Measure Descriptions for Daily Early Mobility: Facilitator Guide
AHRQ Safety Program for Mechanically Ventilated Patients
Slide 1: Measure Descriptions for Daily Early Mobility
Say:
In this module, you will learn about the data measures you will use to evaluate early mobility process and outcome measures in your unit.
Slide 2: Learning Objectives
Say:
After this session, you will be able to collect and enter daily early mobility data using the Daily Early Mobility Data Collection Tool, understand the definitions of the data elements, and locate the necessary data elements.
Slide 3: Daily Early Mobility: Key Interventions
Ask:
What are the key interventions involved in implementing a daily early mobility protocol?
Say:
The Society of Critical Care Medicine’s 2013 Pain, Agitation, and Delirium Guidelines are clinical practice guidelines for the sustained use of sedatives and analgesics in critically ill patients. The key interventions listed here are in line with those guidelines. These recommendations begin with using a multidisciplinary, coordinated approach to managing pain, agitation, and delirium to improve patient outcomes. The second key intervention is interrupting sedation daily and minimizing sedative use in order to promote active participation in early mobility activities. The next intervention is performing structured assessments of sedation and delirium using validated scales. This allows physicians and other members of the care team to target appropriate treatment strategies. Fourth, screening every day for the highest level of mobility achieved by your patients, and finally, employing a nurse-driven protocol to achieve the highest level of mobility.
Slide 4: Data Collection

Say:
Collecting the data for early mobility can be a significant time commitment as well as require a substantial amount of manpower. However, for early mobility in particular, this data can not only be used to drive quality improvement efforts, but can also be used for quality improvement process development. Having this data at your disposal will provide quantifiable measures of care practices that assist in guiding conversations about improving patient safely. This information can also be used to help justify the necessary human, financial, and equipment resources.
Slide 5: Daily Early Mobility Data Collection Tool
Say:
The Daily Early Mobility Data Collection Tool is a resource you can use to collect information on your early mobility measures. It includes information about when the patient was intubated, which sedation scale your unit uses, the results of sedation scales performed, the delirium assessment scale your unit uses and the results of those assessments, the highest level of your patients’ mobility and perceived barriers to meeting a higher level of mobility, whether your patients were evaluated by a physical or occupational therapist, and finally, whether any adverse events associated with mobilization occurred and, if so, what types of events occurred.
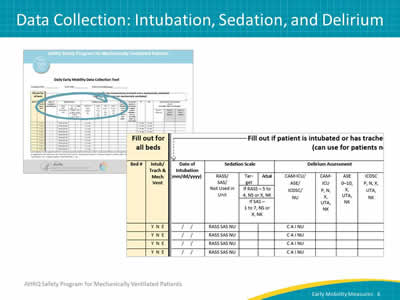
Slide 6: Data Collection: Intubation, Sedation, and Delirium
Say:
The first half of the data collection tool focuses on intubation and the assessment of sedation and delirium.
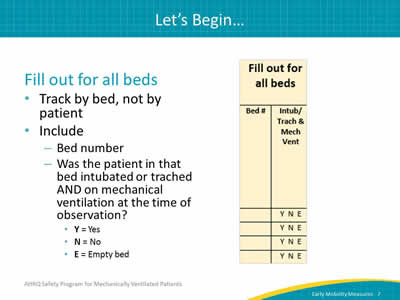
Slide 7: Let’s Begin
Say:
The early mobility measures are tracked by bed, and not by a specific patient. It is most useful to track all beds in the unit, whether they are filled or not. Begin by filling out the bed number and indicating whether the patient in that bed was ventilated through intubation or through a tracheostomy tube (typically referred to as "trached") AND was on mechanical ventilation at the time of observation. The codes you will use are listed on the collection tool itself: use the Y code if the patient is intubated or trached AND on mechanical ventilation, use the N code if the patient is NOT, and use E if the bed is empty.
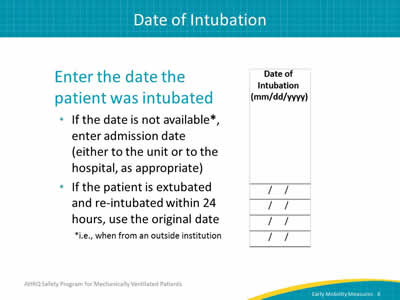
Slide 8: Date of Intubation
Say:
The next field is the date of intubation. In this field, you enter the date that the patient was intubated.
