Module 3: Staff Empowerment: Facilitator Notes
AHRQ Safety Program for Long-Term Care: HAIs/CAUTI
Slide 1: Module 3: Staff Empowerment
Say:
The Staff Empowerment module will discuss the importance of staff empowerment and strategies for implementing staff empowerment in your facility.
Slide 2: Objectives
Say:
The objectives are to—
- Cite staff empowerment concepts.
- Discuss how staff empowerment contributes to a culture of resident safety, leading to improved outcomes and quality of life.
- Illustrate three ways to increase staff empowerment.
- Explain how to address and overcome challenges to staff empowerment.
Slide 3: What Is Staff Empowerment?
Say:
Empowerment is the belief that you have the control and competence needed to make decisions. An organization that provides its staff access to support, resources, information, and opportunities to learn and grow will have a positive effect on employee job satisfaction and the quality of care they provide.
Access to support refers to feedback and guidance from supervisors, peers, and direct reports. Access to resources includes funds, supplies, and time required to meet project goals. Access to information refers to the availability of knowledge of the organization's values, goals and policies, and staff's knowledge and expertise required to work effectively. Lastly, access to opportunity is the availability of challenges, rewards, and professional development opportunities to increase job-related knowledge and skills.
Slide 4: Organizational Factors for Staff Empowerment2-4
Say:
Organizational factors that can affect staff empowerment are—
- Structures for advancement opportunities.
- Awareness of staff contributions.
- Access to resources, information, and support.
Staff empowerment is both the process and the outcome that provides employees the ability to make effective, timely decisions. This includes providing the resources and culture that support decision making. While staff empowerment starts from leadership, the team and staff will be ultimately responsible for keeping up the motivation, project momentum, and positive reinforcement for one another to sustain long-term efforts.
2. Brannon D, Mor V. Nurse aide empowerment strategies and staff stability: Effects on nursing home resident outcomes. The Gerontologist. 2005;45(3):309-317.
3. Bowers N, Nolet K, Roberts E, et al. Implementing Change in Long-Term Care: A Practical Guide to Transformation. University of Wisconsin–Madison, School of Nursing; 2007.
4. Cready C, Yeatts D, Gosdin M, et al. CNA empowerment: Effects On Job Performance And Work Attitudes. Journal of Gerontological Nursing. 2008;34(3):26-35.
Slide 5: Staff Empowerment Assessment Tools3,5
Ask:
What does it look like when staff is empowered? How is it reflected in their behavior?
Say:
Measuring worker empowerment can help managers identify and remove conditions in the organization that lead to powerlessness. Several instruments are available to measure staff empowerment in long-term care. Consider gathering baseline empowerment data before you begin to implement changes and again afterwards. The U.S. Department of Health and Human Services, the U.S. Department of Labor, and the Institute for the Future of Aging Services have developed a report listed here that provides many tools to measure your staff empowerment level.
3. Bowers N, Nolet K, Roberts E, et al. Implementing Change in Long-Term Care: A Practical Guide to Transformation. University of Wisconsin–Madison, School of Nursing; 2007.
5. Harris-Kojetin L, Brannon D, Barry T, et al. Measuring Long-Term Care Work: A Guide to Selected Instruments To Examine Direct Care Worker Experiences and Outcomes. Washington, D.C.: U.S. Department of Health & Human Services, U.S. Department of Labor; 2005.
Slide 6: Psychological Empowerment Instrument5
Say:
For example, the Psychological Empowerment Instrument was designed to measure four dimensions of empowerment: meaning, competence, self-determination, and impact. The tool has 12 questions, which can be administered in 5 to 10 minutes. Sample questions include—
How strongly do you agree or disagree with these statements?
- I am confident about my ability to do my job.
- I am self-assured about my capability to perform my work.
- I have mastered the skills necessary for my job.
5. Harris-Kojetin L, Brannon D, Barry T, et al. Measuring Long-Term Care Work: A Guide to Selected Instruments To Examine Direct Care Worker Experiences and Outcomes. Washington, D.C.: U.S. Department of Health & Human Services, U.S. Department of Labor; 2005.
