Module 4: Teamwork and Communication
AHRQ Safety Program for Long-Term Care: HAIs/CAUTI
Slide 1: Module 4: Teamwork and Communication
Slide 2: Objectives
- Describe effective communication and teamwork.
- Describe why teamwork training and improved communication optimizes resident safety.
- List barriers, tools, and strategies to effective teamwork and communication.
- Describe selected teamwork and communication tools.
- Review solutions to teamwork and communication challenges.
Slide 3: Effective Teamwork and Communication1,2
Teamwork and communication training
- decreases medical errors,
- improves outcomes and
- improves satisfaction (e.g., Resident, Family and Staff), contributing to increased resident safety.
1. Fuqua RM. Long term care nurses' feelings on communication, teamwork and stress in long term care. Journal of Sociological Research. 2013;4(2):61.
2. Salas E, Frush K. Improving Patient Safety Through Teamwork And Team Training. Oxford: Oxford University Press; 2012.
Slide 4: What Is Effective Communication Among Staff?3
- Process by which needed information is exchanged between individuals, departments, or organizations.
- Information needed to keep residents safe should be received, understood as intended, and shared at the appropriate time.
Image: A facility staff team
3. TeamSTEPPS Long-Term Care Toolkit. Rockville, MD. Agency for Healthcare Research and Quality; October 2012.
Slide 5: Why Is Effective Communication Among Staff Important?4
- Contributes to resident safety, which depends on information being relayed to the whole team at the right time.
- Improves staff satisfaction and morale, potentially lessening staff turnover, which leads to better outcomes.
Image: Staff at a resident's bedside
4. CUSP Toolkit. Rockville, MD: Agency for Healthcare Research and Quality; December 2012.
Slide 6: Staff Communication
Image: Indicating a video on the slide
PLAY VIDEO:
Video 1.1: Staff Communication
Slide 7: Barriers, Tools and Strategies, and Outcomes for Communication
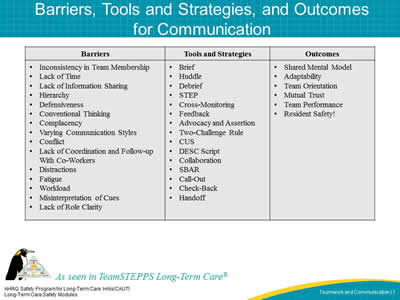
| Barriers | Tools and Strategies | Outcomes |
|---|---|---|
|
|
|
Slide 8: TeamSTEPPS Communication Concepts3
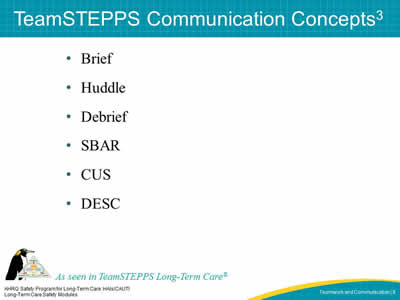
- Brief
- Huddle
- Debrief
- SBAR
- CUS
- DESC
3. TeamSTEPPS Long-Term Care Toolkit. Rockville, MD. Agency for Healthcare Research and Quality; October 2012.
Slide 9: For Planning – The Brief
- Facilitates clear and effective communication.
- Gets the team focused on the goals.
- Creates a sense of teamwork and collaboration.
- Fosters an environment where team members can and do speak up if they perceive a problem.
- Requires active participation by every member of the team.
- Sets the tone for the day and/or procedure.
Slide 10: Brief Checklist
During the brief, the team should address the following questions:
- Who is on the team?
- Do all members understand and agree with goals?
- Are roles and responsibilities understood?
- What is the care plan?
- What is the staff and availability throughout the shift?
- What is the workload among team members?
- What is the availability of resources?
Briefing video located at:
http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/longtermcare/video/03brief_ltc/index.html.
Image: Indicating a video on the slide
Slide 11: For Problem Solving – Huddle
- Ad hoc planning.
- Reestablish situation awareness.
- Reinforce plans already in place.
- Assess the need to adjust the plan.
Huddle video located at:
http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/longtermcare/video/04huddle_ltc/index.html.
Image: Indicating a video on the slide
Slide 12: For Process Improvement – Debrief
- Provides opportunity for an informal information exchange session.
- Designed to improve team performance and effectiveness.
- Reinforces positive behaviors demonstrated by the team.
Slide 13: Debrief Checklist
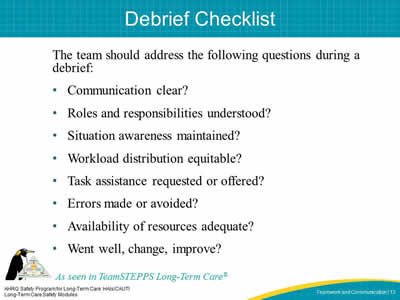
The team should address the following questions during a debrief:
- Communication clear?
- Roles and responsibilities understood?
- Situation awareness maintained?
- Workload distribution equitable?
- Task assistance requested or offered?