Ask:
What if that information is not available, such as when a patient is transferred from an outside institution?
Say:
If that date is not available, enter the admission date to either the unit or the hospital as appropriate.
Ask:
What if the patient has been extubated and reintubated? Which date should be used?
Say:
If the patient has been extubated and reintubated within the previous 24 hours, use the date of the original intubation. If the patient was reintubated after 24 hours of extubation, use the date of the most recent intubation.
Slide 9: Sedation Scale
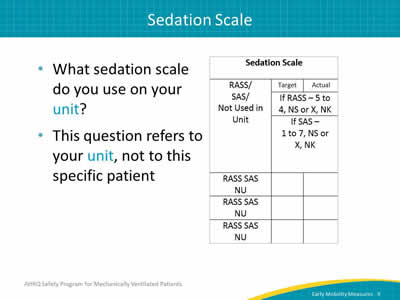
Say:
This field is for recording which sedation scale is used on your unit. This question specifically refers to your unit and not to the specific patient in the bed being observed.
Slide 10: Sedation Scale
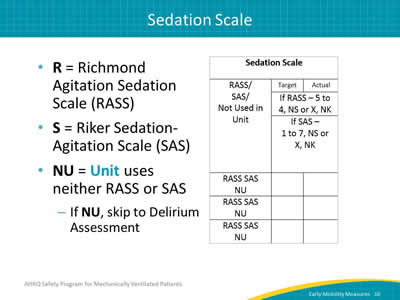
Say:
While the majority of units will likely use the Richmond Agitation Sedation Scale, RASS, or the Riker Sedation-Agitation Scale, SAS, some units may not employ either of these scales or do not use a sedation scale at all.
If you're not using either the RASS or the SAS, then enter the code "NU" for "not used" and move on to the field for Delirium Assessment.
Slide 11: Sedation Scale
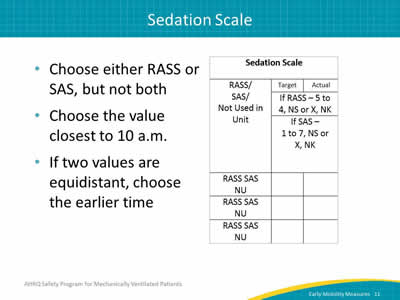
Say:
For units that do employ either RASS or SAS, first select which scale. Since RASS and SAS are documented similarly, we can go over them at the same time.
With respect to timing of the measurement, it’s recommended to choose the value closest to 10 a.m. because this is usually when rounds occur and when it will be discussed among all of the providers. If the assessment was performed more than once but the two closest are equidistant from 10 a.m. (e.g., one at 6 a.m. and one at 2 p.m.), choose the earlier time.
Slide 12: Sedation Scale: Target RASS or SAS
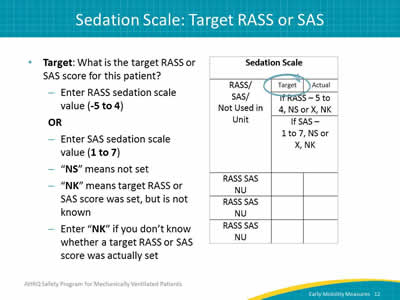
Say:
This field is where you record the target score for your patient. If using RASS, this score is recorded as a value between -5 and 4. If using SAS, the score is recorded as a value between 1 and 7.
If you set a target RASS or SAS, enter the target score in the corresponding column. If a target was not set, then choose NS for "not set."
Ask:
What if the target score is unknown?
Say:
There are two scenarios where you will choose NK for "not known." The first is if you know the target was set but you do not know the target value. Perhaps it was set by a coworker but you have no way of finding out what it is. The other scenario is if you do not know whether a target score was set.
Based on the Joint Commission’s recommendations, the target score must be set by a physician. However, as improving care for these patients involves an interdisciplinary approach, consider suggesting that a physician write the order for your target score, but encourage the team to discuss what they feel would be an appropriate score. This conversation could typically take place during rounds.
