Module 1: Overview
Preventing CAUTI in the ICU Setting Slide Presentation
Slide 1
AHRQ Safety Program for Reducing CAUTI in Hospitals
Preventing CAUTI in the ICU Setting
Module 1: Overview
AHRQ Pub. No. 15-0073-4-EF
September 2015
Slide 2
Learning Objectives
- At the end of this educational event, the participant will be able to:
- Describe the scope of catheter-associated urinary tract infections (CAUTI)
- State the indications for an indwelling urinary catheter
- Identify causes of CAUTI in the intensive care unit (ICU)
- Describe methods to mitigate the risk of CAUTI
Slide 3
Scope of the Problem
- An estimated 560,000 patients develop hospital-acquired UTIs per year1
1. Gould CD, Umscheid CA, Agarwal RK, et al. Guideline for Prevention of Catheter-Associated Urinary Tract Infections 2009. Centers for Disease Control and Prevention. http://www.cdc.gov/hicpac/pdf/CAUTI/CAUTIguideline2009final.pdf.
2. Centers for Disease Control and Prevention. Catheter-Associated Urinary Tract Infections. http://www.cdc.gov/HAI/ca_uti/uti.html. Accessed May 15, 2015.
3. Lo E, Nicolle LE, Coffin SE, et al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014 May;35(5):464-79. PMID: 24709715.
Slide 4
Scope of the Problem
- CAUTIs:
- One of the most common types of healthcare-associated Infection (HAI)3
- Account for 23% of all HAIs in ICU4
- Over 30% of all infections reported to Centers for Disease Control and Prevention’s National Healthcare Safety Network
- Leading cause of secondary bloodstream infection3
- Increase length of stay 2-4 days3
- Result in additional antimicrobial use and antimicrobial resistance
4. Chenoweth C, Saint S. Preventing catheter-associated urinary tract infections in the intensive care unit. Crit Care Clin. 2013 Jan;29(1):19-32. PMID: 23182525.
Slide 5
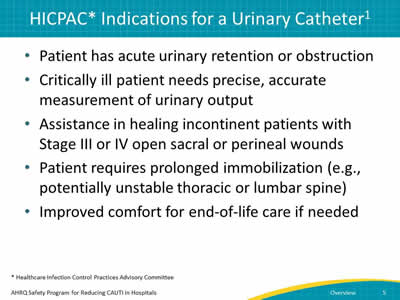
HICPAC* Indications for a Urinary Catheter1
- Patient has acute urinary retention or obstruction
- Critically ill patient needs precise, accurate measurement of urinary output
- Assistance in healing incontinent patients with Stage III or IV open sacral or perineal wounds
- Patient requires prolonged immobilization (e.g., potentially unstable thoracic or lumbar spine)
- Improved comfort for end-of-life care if needed
* Healthcare Infection Control Practices Advisory Committee
Slide 6
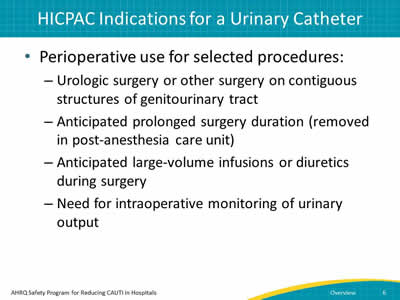
HICPAC Indications for a Urinary Catheter
- Perioperative use for selected procedures:
- Urologic surgery or other surgery on contiguous structures of genitourinary tract
- Anticipated prolonged surgery duration (removed in post-anesthesia care unit)
- Anticipated large-volume infusions or diuretics during surgery
- Need for intraoperative monitoring of urinary output
Slide 7
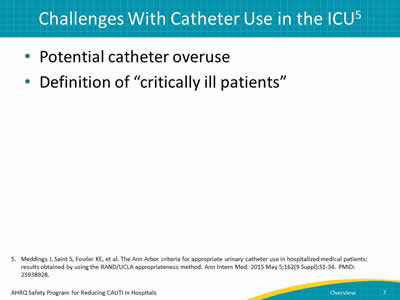
Challenges With Catheter Use in the ICU5
- Potential catheter overuse
- Definition of “critically ill patients”
5. Meddings J, Saint S, Fowler KE, et al. The Ann Arbor criteria for appropriate urinary catheter use in hospitalized medical patients: results obtained by using the RAND/UCLA appropriateness method. Ann Intern Med. 2015 May 5;162(9 Suppl):S1-34. PMID: 25938928.
Slide 8
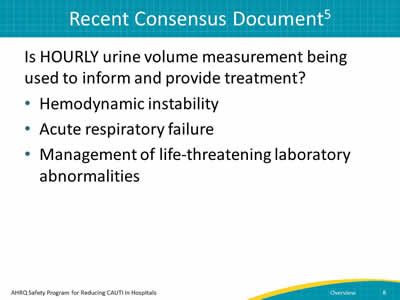
Recent Consensus Document5
Is HOURLY urine volume measurement being used to inform and provide treatment?
