The Four Es of Early Mobility: Slide Presentation
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: AHRQ Safety Program for Mechanically Ventilated Patients
The Four Es of Early Mobility
Slide 2: Learning Objectives
After this session, you will be able to—
- List the four Es from TRIP framework (engage, educate, execute, and evaluate).
- Apply each "E" intervention to early mobility (EM).
Slide 3: Translating Research Into Practice1
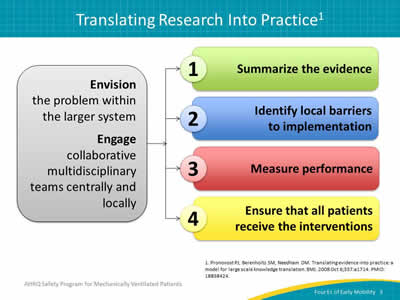
Image: Graphic displaying TRIP framework:
Envision the problem within the larger framework.
Engage collaborative multidisciplinary teams centrally and locally.
- Summarize evidence.
- Identify local barriers.
- Measure performance.
- Ensure all patients receive intervention.
1. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008 Oct 6;337:a1714. PMID: 18838424.
Slide 4: Summarize the Evidence1
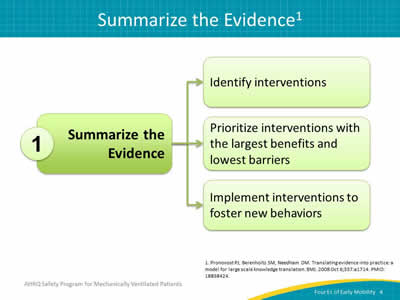
Image: Graphic displaying steps to Summarize the Evidence:
- Identify interventions.
- Prioritize interventions with the largest benefits and lowest barriers.
- Implement interventions to foster new behaviors.
1. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008 Oct 6;337:a1714. PMID: 18838424.
Slide 5: Identify Local Barriers1
Image: Graphic displaying steps to Identify Local Barriers:
- Observe staff performing care delivery tasks.
- Walk the process to identify defects at each step.
- Solicit feedback from all stakeholders.
- Identify potential gains or losses.
1. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008 Oct 6;337:a1714. PMID: 18838424.
Slide 6: What Are Your Barriers?2
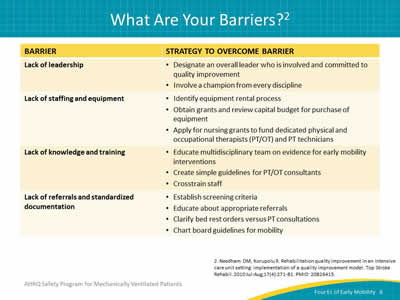
Lack of leadership:
- Designate an overall leader who is involved and committed to quality improvement.
- Involve a champion from every discipline.
Lack of staffing and equipment:
- Identify equipment rental process.
- Obtain grants and review capital budget for purchase of equipment.
- Apply for nursing grants to fund dedicated physical and occupational therapists (PT/OT) and PT technicians.
Lack of knowledge and training:
- Educate multidisciplinary team on evidence for early mobility interventions.
- Create simple guidelines for PT/OT consultants.
- Crosstrain staff.
Lack of referrals and standardized documentation:
- Establish screening criteria.
- Educate about appropriate referrals.
- Clarify bed rest orders versus PT consultations.
- Chart board guidelines for mobility.
2. Needham DM, Korupolu R. Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil 2010 Jul-Aug;17(4):271-81. PMID: 20826415.
Slide 7: What Are Your Barriers?2
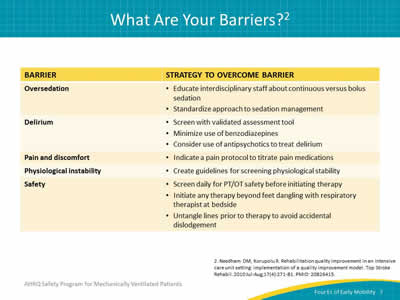
Oversedation:
- Educate interdisciplinary staff about continuous versus bolus sedation.
- Standardize approach to sedation management.