Slide 13: Sedation Scale: Actual RASS or SAS
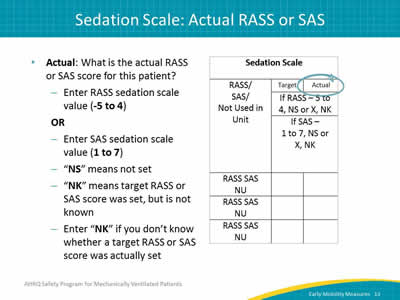
Say:
Once the target score has been entered for either RASS or SAS, you will also enter an actual score. Again, you enter a RASS value from -5 to 4 or a SAS value from 1 to 7. If you did not score an actual RASS or SAS level, then you would choose X. If you do not know the actual score, or if you do not know if there was an actual score, then you choose NK.
Slide 14: Delirium Assessment
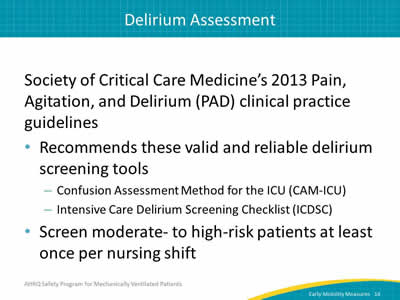
Say:
The second data measure we will focus on is the Delirium Assessment. The Society of Critical Care Medicine's or SCCM’s 2013 Pain, Agitation, and Delirium Clinical Practice Guidelines recommend the Confusion Assessment Method for the ICU, CAM-ICU, and Intensive Care Delirium Screening Checklist, ICDSC, as valid and reliable tools to screen for the presence or absence of delirium. The SCCM also recommends that moderate- to high-risk patients be screened at least once per nursing shift.
Slide 15: Delirium Assessment
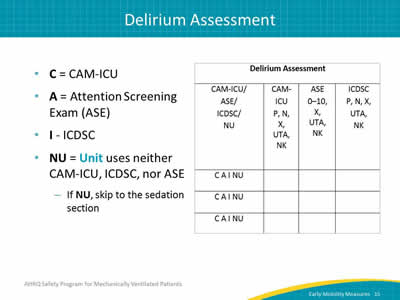
Say:
Here, the choices are between the CAM-ICU, ICDSC, and Attention Screening Exam or ASE. If neither assessment is used, select NU.
Slide 16: Delirium Assessment
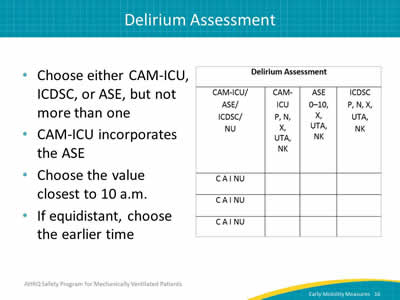
Say:
This data field records whether the patient is positive or negative for delirium. To do this, you will first need to indicate which assessment was used. Keep in mind the ASE is one aspect of the CAM-ICU, so of course if you complete a CAM-ICU, you will have also performed an ASE. For the purposes of clear data collection and analysis, record the most comprehensive test completed, so if the CAM-ICU is completed, choose CAM-ICU. If only the ASE is completed, choose ASE. As with documenting the RASS and SAS scores, when indicating what time the assessment was performed, it’s recommended to choose the value closest to 10 a.m. because this is usually when rounds occur and when it will be discussed among all of the providers. If the assessment was performed more than once but the two closest assessments are equidistant from 10 a.m. (e.g., one at 6 a.m. and one at 2 p.m.), choose the earlier time.
Slide 17: Delirium Assessment: CAM-ICU
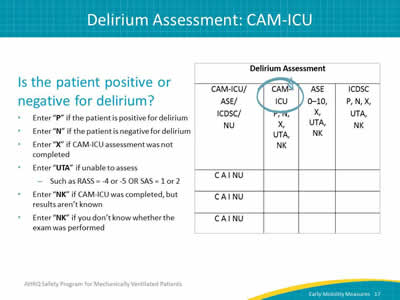
Say:
Now, let’s review how to complete these fields if the CAM-ICU or ICDSC is used to assess for delirium. In this column, you will indicate whether the patient was positive or negative for delirium according to the assessment. If the patient is positive, use the P code. If the patient is negative, use the N code. If you know a delirium assessment was not conducted, use the X code.
