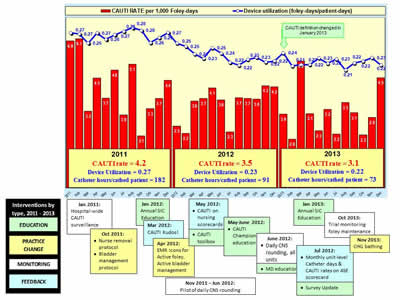
Image: Graph and timeline showin CAUTI rates from 2011 to 2013. In 2011 the rate was 4.2 per 1,000 Foley-days, but by 2013 it was down to 3.1.
Slide 44
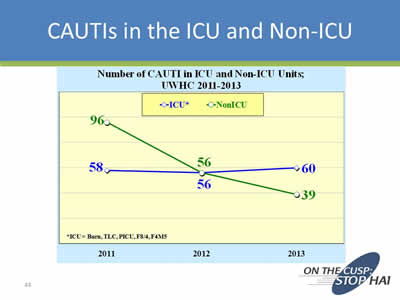
CAUTIs in the ICU and Non-ICU
Image: Chart showing a sharp decrease in CAUTI rates from 2011 to 2013 in non-ICU units (96 down to 39), but a steady rate in the ICU (58 up to 60).
Slide 45
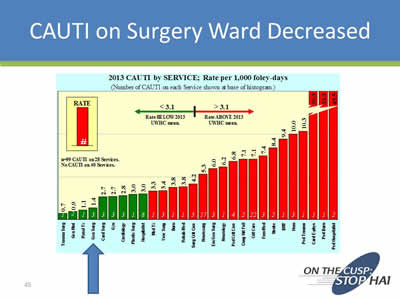
CAUTI on Surgery Ward Decreased
Image: Bar chart showing 2013 CAUTI rates for different units of the hospital, with an arrow pointing to the General Surgery Unit rate.
Slide 46
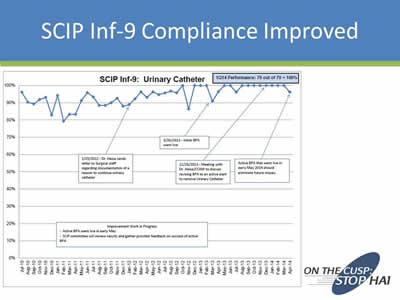
SCIP Inf-9 Compliance Improved
Image: Chart showing compliance rates from July 2010 to April 2014.
Slide 47
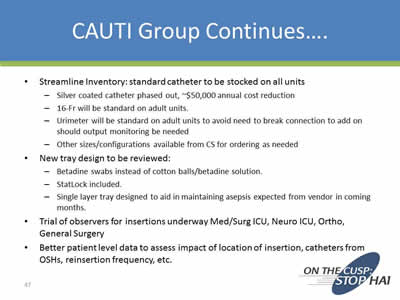
CAUTI Group Continues….
- Streamline Inventory: standard catheter to be stocked on all units:
- Silver coated catheter phased out, ~$50,000 annual cost reduction
- 16-Fr will be standard on adult units.
- Urimeter will be standard on adult units to avoid need to break connection to add on should output monitoring be needed
- Other sizes/configurations available from CS for ordering as needed
- New tray design to be reviewed:
- Betadine swabs instead of cotton balls/betadine solution.
- StatLock included.
- Single layer tray designed to aid in maintaining asepsis expected from vendor in coming months.
- Trial of observers for insertions underway Med/Surg ICU, Neuro ICU, Ortho, General Surgery
- Better patient level data to assess impact of location of insertion, catheters from OSHs, reinsertion frequency, etc.
Slide 48
Summary—2
- Multidisciplinary team critical:
- Size of the team cannot be too cumbersome
- Include critical stakeholders– especially your most vocal naysayers (i.e., embrace your surgeons)
- Show the data
- Thick skin– change is hard and conflict is inevitable!
Slide 49
Thank you!
Questions?
Slide 50
Funding
Prepared by the Health Research & Educational Trust of the American Hospital Association with contract funding provided by the Agency for Healthcare Research and Quality through the contract, “National Implementation of Comprehensive Unit-based Safety Program (CUSP) to Reduce Catheter-Associated Urinary Tract Infection (CAUTI), project number HHSA290201000025I/HHSA29032001T, Task Order #1.”