Delirium:
- Screen with validated assessment tool.
- Minimize use of benzodiazepines.
- Consider use of antipsychotics to treat delirium.
Pain and discomfort:
- Indicate a pain protocol to titrate pain medications.
Physiological instability:
- Create guidelines for screening physiological stability.
Safety:
- Screen daily for PT/OT safety before initiating therapy.
- Initiate any therapy beyond feet dangling with respiratory therapist at bedside.
- Untangle lines prior to therapy to avoid accidental dislodgement.
2. Needham DM, Korupolu R. Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil 2010 Jul-Aug;17(4):271-81. PMID: 20826415.
Slide 8: Measure Performance1
Image: Graphic displaying steps to Measure Performance:
- Select process and/or outcome measures.
- Develop and pilot test measures.
- Measure baseline performance.
1. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008 Oct 6;337:a1714. PMID: 18838424.
Slide 9: Ensure All Patients Receive the Evidence (Four Es)1
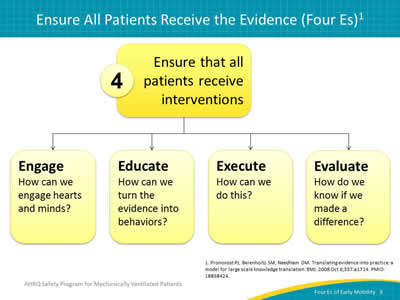
Image: Graphic displaying steps to Ensure that all patients receive interventions:
Engage: How can we engage hearts and minds?
Educate: How can we turn the evidence into behaviors?
Execute: How can we do this?
Evaluate: How do we know if we made a difference?
1. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008 Oct 6;337:a1714. PMID: 18838424.
Slide 10: Four Es of Early Mobility
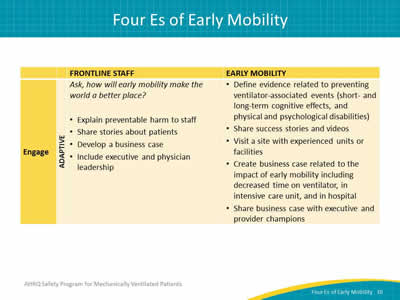
Category: Engage (Adaptive)
Frontline Staff:
Ask, how will early mobility make the world a better place?
- Explain preventable harm to staff.
- Share stories about patients.
- Develop a business case.
- Include executive and physician leadership.
Early Mobility:
- Define evidence related to preventing ventilator-associated events (short- and long-term cognitive effects, and physical and psychological disabilities).
- Share success stories and videos.
- Visit a site with experienced units or facilities.
- Create business case related to the impact of early mobility including decreased time on ventilator, in intensive care unit, and in hospital.
- Share business case with executive and provider champions.
Slide 11: Four Es of Early Mobility
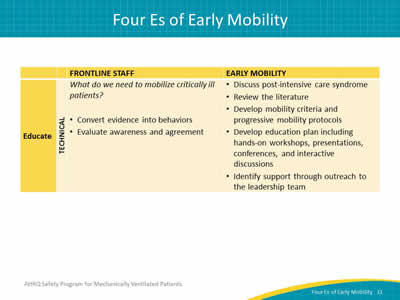
Category: Educate (Technical)
Frontline Staff:
What do we need to mobilize critically ill patients?
- Convert evidence into behaviors.
- Evaluate awareness and agreement.
Early Mobility:
- Discuss post-intensive care syndrome.
- Review the literature.
- Develop mobility criteria and progressive mobility protocols.
- Develop education plan including hands-on workshops, presentations, conferences, and interactive discussions.
- Identify support through outreach to the leadership team.
Slide 12: Four Es of Early Mobility
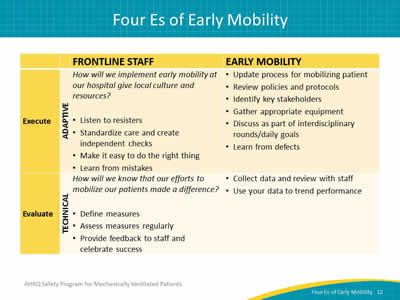
Category: Execute (Adaptive)
Frontline Staff:
How will we implement early mobility at our hospital give local culture and resources?