Ask:
What if the patient is heavily sedated and cannot be assessed?
Say:
If you're unable to assess delirium because the patient is heavily sedated, then you will put in UTA for "unable to assess." For example, if the patient has a RASS score of -5 or -4, or a SAS of 1 or 2, you would use UTA.
Ask:
What if the outcome of the assessment is unknown or if it’s unknown whether the assessment was completed in the first place?
Say:
If you do not know the results of the screening, or if you do not know whether the exam was performed, use the code NK to document "not known."
Slide 18: Delirium Assessment: ICDSC
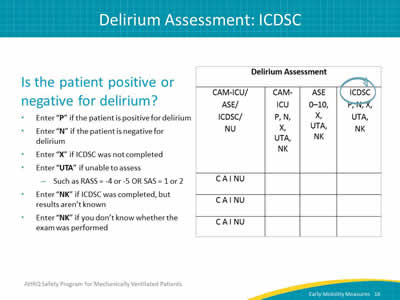
Say:
These fields should be completed identically to the fields for CAM-ICU. In this column, you will indicate whether the patient was positive or negative for delirium according to the assessment. If the delirium assessment is positive, use the P code. If the delirium assessment is negative, use the N code. If you know a delirium assessment was not conducted, use the X code.
Slide 19: Delirium Assessment: Attention Screening Exam
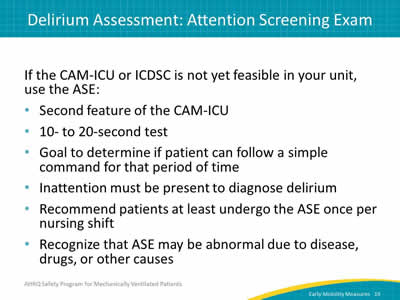
Say:
If you cannot do the CAM-ICU or ICDSC on your unit or if providers feel delirium screening is too time consuming, consider using just the ASE component once per shift. The ASE is actually a part of the CAM-ICU and takes just 10 to 20 seconds to complete. This assessment addresses inattention during a delirium diagnosis by determining if a patient is able to follow a simple command for a 20-second period of time.
Slide 20: Attention Screening Exam
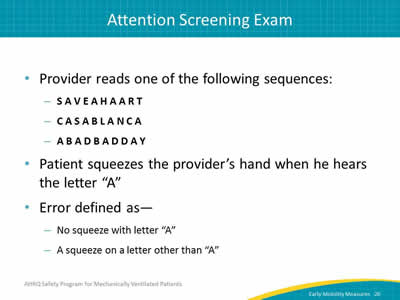
Say:
The Attention Screening Exam, as mentioned previously, determines if a patient can pay attention and follow a simple command for ten to twenty seconds. Inattention is a cardinal feature of delirium for diagnosis and the ASE provides a good barometer of the presence or absence of delirium.
Ask:
How is the ASE conducted?
Say:
To conduct the ASE, the provider reads one of the letter sequences shown on this slide. Read the sequence to the patient letter by letter. The patient is asked to squeeze the provider’s hand every time the patient hears the letter A, and the provider will count the number of errors made. For example, if the patient does not squeeze on an A, that would be an error. If a patient squeezes on a letter other than an A, that would also be an error.
Slide 21: Attention Screening Exam
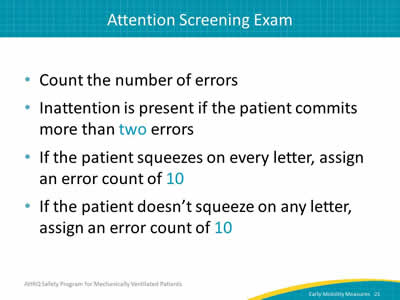
Say:
Inattention is considered to be present if the patient commits more than two errors. To determine the number of errors, count the number of times the patient does not squeeze when the letter A is spoken or if the patient squeezes on a letter that is not A. If the patient squeezes for every letter, assign an error count of 10 (even though the patient did squeeze correctly when the letter A was spoken) and if the patient doesn’t squeeze on any letter, an error count of 10 would be assigned then as well.