Slide 7: Why is Staff Empowerment Important?5,6

Say:
Studies have found that nurses who feel more empowered have higher job satisfaction, are more committed to their employer, and are less likely to voluntarily quit. An empowered front-line staff in nursing homes has also been shown to have lower turnover and provide improved quality of care.
5. Harris-Kojetin L, Brannon D, Barry T, et al. Measuring Long-Term Care Work: A Guide to Selected Instruments To Examine Direct Care Worker Experiences and Outcomes. Washington, D.C.: U.S. Department of Health & Human Services, U.S. Department of Labor; 2005.
6. Kolus K. Mather Pavilion – Staff Empowerment Yields Quality Improvement. Long-Term Living. 2010;59(9):20.
Slide 8: Relationship Between Resident Quality of Life and Staff Empowerment7
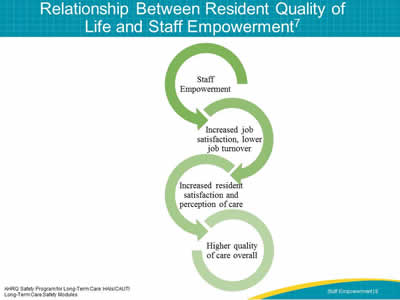
Say:
This illustration shows a positive relationship between staff empowerment and resident quality of life. Staff empowerment leads to higher job satisfaction, resulting in lower turnover. This leads to happier staff, which increases resident satisfaction and perception of care. This is particularly true for frontline staff in nursing homes like the certified nursing assistants, or CNAs, as they have the most contact with residents and are more able to quickly respond to resident needs and changes. When frontline staff can influence day-to-day resident care decisions, both staff and residents are more satisfied. All these factors together lead to higher quality of care.
7. Hamann DJ. Does Empowering Resident Families or Nursing Home Employees in Decision Making Improve Service Quality? Journal of Applied Gerontology. 2014;33(5):603-23
Slide 9: Importance of Empowering Nursing Staff4,7
Say:
Empowerment of nursing staff in decision making is more strongly related to increased service quality than empowerment of non-nursing staff. In nursing homes, it's particularly important for CNAs and other frontline caregivers to be empowered because they're resident advocates and can recognize and respond to resident needs in real time.
Nursing home administrators may want to consider creating teams that include employees with similar job titles and responsibilities who make decisions and recommendations on aspects of their jobs. Through empowerment, teams see their position as meaningful which can boost morale and job performance.
4. Cready C, Yeatts D, Gosdin M, et al. CNA empowerment: Effects On Job Performance And Work Attitudes. Journal of Gerontological Nursing. 2008;34(3):26-35.
7. Hamann DJ. Does Empowering Resident Families or Nursing Home Employees in Decision Making Improve Service Quality? Journal of Applied Gerontology. 2014;33(5):603-23
Slide 10: Characteristics of an Empowered Frontline Staff
Say:
Empowered staff have the following characteristics: They are curious, interested in improvement, and have knowledge of nursing home resources and infrastructure.
Slide 11: Curiosity
Say:
Staff who are empowered are invested in the success of the facility and the safety of its residents. By nurturing this curiosity, staff will feel comfortable speaking up and suggesting changes and improvements. Administrators want to provide an environment in which staff are comfortable asking questions about their work and the reasons for certain procedures.
Slide 12: Interest in Improvement
Say:
Administrators should support staff interest in finding ways to do things better. Because frontline staff are the people closest to bedside processes, they have the greatest insight as to how things can be improved and which solutions are most likely to work. The success rate of process improvement can be enhanced though an empowered staff, as their hands-on input increases the likelihood of buy-in and acceptance of the new process.
Slide 13: Knowledge of Nursing Home Resources and Infrastructure
Say:
An empowered staff will have a broad view of resources and infrastructure. They know what help to seek, when to seek it, and who to ask. To give an example of this view, ask yourself these questions:
How do we get our drugs from the pharmacy? Is there something about this process that affects my ability to do my clinical work? How does this process affect my residents? How can it be improved? How does this improvement affect not just my residents, but all the residents in the facility?
An empowered staff—
- Understands how to assess organizational processes on clinical practice and be actively involved in these assessments.
- Is actively involved in the evaluation of practice interventions at an individual and an organizational level.
- Is comfortable participating in both of these activities.
Slide 14: What Builds Staff Empowerment?