- Listen to resisters.
- Standardize care and create independent checks.
- Make it easy to do the right thing.
- Learn from mistakes.
Early Mobility:
- Update process for mobilizing patient.
- Review policies and protocols.
- Identify key stakeholders.
- Gather appropriate equipment.
- Discuss as part of interdisciplinary rounds/daily goals.
- Learn from defects.
Category: Evaluate (Technical)
Frontline Staff:
How will we know that our efforts to mobilize our patients made a difference?
- Define measures.
- Assess measures regularly.
- Provide feedback to staff and celebrate success.
Early Mobility:
- Collect data and review with staff.
- Use your data to trend performance.
Slide 13: Engage and Educate Frequently
- Share at multidisciplinary safety program meetings.
- Discuss at staff meetings every 6 weeks.
- Present at board meetings.
- Clarify expectations at daily huddles.
- Reinforce with email.
- Publish newsletter.
- Post on bulletin boards.
- Talk with staff while collecting data.
Slide 14: Engage All Staff
- Sitters/Observers.
- Clinical Technicians/ Nursing Assistants:
- Ambulate.
- Turn.
- Range of motion.
- Document.
- Ancillary Personnel.
Slide 15: Engage—Family Resources
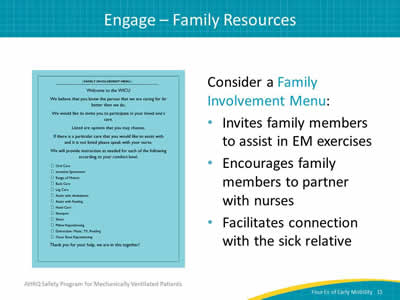
Consider a Family Involvement Menu:
- Invites family members to assist in EM exercises.
- Encourages family members to partner with nurses.
- Facilitates connection with the sick relative.
Image: A Family Involvement Menu.
Slide 16: Educate: Turn Evidence Into Behaviors
- Define and approve mobilization readiness criteria.
- Develop early/progressive mobility protocols and guidelines.
- Review the literature.
- Develop education plan including hands-on workshops, presentations, conferences, and interactive discussions.
- Identify support through outreach to the leadership team.
Slide 17: Readiness Assessment: Other Considerations
- Patient factors:
- Sedation level.
- Breathing support for EM interventions.
- Femoral lines.
- Presence of lines, drains, catheters.
- Other factors:
- The right equipment.
- Sufficient staffing/multidisciplinary focus.
Slide 18: Execute: Make It Easy To Do the Right Thing
- What is the process for mobilizing a patient?
- Is there a policy on the unit?
- Who should be involved?
- Do we have all the equipment?
- Discuss as part of interdisciplinary rounds/daily goals.
- Add mobility level to report sheet and nursing handoff.
Slide 19: Early Progressive Mobility Protocol
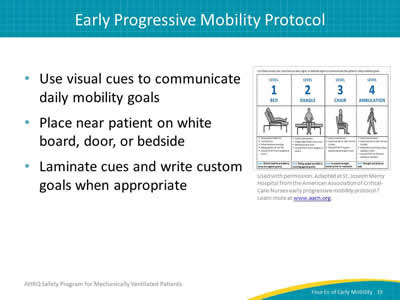
- Use visual cues to communicate daily mobility goals.
- Place near patient on white board, door, or bedside.
- Laminate cues and write custom goals when appropriate.
Image: Visual cues chart for an early mobility protocol.
Used with permission. Adapted at St. Joseph Mercy Hospital from the American Association of Critical-Care Nurses early progressive mobility protocol.3 Learn more at www.aacn.org.
3. Early Progressive Mobility Protocol. Aliso Viejo, CA: American Association of Critical-Care Nurses. April 2013. http://www.aacn.org/wd/practice/docs/tool%20kits/early-progressive-mobility-protocol.pdf. Accessed June 14, 2016.