Slide 22: Attention Screening Exam
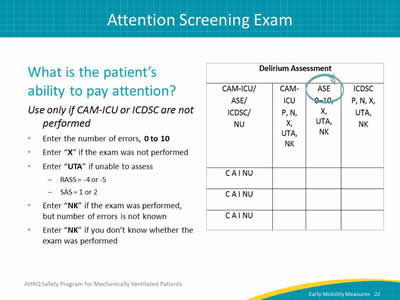
Say:
In the ASE column, record the number of errors counted during the assessment, again remembering that more than two errors indicates inattention. Mark X if the ASE was not completed as a standalone assessment. If your patient is considered to be substantially sedated, defined as having a -5 or -4 RASS or a SAS of 1 or 2, you would use UTA, or unable to assess. If the ASE was not performed, if you do not know whether it was performed at all, or if you do not know the number of errors, use the code NKT for "not known." Remember: only use the column for the ASE if the CAM-ICU was NOT performed.
Slide 23: Data Collection: Early Mobility Measures
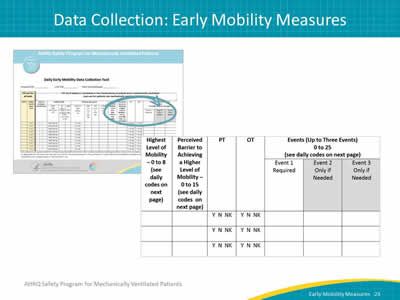
Say:
The second half of the data collection tool focuses on efforts to achieve early mobility.
Slide 24: Highest Level of Mobility
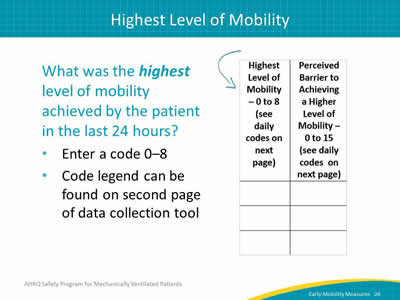
Say:
Start with the column documenting the highest level of early mobility.
Ask yourself, "What was the highest level of mobility achieved by a particular patient in the last 24 hours?" Then, enter the code that corresponds to a level of mobility from zero to 8. These code legends can be found on the second page of the Data Collection Tool.
Slide 25: Highest Level of Mobility
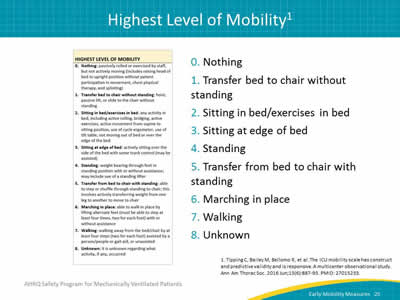
Say:
The scale to measure the highest level of a patient’s mobility has been adopted from a published and validated scale by Dr. Carol Hodgson and her colleagues. The scale itself has been consolidated to make it easier for the purpose of data collection. The scale lists mobility levels ranging from unable to achieve active mobility to walking, with or without assistance.
Slide 26: Perceived Barrier to Achieving Higher Mobility
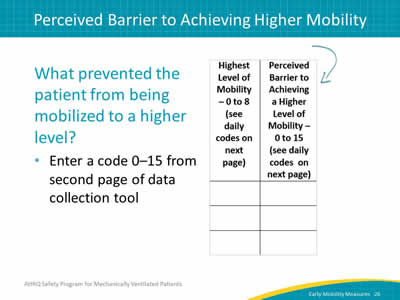
Say:
The next column is Perceived Barrier to Achieving a Higher Mobility. This important field can give your team a better idea of what barriers are preventing additional mobilization of your patients. Additionally, this field gives you the ability to document when a patient is already at the highest level of mobility the patient can achieve, which can be instrumental in determining whether your mobilization efforts are making a difference. Here, you will enter a code from zero to 15, based on the codes found on the second page of the Data Collection Tool.