- Errors made or avoided?
- Availability of resources adequate?
- Went well, change, improve?
Slide 14: Communication Tools
Image: Indicating a video on the slide
PLAY VIDEO:
Video 1.4 Communication Tools
Slide 15: For Information Exchange – SBAR
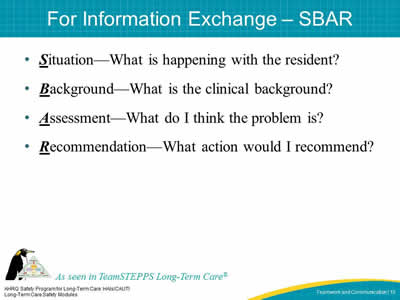
- Situation—What is happening with the resident?
- Background—What is the clinical background?
- Assessment—What do I think the problem is?
- Recommendation—What action would I recommend?
Slide 16: Practicing SBAR3
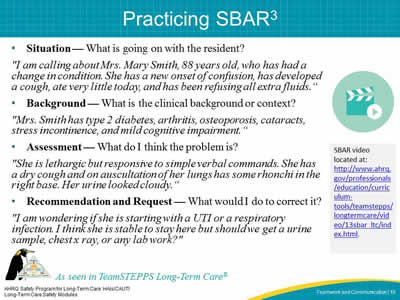
- Situation — What is going on with the resident?
"I am calling about Mrs. Mary Smith, 88 years old, who has had a change in condition. She has a new onset of confusion, has developed a cough, ate very little today, and has been refusing all extra fluids."
- Background — What is the clinical background or context?
"Mrs. Smith has type 2 diabetes, arthritis, osteoporosis, cataracts, stress incontinence, and mild cognitive impairment."
- Assessment — What do I think the problem is?
"She is lethargic but responsive to simple verbal commands. She has a dry cough and on auscultation of her lungs has some rhonchi in the right base. Her urine looked cloudy."
- Recommendation and Request — What would I do to correct it?
"I am wondering if she is starting with a UTI or a respiratory infection. I think she is stable to stay here but should we get a urine sample, chest x ray, or any lab work?"
SBAR video located at:
http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/longtermcare/video/13sbar_ltc/index.html.
Image: Indicating a video on the slide
3. TeamSTEPPS Long-Term Care Toolkit. Rockville, MD. Agency for Healthcare Research and Quality; October 2012.
Slide 17: For Information Transfer – Handoffs
- Includes the transfer of knowledge and responsibility.
- Designed to enhance information exchange at critical times.
- Maintains continuity of care despite changing caregivers and patients.
- Use I PASS the BATON as a handoff checklist.
Image: Two staff members reviewing a checklist
Slide 18: Handoff Tools
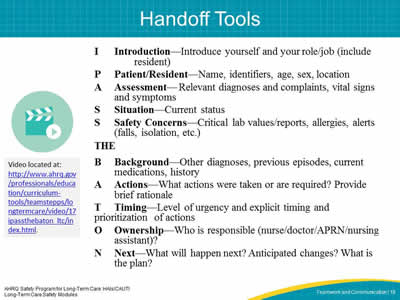
| I | Introduction—Introduce yourself and your role/job (include resident) |
| P | Patient/Resident—Name, identifiers, age, sex, location |
| A | Assessment—Relevant diagnoses and complaints, vital signs and symptoms |
| S | Situation—Current status |
| S | Safety Concerns—Critical lab values/reports, allergies, alerts (falls, isolation, etc.) |
THE
| B | Background—Other diagnoses, previous episodes, current medications, history |
| A | Actions—What actions were taken or are required? Provide brief rationale |
| T | Timing—Level of urgency and explicit timing and prioritization of actions |
| O | Ownership—Who is responsible (nurse/doctor/APRN/nursing assistant)? |
| N | Next—What will happen next? Anticipated changes? What is the plan? |
Video located at:
http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/longtermcare/video/17ipassthebaton_ltc/index.html.
Image: Indicating a video on the slide
Slide 19: Speaking Up Using Structured Language
- Use special words that indicate there is a problem.
- Both the sender and the receiver need to understand these words.
Slide 20: CUS
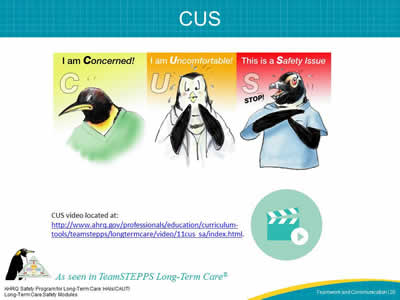
Image: CUS stands for I am concerned, I am uncomfortable, this is a safety issue.
CUS video located at:
http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/longtermcare/video/11cus_sa/index.html
Image: Indicating a video on the slide
Slide 21: DESC
- Describe the specific situation or behavior; provide concrete data.
- Express how the situation makes you feel/what your concerns are.
- Suggest alternatives and seek agreement.
- Consequences should be stated in terms of impact on established team goals.