Slide 20: Sample Early Mobility Protocol4
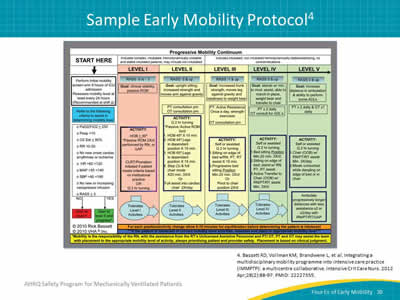
Image: Progressive mobility continuum chart.
4. Bassett RD, Vollman KM, Brandwene L, et al. Integrating a multidisciplinary mobility programme into intensive care practice (IMMPTP): a multicentre collaborative. Intensive Crit Care Nurs 2012 Apr;28(2):88-97. PMID: 22227355.
Slide 21: Evaluate: Measure Your Success
- Collect process measures data.
- Review at monthly safety program meetings.
- Post prominently for frontline staff.
- Use your data to trend performance.
Slide 22: Daily Early Mobility Measures Form
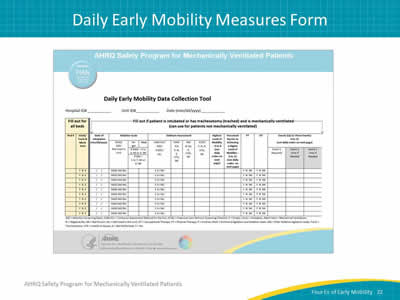
Image: Daily Early Mobility Data Collection Tool.
Slide 23: Daily Early Mobility Measures Guide
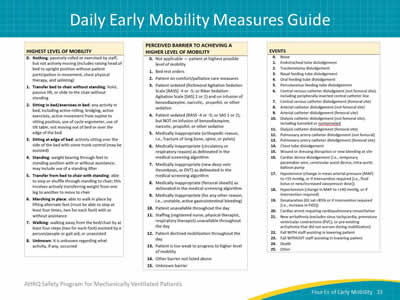
Image: Second page of the Daily Early Mobility Data Collection Tool.
Slide 24: Highest Level of Mobility
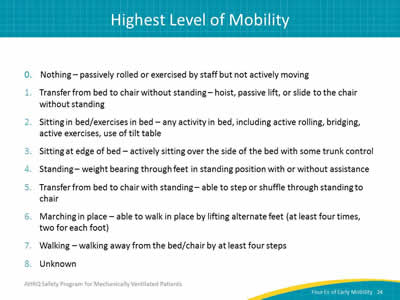
- Nothing—passively rolled or exercised by staff but not actively moving.
- Transfer from bed to chair without standing—hoist, passive lift, or slide to the chair without standing.
- Sitting in bed/exercises in bed—any activity in bed, including active rolling, bridging, active exercises, use of tilt table.
- Sitting at edge of bed—actively sitting over the side of the bed with some trunk control.
- Standing—weight bearing through feet in standing position with or without assistance.
- Transfer from bed to chair with standing—able to step or shuffle through standing to chair.
- Marching in place—able to walk in place by lifting alternate feet (at least four times, two for each foot).
- Walking—walking away from the bed/chair by at least four steps.
- Unknown.
Slide 25: Perceived Barriers
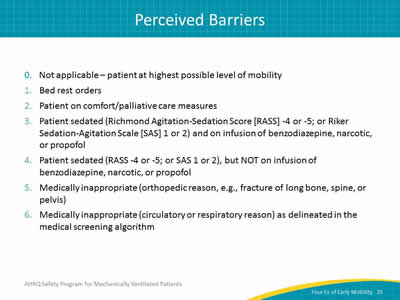
- Not applicable—patient at highest possible level of mobility.
- Bed rest orders.
- Patient on comfort/palliative care measures.
- Patient sedated (Richmond Agitation-Sedation Score [RASS] -4 or -5; or Riker Sedation-Agitation Scale [SAS] 1 or 2) and on infusion of benzodiazepine, narcotic, or propofol.
- Patient sedated (RASS -4 or -5; or SAS 1 or 2), but NOT on infusion of benzodiazepine, narcotic, or propofol.
- Medically inappropriate (orthopedic reason, e.g., fracture of long bone, spine, or pelvis).