Say:
Staff empowerment can be facilitated by starting with a leader sharing the vision of an empowered staff and creating teams of frontline staff. By building trust and confidence, leadership and staff will have improved communication and information sharing. When confident and empowered staff use their shared information to improve care, leaders should provide positive reinforcement. A Just Culture is one that allows teams to learn from mistakes in a safe environment. If one team member makes a mistake, it's viewed as an opportunity for the entire team to learn and improve the process or system. On the flip side, if you don't have a Just Culture, staff will not report when an error happens because they will fear punishment, and processes may not change and the same mistakes will continue to happen.
Slide 15: An Empowered Team
Say:
The following video shows an empowered team. See if you can identify the elements of staff empowerment.
PLAY VIDEO:
Video 2.2: Enabling the Team
Ask:
Can you see how teamwork builds staff empowerment in the video? Are there examples of similar meetings and teamwork in your facility?
Slide 16: Leader Support and Teams2,4
Say:
No member of the facility staff should be left out of the quality improvement process. Each staff member provides a unique and valuable perspective which allows all aspects of resident safety to be considered. Hierarchies within teams should be eliminated, as it creates a system in which one person's input is more valuable than another's. Leaders assist teams in setting ground rules, making it safe to speak up and voice concerns at any level. It's important to value each perspective equally, particularly of staff members who may be skeptical about their input being taken seriously.
Leaders should also provide access to resources for an empowered staff. This can include channels for advancement or growth in the organization, such as incentive or career ladder programs for employees, opportunities for staff to build their knowledge and skills, including staff training about best practices for safety and infection prevention, and allowing staff to participate in task forces or committees that influence decisions related to day-to-day care, such as redesign of facility and resident spaces, operations or technology to help staff do their jobs more efficiently.
2. Brannon D, Mor V. Nurse aide empowerment strategies and staff stability: Effects on nursing home resident outcomes. The Gerontologist. 2005;45(3):309-317.
4. Cready C, Yeatts D, Gosdin M, et al. CNA empowerment: Effects On Job Performance And Work Attitudes. Journal of Gerontological Nursing. 2008;34(3):26-35.
Slide 17: Teamwork and Support
Say:
Watch this video showing two colleagues discussing a resident issue.
PLAY VIDEO
Video 3.1 Teamwork and Support
Ask:
How have staff training opportunities contributed to the way Sharon and Joni handled the situation? How would you have acted in their situation?
Slide 18: Communication and Information Sharing3
Say:
Encouraging two-way communication between management and staff is crucial. Most managers will say they wish employees would bring up issues and discuss solutions more often. Getting staff to give constructive feedback or raise issues can be challenging. It may take trial and error to have workable systems in place. Planning forums for regular two-way communication with staff can be useful. Many staff report that meetings with leadership are intimidating or that leaders do not welcome their comments. The environment often doesn't feel safe for employees to share concerns or even positive updates. They are unsure what management wants to hear and sometimes feel uncomfortable speaking in front of other staff.
You may develop ideas of your own, but here are some suggestions:
- Management will need to create clear ways to solicit ideas, input, and requests for resources.
- For example, set the expectation that staff regularly share at staff meetings. They can take turns presenting concerns or celebrating successes. Encouraging staff to celebrate accomplishments can help avoid the perception of staff or unit meetings being complaint sessions.
- It's also important to create a process for staff to share concerns outside of these meetings, especially early on while teams are still building confidence and may not feel safe or comfortable speaking out loud. Secure lockboxes for anonymous suggestions can work if management pays careful consideration to the items submitted.
- Managers should consider all requests and input, being careful not to provide the answer to staff before considering all the options
- Assure everyone that they bring different skills to the table, all of which are valued.
- Time should be provided to actively seek input from everyone at the table or on the team.
3. Bowers N, Nolet K, Roberts E, et al. Implementing Change in Long-Term Care: A Practical Guide to Transformation. University of Wisconsin–Madison, School of Nursing; 2007.
Slide 19: Open Communication
Say:
In the following video, Sharon brings up a mistake with her nurse manager. Watch how Thomas encourages communication and information sharing.