DESC video located at:
http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/longtermcare/video/12descscript_ltc/index.html
Image: Indicating a video on the slide
Slide 22: Communication Strategies for Use With Residents and Family Members
Slide 23: Why Is It Important?

- Positively affect outcomes, perceptions of quality, and resident safety.
- Residents are more likely to experience higher levels of satisfaction and follow care plans.
- Leads to better clinical outcomes.
Image: Staff and a resident in a wheelchair
Slide 24: What Is Effective Communication Between Staff and Residents and Family?
- Complete, clear, brief, and timely.
- No jargon: using language the residents/families can understand.
- Making sure they truly understand what is being communicated to them.
Image: Staff at a resident's bedside
Slide 25: Communication and Engaging the Family
Image: Indicating a video on the slide
PLAY VIDEO:
Video 1.2 Communication and Engaging the Family
Slide 26: Addressing Challenges

- Residents who are impaired in some way
- Hard of hearing.
- Dementia.
- Language differences.
- Family members not available
- Logistical challenges.
- Frequency of visitation.
- Language differences.
Image: A resident in a wheelchair
Slide 27: Barriers to Speaking Up for Staff, Residents, and Families
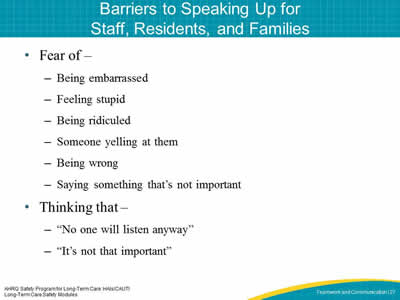
- Fear of –
- Being embarrassed.
- Feeling stupid.
- Being ridiculed.
- Someone yelling at them.
- Being wrong.
- Saying something that's not important.
- Thinking that –
- "No one will listen anyway"
- "It's not that important"
Slide 28: Communicating Adverse Events
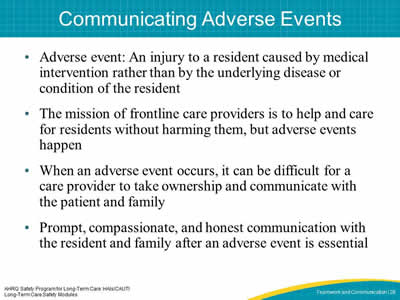
- Adverse event: An injury to a resident caused by medical intervention rather than by the underlying disease or condition of the resident.
- The mission of frontline care providers is to help and care for residents without harming them, but adverse events happen.
- When an adverse event occurs, it can be difficult for a care provider to take ownership and communicate with the patient and family.
- Prompt, compassionate, and honest communication with the resident and family after an adverse event is essential.
Slide 29: Disclosure and Apology for Unexpected Adverse Outcomes
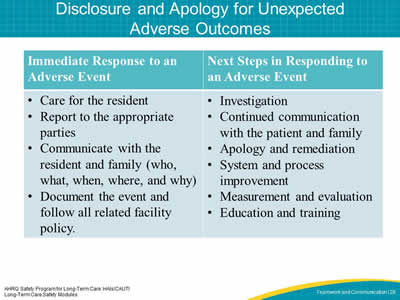
| Immediate Response to an Adverse Event | Next Steps in Responding to an Adverse Event |
|---|---|
|
|
Slide 30: How To Communicate About An Adverse Event
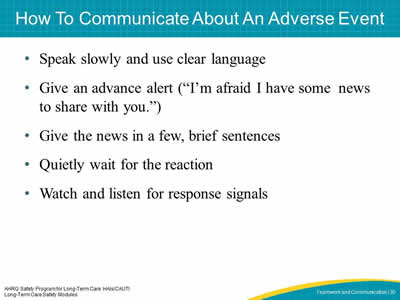
- Speak slowly and use clear language.
- Give an advance alert ("I'm afraid I have some news to share with you.").
- Give the news in a few, brief sentences.
- Quietly wait for the reaction.
- Watch and listen for response signals.
Slide 31: Communication in Action
Image: Indicating a video on the slide
PLAY VIDEO:
Video 1.3 Communication in Action
Slide 32: Key Concepts Review
- Effective communication involves sending, recurring, verifying, and validating techniques.
- Using tools, such as TeamSTEPPS, can improve communication and teamwork with staff, residents, and residents' families.
- Effective teamwork and communication decreases medical errors, improves outcomes and improves satisfaction for staff, residents and resident's families.
- Improved communication and teamwork contributes to resident safety.
Slide 33: References
- Fuqua RM. Long term care nurses' feelings on communication, teamwork and stress in long term care. Journal of Sociological Research. 2013;4(2):61.
- Salas E, Frush K. Improving Patient Safety Through Teamwork And Team Training. Oxford: Oxford University Press; 2012.
- TeamSTEPPS Long-Term Care Toolkit. Rockville, MD. Agency for Healthcare Research and Quality; October 2012.
- CUSP Toolkit. Rockville, MD: Agency for Healthcare Research and Quality; December 2012.