- Medically inappropriate (circulatory or respiratory reason) as delineated in the medical screening algorithm.
Slide 26: Perceived Barriers
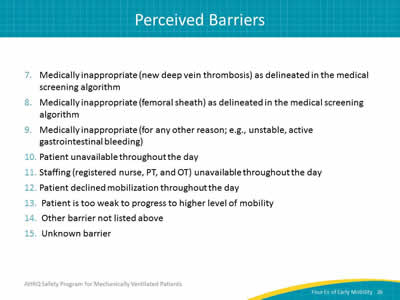
- Medically inappropriate (new deep vein thrombosis) as delineated in the medical screening algorithm.
- Medically inappropriate (femoral sheath) as delineated in the medical screening algorithm.
- Medically inappropriate (for any other reason; e.g., unstable, active gastrointestinal bleeding).
- Patient unavailable throughout the day.
- Staffing (registered nurse, PT, and OT) unavailable throughout the day.
- Patient declined mobilization throughout the day.
- Patient is too weak to progress to higher level of mobility.
- Other barrier not listed above.
- Unknown barrier.
Slide 27: Adverse Events During Mobilization
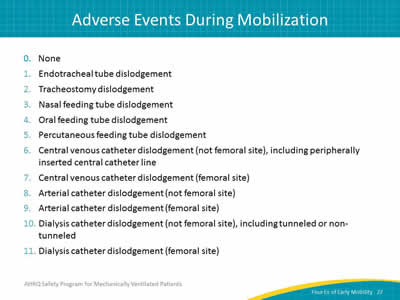
- None.
- Endotracheal tube dislodgement.
- Tracheostomy dislodgement.
- Nasal feeding tube dislodgement.
- Oral feeding tube dislodgement.
- Percutaneous feeding tube dislodgement.
- Central venous catheter dislodgement (not femoral site), including peripherally inserted central catheter line.
- Central venous catheter dislodgement (femoral site).
- Arterial catheter dislodgement (not femoral site).
- Arterial catheter dislodgement (femoral site).
- Dialysis catheter dislodgement (not femoral site), including tunneled or non-tunneled.
- Dialysis catheter dislodgement (femoral site).
Slide 28: Summary
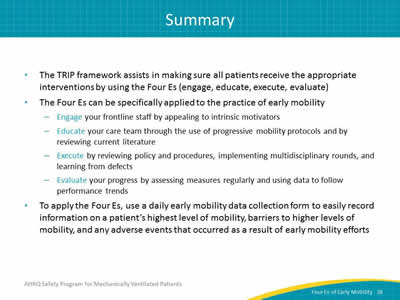
- The TRIP framework assists in making sure all patients receive the appropriate interventions by using the Four Es (engage, educate, execute, evaluate).
- The Four Es can be specifically applied to the practice of early mobility:
- Engage your frontline staff by appealing to intrinsic motivators.
- Educate your care team through the use of progressive mobility protocols and by reviewing current literature.
- Execute by reviewing policy and procedures, implementing multidisciplinary rounds, and learning from defects.
- Evaluate your progress by assessing measures regularly and using data to follow performance trends.
- To apply the Four Es, use a daily early mobility data collection form to easily record information on a patient’s highest level of mobility, barriers to higher levels of mobility, and any adverse events that occurred as a result of early mobility efforts.
Slide 29: References
1. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008 Oct 6;337:a1714. PMID: 18838424.
2. Needham DM, Korupolu R. Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil 2010 Jul-Aug;17(4):271-81. PMID: 20826415.
3. Early Progressive Mobility Protocol. Aliso Viejo, CA: American Association of Critical-Care Nurses. April 2013. http://www.aacn.org/wd/practice/docs/tool%20kits/early-progressive-mobility-protocol.pdf. Accessed June 14, 2016.
4. Bassett RD, Vollman KM, Brandwene L, et al. Integrating a multidisciplinary mobility programme into intensive care practice (IMMPTP): a multicentre collaborative. Intensive Crit Care Nurs 2012 Apr;28(2):88-97. PMID: 22227355.