PLAY VIDEO
Video 3.2 Open Communication
Ask:
Sharon was comfortable talking to her nurse manager who encouraged the communication and created a safe environment to share concerns. Would a nurse in your facility be able to bring up an issue with the nurse manager as well? Can you think of an example when you did or did not feel comfortable bringing up a concern? How did that make you feel?
Slide 20: Positive Reinforcement3
Say:
As staff demonstrate their empowerment, leaders should acknowledge the positive changes in staff behavior. Here are two things you can do to provide positive reinforcement to staff:
- Set a goal, and when that goal is reached, plan a pizza party. Celebrating when goals are met is crucial to keeping momentum and engagement in the project. Leaders should be invited to these celebrations as they can learn about project success, and staff members have the chance to share their contributions.
- Discuss project successes with higher levels in the organization. Invite staff members who presented during all-staff or unit meetings to share their stories with senior leaders and administrators.
Recognize that there will often be failures in addition to successes. Encourage staff to find the silver linings or the pearls of wisdom in these failures. In failure, you are given an opportunity to learn from your mistakes and continue to improve processes. By using the Learn From Defects tool, teams can get down to the root cause of the problem, allowing for more targeted improvement.
Ask:
Does your facility celebrate success? What are some examples?
Do:
Make a list of three team members to recognize and provide feedback.
Have they shown a willingness to try new things?
Did they develop a solution to a problem?
Do they show an exceptionally positive attitude with residents? With other team members?
Celebrate them!
3. Bowers N, Nolet K, Roberts E, et al. Implementing Change in Long-Term Care: A Practical Guide to Transformation. University of Wisconsin–Madison, School of Nursing; 2007.
Slide 21: Positive Reinforcement
Say:
In the following video, Sharon and Thomas speak with the director of nursing about Sharon's mistake in protocol.
PLAY VIDEO
Video 3.3 Positive Reinforcement
Ask:
Do you see elements of positive reinforcement in the way the director of nursing responds to Sharon?
Say:
Sharon's mistake is used as an opportunity to learn, and Sharon is encouraged to bring forward such mistakes that allow the facility to re-examine their procedure and the reason for the mistake
Slide 22: Confidence9
Say:
Teams should develop a strong sense of collaborative trust and confidence. This trust and confidence can be described as psychological safety, where team members feel safe interacting within the group.
Team members who promote psychological safety will—
- Invite input from all team members.
- Encourage team members to contribute.
- Promote active listening and learning from each other.
- Ensure all team members are accessible.
- Acknowledge the limits of current knowledge.
Confidence is the essential element that will allow staff to feel empowered in the work they are doing. Staff members who feel confident in their work, knowledge, and skills are more satisfied with their jobs.
9. CUSP Toolkit. Rockville, MD: Agency for Healthcare Research and Quality; December 2012.
Slide 23: Collaborative Trust and Confidence
Say:
In the following video, Sharon and Thomas speak again with the director of nursing about Sharon's mistake in protocol.
PLAY VIDEO
Video 3.4 Collaborative Trust and Confidence
Ask:
Do you see elements of psychological safety in the way the director of nursing responds to Sharon?
Slide 24: Just Culture8,9
Say:
The term "Just Culture" refers to a system of shared accountability in which health care organizations are accountable for the practices they've designed and for sustaining the safe choices they've made. Staff, in turn, are accountable for the choices they make to ensure their residents receive the highest quality of care possible. A Just Culture environment helps provide a foundation for staff empowerment.
Within the Just Culture model, five key elements contribute to improved outcomes.
Mission, values, and expectations
For an organization to be effective, it must first define its mission and articulate values and expectations that align with that mission. Perfection is not a productive expectation because it's unattainable. Rather, an organization should set improvement as a goal. Defining these expectations gives staff a clear understanding of how they fit into the organization and how they can contribute.
System design
Humans are not perfect and occasionally make mistakes, either through unintentional errors or risky behaviors. To achieve optimal outcomes, organizations must design systems that minimize risks. Forcing functions, checks, and redundancies are some features of systems intended to minimize errors. Creating a culture in which staff feel safe discussing errors and concerns will allow an organization to learn from these mistakes and refine systems to be safer in the future. Open communication and the ability to provide meaningful feedback are key elements for an empowered staff.
Behavioral choices
Managing human behavior is essential to achieving outcomes. It's important to reinforce behaviors that reduce risk and deter behaviors that increase risk.