Slide 27: Perceived Barrier Code Examples
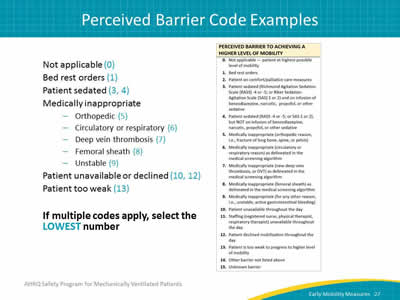
Ask:
What if there are several barriers that prevent a patient from being mobilized to a higher level?
Say:
This is an ordinal scale. If you are encountering several barriers, select the lowest number that corresponds to the barriers to early mobilization.
For example, if bed rest orders apply and the patient is medically inappropriate for being mobilized due to an orthopedic reason, then both the 1 and 5 codes apply. In this case, you would enter 1 in your Data Collection Tool.
Slide 28: Physical and Occupational Therapy
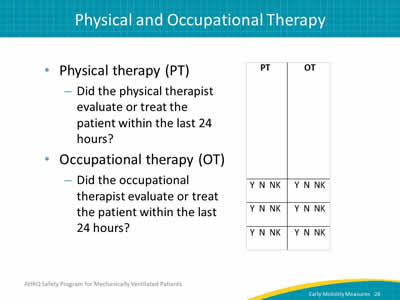
Say:
Next, we have two columns, where you can record whether a physical or occupational therapist evaluated or treated the patient within the last 24 hours. This does not mean that a physical or occupational therapist must be involved in your patient's care; for many smaller or academic hospitals this is not always practical. However, this may be useful information at some point.
Slide 29: Events
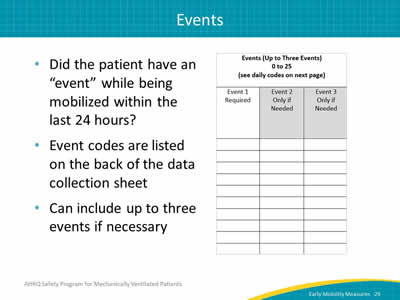
Say:
The next columns are designed to help track any adverse events that might have occurred while the patient was being mobilized. This field allows you to document up to three events if multiple events occurred.
Slide 30: Event Codes
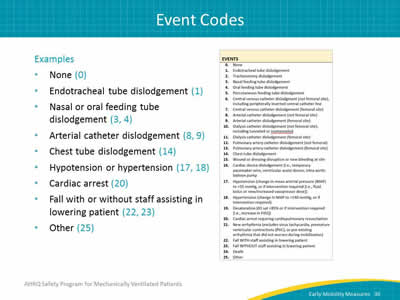
Say:
If no adverse events occurred, use "0" (the code for "none") to indicate that no adverse events took place. There are 25 event codes all together, ranging from endotracheal tube dislodgement to death.
Slide 31: Data Measures Guide
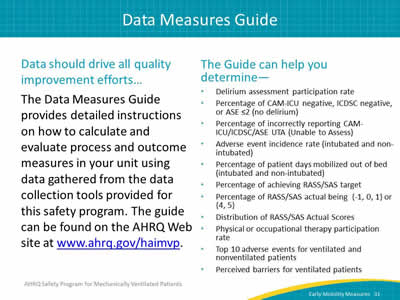
Ask:
How can we use the data we collect?
Say:
The Data Measures Guide provides detailed explanations for the measures used to evaluate the implementation of the interventions within the AHRQ Safety Program for Mechanically Ventilated Patients. It gives you a foundation for evaluating both process and outcome measures in your unit or hospital by providing detailed instructions and guidance on calculating metrics you can use to improve the safety of your patients.
From the information recorded on the Daily Early Mobility Collection Tool, you can use the Data Measures Guide to find out more than 10 different metrics, including your delirium assessment participation rate and the percentage of patients achieving their RASS or SAS target, as well as determine the top 10 adverse events for ventilated and nonventilated patients. Remember that collecting and analyzing these data points will give you a wealth of information that can be used to support the creation of actionable plans to improve quality in your unit. This data will help create a "feedback loop" where your successes can serve to inspire future success.
Slide 32: Questions?
Ask:
Are there any questions?
Slide 33: References