- Hemodynamic instability
- Acute respiratory failure
- Management of life-threatening laboratory abnormalities
Slide 9
Consensus
- Is daily urine volume measurement being used to provide treatment AND volume status cannot be adequately or reliably assessed without a Foley catheter, such as by daily weight or urine collection by urinal, commode, bedpan, or external catheter?
- Examples: Management of acute renal failure, IV fluids, or IV or oral bolus diuretics
- Fluid management in acute respiratory failure requiring large volumes of oxygen (≥5 L/min or >50%)
Slide 10
Stop and Think
- What are you doing in your facility?
- Are your practices well defined and current?
- What are your barriers?
Slide 11
Variables Impacting CAUTI in ICU Settings
- Technical Issues
- Evidence-based guidelines
- Socio-adaptive (cultural issues)
- Staff behavior and unit culture
Slide 12
Technical Challenges
- Can be solved with existing, “knowledge-based” science or technology
- Ask yourself:
- Have we summarized the evidence and disseminated to the frontline staff?
- Is there a lack of knowledge of prevention and prevalence of CAUTI in ICU?
- Do we evaluate and share info on CAUTI rates and device use ratios?
Slide 13
Adaptive or Cultural Changes
- Require a change of values, attitudes, or beliefs (i.e., “behavior based”)
- Examples:
- Are nurses reluctant to remove urinary catheters even when the patient no longer meets criteria for a catheter?
- Are physicians engaged in CAUTI prevention?
Slide 14
Etiology of CAUTI
- Patient’s colonic or perineal flora
- Bacteria on hands of patient and personnel
- Microbes enter bladder via two routes:
- Extraluminal: Around the external surface
- Intraluminal: Inside the catheter
- Daily risk of bacteriuria with catheterization
- 3% to 7%
- By day 30, 100%
Slide 15
Patient Factors
- ICU patients who are critically ill may be at high risk for infection for many reasons
- Underlying comorbid conditions
- Exposure to invasive devices
- Antibiotic exposure putting them at risk for multiple drug-resistant organisms (MDROs)
Slide 16
Behavioral or Cultural Factors
- Pan culturing
- ICUs may obtain cultures from multiple sites when a patient has a temperature spike
- Not an automatic culture
- Belief that all patients need a urinary catheter
- Sending routine admission orders on patients admitted with a urinary catheter without signs and symptoms of infections
Slide 17
Methods for Mitigating Risk
- Optimize insertion practices
- Prevent insertion of catheters when patient's case does not meet one of HICPAC's approved indications
- Promote aseptic insertion by trained personnel with competency documented by direct observation
Slide 18
Methods for Mitigating Risk
- Optimize catheter maintenance
- Periodic audit
- Direct observation
- Maintenance bundle
- Maintain unobstructed urine flow
- Maintain a continually closed system
- Perform hand hygiene and use standard precautions
- Empty urine drainage bag regularly and always before transport
- Perform routine meatal care (minimum of daily)
Slide 19
Methods for Mitigating Risk
- Limit duration of catheter use
- Device rounds
- Daily assessment of indication
- Continued need for hourly monitoring of fluid intake and output?
- Needed to titrate meds?
- Reminders/stop orders
- Nurse-driven removal protocol
Slide 20
Methods for Mitigating Risk
- Follow evidence-based culturing practices
- Perform clinical assessment for signs/symptoms of UTI
- Increase use of alternatives to indwelling urinary catheters
- `Condom catheters (evaluate multiple products)
- Moisture-wicking incontinence pads
- Bladder scanners
- Intermittent catheterization
Slide 21
Demonstrate Team-Based Practices
- Mitigating risk of CAUTI requires a team approach
- 1:1 Conversations
- Drill down on CAUTI (Learning From Defects tool)
- Nurse-physician cooperation!
Slide 22
References
- Gould CD, Umscheid CA, Agarwal RK, et al. Guideline for Prevention of Catheter-Associated Urinary Tract Infections 2009. Centers for Disease Control and Prevention. http://www.cdc.gov/hicpac/pdf/CAUTI/CAUTIguideline2009final.pdf.
- Centers for Disease Control and Prevention. Catheter-Associated Urinary Tract Infections. http://www.cdc.gov/HAI/ca_uti/uti.html. Accessed May 15, 2015.
- Lo E, Nicolle LE, Coffin SE, et al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014 May;35(5):464-79. PMID: 24709715.
- Chenoweth C, Saint S. Preventing catheter-associated urinary tract infections in the intensive care unit. Crit Care Clin. 2013 Jan;29(1):19-32. PMID: 23182525.
- Meddings J, Saint S, Fowler KE, et al. The Ann Arbor criteria for appropriate urinary catheter use in hospitalized medical patients: results obtained by using the RAND/UCLA appropriateness method. Ann Intern Med. 2015 May 5;162(9 Suppl):S1-34. PMID: 25938928.