Learning systems
By establishing learning systems, organizations can manage both systems and human behavior. The Staff Safety Assessment and Learn From Defects form in this toolkit are two communication tools that can be used to promote learning systems. Learning opportunities, including the development of skills, techniques and career development, will allow staff to feel more prepared and committed to their work.
Accountability and justice
Accountability in a Just Culture is about more than simply blaming a person whenever a resident is harmed. In a Just Culture, the quality of behavioral choices should be emphasized more than the outcome of the choices, which may or may not have resulted in harm. A nonpunitive response to error is important. All humans make mistakes, and it is important to differentiate between human error and at-risk behavior versus reckless behavior.
8. Griffith S. Just Culture, Healthcare Services Overview. Outcome Engineering; 2012.
9. CUSP Toolkit. Rockville, MD: Agency for Healthcare Research and Quality; December 2012.
Slide 25: A Just Culture
Say:
A system of Just Culture recognizes that people make mistakes. Sharon was able to bring her mistake to the nurse manager and the director of nursing, who recognized that this mistake was an opportunity to learn, and not an intentional harm on Sharon's part.
PLAY VIDEO
Video 3.5: Just Culture and Open Communication
Ask:
How would Sharon's mistake have been handled at your facility?
Slide 26: Barriers to Staff Empowerment10
Say:
Many barriers to staff empowerment need to be acknowledged and addressed based on your own facility experience. Lack of resources, poor teamwork, and high staff turnover are just a few examples you might experience in your facility.
Team leaders must both change the systems that undermine the team's vision and also remove obstacles to change. It's essential that team leaders remove as many barriers as possible. Some key ways to engage your senior leader include communicating data, obtaining consensus on the shared vision, and aligning project goals with the facility goals. For more details and strategies, refer to the Senior Leader Engagement module of this Long-Term Care Safety Toolkit.
Ask:
What barriers to staff empowerment do you anticipate in your facility?
How have barriers been addressed in other improvement projects?
How would you prioritize the order in which barriers need to be addressed?
10. TeamSTEPPS Long-Term Care Toolkit. Rockville, MD. Agency for Healthcare Research and Quality; October 2012.
Slide 27: Key Concepts Review
Say:
Empowerment of frontline staff contributes to lower staff turnover and higher job satisfaction, which then increases resident satisfaction and resident safety. The key factors in empowering staff include opportunities for growth, resources, information, support, and acknowledgment of staff contributions.
Slide 28: References
- Laschinger, HKS and Read, E. The influence of nursing unit empowerment and social capital on unit effectiveness and nurse perceptions of patient care quality. Journal of Nursing Administration. 2014;44(6):347-352.
- Brannon D, Mor V. Nurse aide empowerment strategies and staff stability: Effects on nursing home resident outcomes. The Gerontologist. 2005;45(3):309-317.
- Bowers N, Nolet K, Roberts E, et al. Implementing Change in Long-Term Care: A Practical Guide to Transformation. University of Wisconsin–Madison, School of Nursing; 2007.
- Cready C, Yeatts D, Gosdin M, et al. CNA empowerment: Effects On Job Performance And Work Attitudes. Journal of Gerontological Nursing. 2008;34(3):26-35.
- Harris-Kojetin L, Brannon D, Barry T, et al. Measuring Long-Term Care Work: A Guide to Selected Instruments To Examine Direct Care Worker Experiences and Outcomes. Washington, D.C.: U.S. Department of Health & Human Services, U.S. Department of Labor; 2005.
Slide 29: References
- Kolus K. Mather Pavilion – Staff Empowerment Yields Quality Improvement. Long-Term Living. 2010;59(9):20.
- Hamann DJ. Does Empowering Resident Families or Nursing Home Employees in Decision Making Improve Service Quality? Journal of Applied Gerontology. 2014;33(5):603-23
- Griffith S. Just Culture, Healthcare Services Overview. Outcome Engineering; 2012.
- CUSP Toolkit. Rockville, MD: Agency for Healthcare Research and Quality; December 2012.
- TeamSTEPPS Long-Term Care Toolkit. Rockville, MD. Agency for Healthcare Research and Quality; October 2012.



